UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYBy :Dr Ali Moayid
2020-2021
Department of
Conservative Dentistry
5th YEARs
Periapical pathosisUNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Primary Acute Apical Periodontitis
The term “apical periodontitis” implies inflammation of the periapical tissues. When this first commences, there will not be a radiolucency as it takes some time for the bone (and possibly some of the tooth) to be resorbed to the extent where it is visible radiographically
Typical symptoms—the pain has only been present for a short time (e.g., a few days or less); the pain is usually quite severe; because the inflammation is confined within the hard bony tissues and the PDL where there is no space for the swelling, exudate, and so forth to expand pain to biting and pressure on the tooth; pain to touch the tooth—even with light pressure; may be pain due to acute irreversible pulpitis if present; occasionally may have pain due to acute reversible pulpitis.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
Clinical findings—may be caries, a restoration breaking down or a crack; severe pain to percussion; pain when pushing on the tooth; usually no response to pulp sensibility tests—unless acute reversible pulpitis or acute irreversible pulpitis in which case the tooth will respond to cold pulp testing which reproduces the thermal sensitivity pain that the patient will also complain of; sometimes the tooth is in traumatic occlusion
due to being extruded from its normal position as a result of the periapical inflammation being constrained by the hard bone structure that has not yet resorbed to create space.
Radiographic findings—caries may be seen if extensive enough; normal PDL space and lamina dura; a slightly widened PDL space may be evident if the tooth is extruded from its normal position; some cases may have evidence of previous endodontic treatment; occasionally may see a radiolucency within the tooth root indicating internal inflamma-
tory resorption.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Key findings for diagnosis—there are no radiographic periapical changes, the pain is recent and severe; there is pain when touching the tooth, with pressure and on percussion.
Distinguish from secondary acute apical periodontitis by the lack of radiographic signs of any periapical changes.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Distinguish from chronic apical periodontitis by the lack of radiographic signs of any periapical changes, plus the presence of pain and the tenderness to percussion.
Distinguish from a primary and secondary acute apical abscess by the lack of swelling.
Distinguish from a chronic apical abscess by the lack of a draining sinus.UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Secondary acute apical periodontitis occurs when there has been chronic apical periodontitis or a chronic apical abscess present for some time so there is also a periapical radiolucency .
Secondary acute apical periodontitis is usually a result of an imbalance occurring between the intra-canal infection and the host defence system whereby some bacteria and/or their endotoxins escape through the apical foramen and cause an acute exacerbation of the chronic inflammatory response that has been present for some time.
This process may occur on numerous occasions (e.g., patient reports that the pain “comes and goes.
The process is dynamic and the secondary acute apical periodonttis can return to being chronic apical periodontitis if the environmental conditions are suitable and the host defence response is adequate.
Secondary Acute Apical Periodontitis
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Typical symptoms—the pain has only been present for a short time (e.g., a few days or less); the pain is usually quite severe; pain to biting or pressure on the tooth; no thermal sensitivity.
Clinical findings—may be caries, a restoration breaking down or a crack; very tender to percussion; no response to pulp sensibility tests; may be tender to palpation.
Radiographic findings—caries may be seen if extensive enough; a periapical radiolucency is present—this indicates chronic apical periodontitis has been present for some time; some cases may have evidence of previous endodontic treatment; occasionally may see a
radiolucency within the tooth root indicating internal inflammatory resorption.
Key findings for diagnosis—there is a periapical radiolucency, the pain is recent and severe; pain with pressure and on percussion.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Distinguish from primary acute apical periodontitis by the presence of a periapical radiolucency.
Distinguish from chronic apical periodontitis by the pain and the tenderness to percussion.
Distinguish from a primary acute apical abscess by the lack of swelling.
Distinguish from a secondary acute apical abscess by the lack of swelling.
Distinguish from a chronic apical abscess by the lack of a draining sinus.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
Chronic Apical Periodontitis
After an initial period of primary acute apical periodontitis, and if the tooth has not been treated, the periapical inflammation can become chronic. After several months, Bone is resorbed to create space for the inflammatory reaction to occur so there are usually no, or only occasional mild symptoms .
Typical symptoms—usually no symptoms; the patient may report a history of occasional “awareness” of the tooth feeling different; the patient may report a history of previous pulp-related symptoms some time ago; the patient may report a history of previous endodontic treatment.
