1
Hematopoiesis:
Hematopoiesis is the process by which all of your blood cells are formed, develop and mature into their final adult types.2
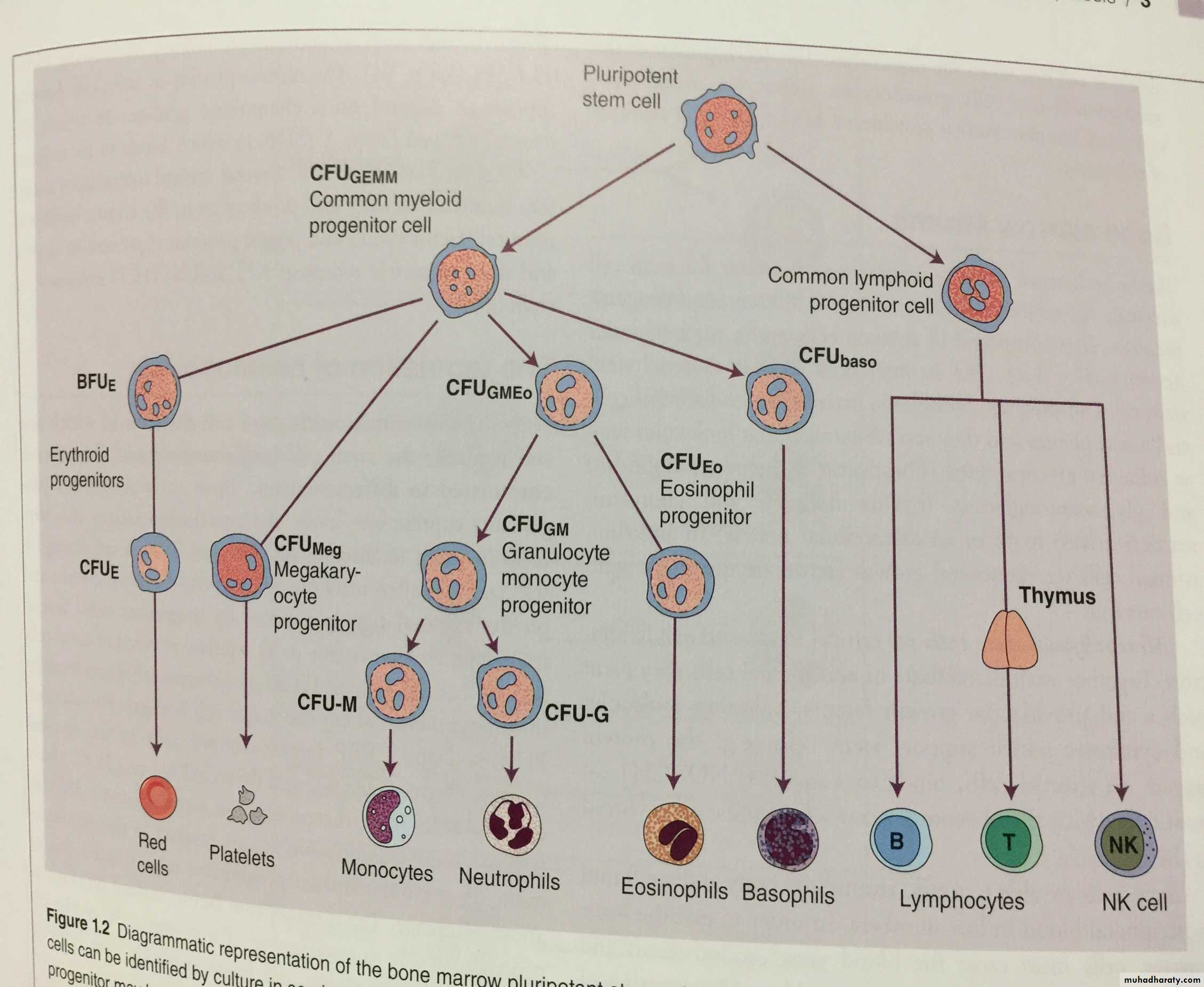
beginning with what’s known as a hematopoietic stem cell, going through a series of steps to arrive at the final product—a mature blood cell, whether it’s a red blood cell, a white blood cell such as a lymphocyte, or some other type of blood cell.