Clinical findings—may be caries, a restoration breaking down or a crack; the tooth is not tender to percussion but will sometimes feel “different” to percussion; no response to pulp sensibility tests.
Radiographic findings—caries may be seen if extensive enough; a periapical radiolucency will be present; some cases may have evidence of previous endodontic treatment; occasionally may see a radiolucency within the tooth root indicating internal inflammatory resorption.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Key findings for diagnosis—there is a periapical radiolucency and no pain or only occasional “awareness” of the tooth.
Distinguish from primary acute apical periodontitis by the presence of a periapical radiolucency.
Distinguish from secondary acute apical periodontitis bythe lack of symptoms.
Distinguish from a primary acute apical abscess by the lack of swelling and lack of symptoms.
Distinguish from a chronic apical abscess by the lack of a draining sinus.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
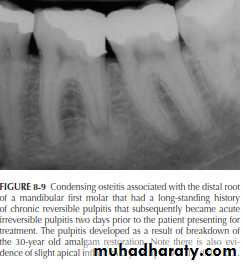
Condensing Osteitis
Condensing osteitis is a form of chronic apical periodontitis but it manifests as a radiopacity instead of a radolucency.
It is most commonly associated with teeth that have long-standing pulpitis—usually, or at least initially, chronic reversible pulpitis. Hence, it is essentially an extension of the inflammatory response that began in the pulp or it is an indication that the periapical tissues have been irritated for some time with the result that more bone is laid down rather than being resorbed. The chronic reversible pulpitis may have episodes of acute reversible pulpitis that may be the time when the patient presents for treatment. Alternatively, the chronic reversible pulpitis may develop into chronic irreversible pulpitis, acute irreversible pulpitis or pulp necrosis with infection.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Also, the root canal system may become pulpless and infected. The state of the pulp/root canal will depend on when the patient presents for treatment whereas the increased bone density that is evident radiographically may take many years to resolve and may not resolve at all. When the root canal
system becomes infected, a radiolucency will typically develop immediately adjacent to the root apex and this may be surrounded by the sclerotic bone of the condensing osteitis, thus appearing as both radiopacity and radiolucency.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
Typical symptoms—no symptoms from the periapical or periradicular tissues; no tenderness to percussion; any symptoms will be from the pulp—hence, symptoms depend
on the status of the pulp; usually associated with longstanding chronic reversible the chronic. the symptoms vary according to the stage of pulp disease.
Clinical findings—may be caries, a restoration breaking down or a crack; the tooth is not tender to percussion but may occasionally feel “different” to percussion; the tooth will
usually respond to pulp sensibility tests (the nature of the response depends on the state of the pulp) unless the pulp state has progressed to pulp necrosis, and so forth.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Radiographic findings—caries may be seen if extensive enough; the periapical region appears more radiopaque than the surrounding bone due to increased bone deposition (i.e., condensing osteitis); some cases may present later after the pulp has necrosed and the root canal system has become infected with various forms of apical periodontitis or apical abscesses—in these cases, some condensing osteitis may still be evident radio-
graphically and there may be a widened PDL space or a radiolucency surrounded by the denser bone of condensing osteitis.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Distinguish from primary acute apical periodontitis by the presence of the radiopacity and lack of symptoms.
Distinguish from secondary acute apical periodontitis by the presence of the radiopacity and lack of symptoms.
Distinguish from chronic apical periodontitis by the presence of the radiopacity although it should be noted that condensing osteitis is essentially a form of chronic apical periodontitis)
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
.
Distinguish from a primary acute apical abscess by the lack of swelling and lack of symptoms, and the presence of the radiopacity.
Distinguish from a secondary acute apical abscess by the lack of swelling and lack of symptoms, and the presence of the radiopacity.
Distinguish from a chronic apical abscess by the lack of a draining sinus and the presence of the radiopacity.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
An abscess is defined as a “localized collection of pus.” When this occurs in the early stages of the periapical disease process, there will not be a radiolucency as it takes some
time for the bone (and possibly some of the tooth) to be resorbed to the extent where it is visible radiographically (hence, an abscess in its early stages is called “primary acute apical abscess” and its key feature is the lack of a radiolucency, yet there is considerable pain.
Typical symptoms—the pain has only been present for a short time (e.g., a few days or less); the swelling has had rapid onset (e.g., hours, or less than one day); pus will be present; the pain is severe; pain to biting and pressure on the tooth; pain to touch the tooth—even with light pressure; occasionally the patient may complain of feeling unwell and having fever.
Clinical findings—may be caries, a restoration breaking down or a crack; swelling associated with the tooth;
Primary Acute Apical Abscess
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
severe pain to percussion; pain when pushing on the tooth; pain on palpation; no response to pulp sensibility tests; usually the tooth is in traumatic occlusion due to being extruded from its normal position; occasionally the patient may have fever, malaise and lymphadenopathy.
Radiographic findings—caries may be seen if extensive enough; normal PDL space and lamina dura; a slightly widened PDL space may be evident where there is no space for the pus and swelling to expand. if the tooth is extruded from its normal position; some cases may have evidence of previous endodontic treatment; occasionally may see a radiolucency within the tooth root indicating internal inflammatory resorption.
Key findings for diagnosis—there are no radiographic periapical changes, there is swelling present, the pain is recent and severe, and there is pain when touching the
tooth, with pressure and on percussion.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
Distinguish from primary acute apical periodontitis by the presence of the swelling and pus.
Distinguish from secondary acute apical periodontitis by the lack of periapical radiolucency, and the presence of the swelling and pus.
Distinguish from chronic apical periodontitis by the lack of periapical radiolucency, and the presence of pain, swelling tenderness to percussion, and pus.
Distinguish from a secondary acute apical abscess by the lack of periapical radiolucency.
Distinguish from a chronic apical abscess by the lack of a draining sinus and no periapical radiolucency.
231
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
A secondary acute apical abscess occurs when there has been chronic apical periodontitis or a chronic apical abscess present for some time so there is also a radiolucency
. A secondary acute apical abscess is usually a result of an imbalance occurring between the intra-canal infection and the host defense system whereby some bacteria and/or their endotoxins (or both) escape through the apical foramen and cause an acute exacerbation of the chronic inflammatory response that has been present for some time. The acute exacerbation will be in the form of a localized collection of pus (i.e., an abscess). It may also occur when the draining sinus of a chronic apical abscess closes or becomes blocked so the pus cannot drain.
Typical symptoms—the pain has only been present for a short time (e.g., a few days or less); the swelling has had rapid onset (e.g., hours, or less than one day); pus will be present; the pain is usually quite severe; pain to biting or pressure on the tooth; no thermal sensitivity; occasionally the patient may complain of feeling unwell and having fever.
Secondary Acute Apical Abscess
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Clinical findings—may be caries, a restoration breaking down or
a crack; the tooth is very tender to percussion; no response to
pulp sensibility tests; tender to palpation; occasionally the patient
may have fever, malaise and lymphadenopathy.
Radiographic findings—caries may be seen if extensive enough; there will be a periapical radiolucency present—indicates chronic apical periodontitis has been present for some time before the abscess developed; some cases may have evidence of previous endo-
dontic treatment; occasionally may see a radiolucency within the tooth root indicating internal inflammatory resorption.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Key findings for diagnosis—there is a periapical radiolucency, swelling is present, the pain is recent and severe, and there is pain when touching the tooth, with pressure and on percussion
.
Distinguish from primary acute apical periodontitis by the presence of a periapical radiolucency and the swelling.
Distinguish from secondary acute apical periodontitis by the presence of the swelling and if the patient has fever, malaise, and so forth
Distinguish from chronic apical periodontitis by the presence of swelling, pain, fever, and so forth.
Distinguish from a primary acute apical abscess by the presence of a periapical radiolucency.
Distinguish from a chronic apical abscess by the lack of a draining sinus and the presence of swelling and symptoms
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
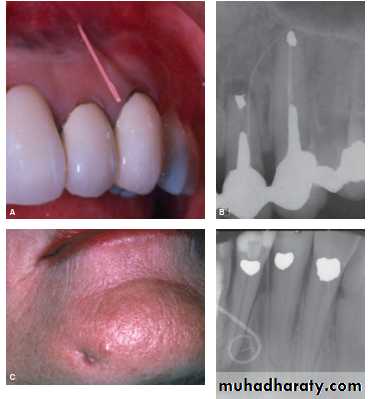
Chronic Apical Abscess
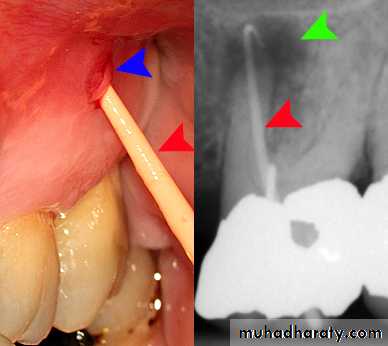
A chronic apical abscess is characterized by the presence of a draining sinus either intra-orally or extra-orally on the the condition may oscillate between being chronic
apical periodontitis and a chronic apical abscess.
Typical symptoms—usually there are no symptoms; some
patients may be aware of the presence of a draining
sinus (they may refer to it as a “gum boil,” “lump,”
“ulcer,” etc.); the draining sinus is usually intra-oral (on
the oral mucosa) but may be extra-oral (on the face);
the patient may report a history of occasional “aware-
ness” of the tooth feeling different; the patient may
report a history of previous pulp-related symptoms
some time ago; may have history of previous endodon-
tic treatment.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Clinical findings—may be caries, a restoration breaking
down or a crack; the tooth is not tender to percussion;
may feel “different” to percussion; no response to pulp
sensibility tests; draining sinus evident—intra-oral or
extra-oral; palpation or pressure on the tissues overly-
ing the periapical region may cause pus to exude from
the draining sinus; can often insert a gutta-percha point
into the draining sinus to trace it radiographically.
Radiographic findings—caries may be seen if extensive
enough; there is a periapical radiolucency present; a
gutta-percha point inserted into the draining sinus can
trace its origin to the infected tooth; some cases may
have evidence of previous endodontic treatment; occa-
sionally may see a radiolucency within the tooth root
indicating internal inflammatory resorption.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Key findings for diagnosis—there is a draining sinus, a periapical
radiolucency and no pain or only occasional “awareness.”
Distinguish from secondary acute apical periodontitis by the presence of the draining sinus and lack of symptoms.
Distinguish from chronic apical periodontitis by the presence of the draining sinus.
Distinguish from a secondary acute apical abscess by the presence of the draining sinus, and the lack of swelling and symptoms.
Distinguish from a foreign body reaction by the presence of the draining sinus and the lack of radiographic evidence of a foreign body (but some foreign bodies may not be radiopaque and therefore may not be evident radiographically.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
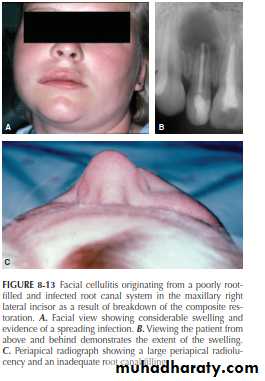
Facial Cellulitis
Facial cellulitis occurs when an infected root canal system
develops a periapical abscess (usually a secondary acute
apical abscess, although it could be a primary acute apical
abscess) and the infection spreads between the fascial planes of the muscles of the face, head, and/or neck (It is a spreading infection and it can be superficial or deep. In either case, it can be life-threatening if the resultant swelling restricts the airway. Patients with facial cellulitis require immediate and aggressive treatment—that is, not just oral antibiotic therapy but active dental treatment to remove the source of the bacteria. They often require hospitalisation
and even management in an intensive care unit to protect the airway and provide life support in severe cases.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Typical symptoms—facial swelling that is increasing in size—often rapidly; the swelling has had rapid onset (e.g., hours); the patient has considerable pain and discomfort; the pain has only been present for a short time (usually less than 24 hours); there is pain to biting or pressure on the tooth; no thermal sensitivity; the patient has fever and feels unwell.
Clinical findings—facial swelling is evident; may be caries, a restoration breaking down or a crack; very tender to percussion; no response to pulp sensibility tests; tender to palpation; the patient has fever, malaise and lymphadenopathy; severe cases may have airway involvement; typically also have localized signs of a secondary acute apical abscess as the abscess usually occurs before the infection spreads to become facial cellulitis.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Radiographic findings—caries may be seen if extensive enough;
there is a periapical radiolucency present indicates chronic apical
periodontitis has been present for some time before the abscess and facial cellulitis
developed; some cases may have evidence of previous endodontic treatment; occasionally may see a radiolucency within the tooth root indicating internal inflammatory resorption.
Key findings for diagnosis—there is facial swelling of rapid onset, the swelling is spreading, the patient has fever, feels unwell, has a periapical radiolucency, and pain with pressure and percussion.
Distinguish from primary acute apical periodontitis by the presence of a periapical radiolucency, facial swelling, fever, and malaise.
Distinguish from secondary acute apical periodontitis by the presence of facial swelling, fever, and malaise.
Distinguish from chronic apical periodontitis by the pain, facial swelling and the tenderness to percussion.
Distinguish from a primary acute apical abscess by the presence of a periapical radiolucency, facial swelling, fever, and malaise.
Distinguish from a secondary acute apical abscess by the swelling spreading throughout the face, and so forth.
Distinguish from a chronic apical abscess by the lack of a draining sinus and the presence of pain and facial swelling.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
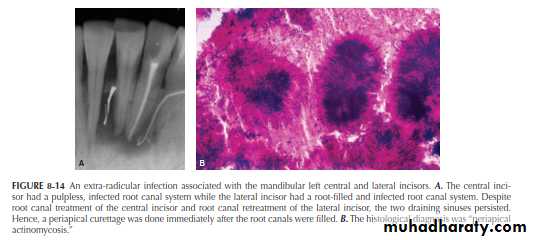
Extra-Radicular Infection
An extra-radicular infection occurs when bacteria establish
colonies on the external root surface within the periapical region.
It is usually a sequel to an infected root canal system and the extra-radicular
bacteria are similar to those found in infected root canals. Actinomyces species are often found in these cases .
Extra-radicular infections cannot be diagnosed clinically
and they can only be diagnosed histologically. However, cli-
nicians should recognize that this condition does occur and
it should be part of the differential diagnosis of a persistent
radiolucency following endodontic treatment.
Typical symptoms—may have no symptoms; may be asso-
ciated with persistent swelling and/or draining sinus;
patient may report a history of occasional “awareness”
of the tooth feeling different; history of recent or cur-
rent root canal treatment that is not resolving the
problem.
Clinical findings—may be caries, a restoration breaking down or a crack; tooth has signs of recent root canal treatment (e.g., access cavity restoration); not tender to percussion or may feel “different” to percussion; no response to pulp sensibility tests; some cases will have a persistent draining sinus despite recent or ongoing root canal treatment—the draining sinus may be intra- oral or extra-oral; palpation or pressure on the tissues
overlying the periapical region may cause pus to exude from the draining sinus, if present; can insert a gutta percha point into the draining sinus, if present, to trace it radiographically.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Radiographic findings—caries may be seen if exten-
sive enough; a periapical radiolucency is present; the
radiolucency is persisting or may be increasing in size
despite recent root canal treatment; root canal filling or
intracanal dressing evident; gutta percha point inserted
into the draining sinus, if present, can trace its origin to
the affected tooth.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY2020-2021
Key findings for diagnosis—a periapical radiolucency and no pain, typically has had recent root canal treatment without resolution of the periapical radiolucency.
Distinguish from a foreign body reaction, a periapical pocket cyst, a periapical true cyst , and a periapical scar by histological examination of a biopsy specimen.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
Foreign Body Reaction
A foreign body reaction is an inflammatory response to a foreign
material within the periapical tissues. The most common foreign
material is excess root filling material, such as gutta percha or root
canal cement that has been extruded through the apical foramen.
Radiographically, foreign body reactions usually appear as a periapical radiolucency surrounding some radiopaque .
Foreign body reactions cannot be diagnosed clinically and they can only be diagnosed histologically. However, clinicians should recognize that this condition does occur and
it should be part of the differential diagnosis of a persistent radiolucency following endodontic treatment.
Typical symptoms—usually no symptoms; the patient may report a history of occasional “awareness” of the tooth feeling different; history of recent or current endodontic treatment without resolution of the periapical radiolucency and/or symptoms.
Clinical findings—the tooth has signs of recent root canal treatment (e.g., access cavity restoration);
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
2020-2021
the tooth is not tender to percussion or may feel “different” to
percussion; no response to pulp sensibility tests.
Radiographic findings—a periapical radiolucency is present; the radiolucency is persisting or may be increasing in size despite recent root canal treatment; root canal filling or intracanal dressing evident; radiopaque material may be seen in the periapical tissues; some
cases may be due to materials that are not radiopaque and therefore not evident radiographically.
Key findings for diagnosis—there is a periapical radiolucency; usually no pain; typically has had root canal treatment without resolution of the periapical radiolucency; many cases have radiopaque material present within the periapical radiolucency.
Distinguish from an extra-radicular infection, a periapical
pocket cyst, a periapical true cyst, and a periapical scar byhistological examination of a biopsy specimen.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYTHE END
2020-2021
Hope to you life without apical pathosis