3
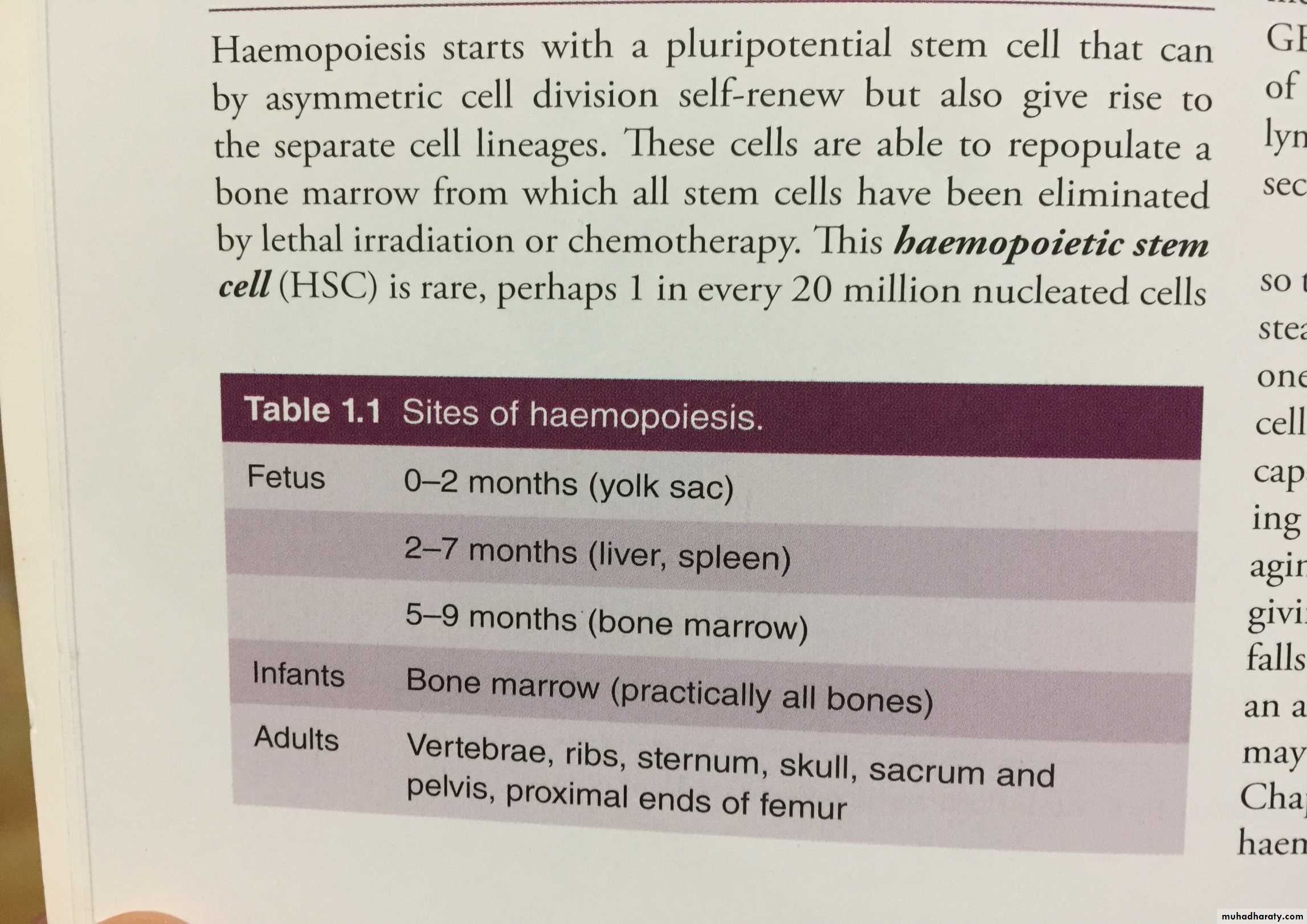
The sites of blood cell production depend on whethaer you are talking about a baby still in its mother’s womb, or after wards during infancy and throughout adulthood.
4
That is, in utero, a developing child uses a variety of different sites in the body for hematopoiesis, including the liver, spleen, thymus, lymph nodes, as well as the bone marrow. After birth, the main site of hematopoiesis is the bone marrow.
5
6
Extramedullary hematopoiesis is the formation of blood cells at sites other than the bone marrow. And while extramedullary hematopoiesis is the norm for a baby in the womb, once a person is born, it is generally a sign of disease, or an indication that the bone marrow is unable to produce enough healthy red blood cells to meet the demand.
7
Hematopoietic stem cell transplantation, also called bone marrow transplant or stem cell transplant, involves taking donated stem cells and giving them to a recipient, so that the recipient can make his or her own new red blood cells, white blood cells, and platelets.
8
Hematopoietic malignancy refers to cancer of the blood-forming cells. Hematopoietic malignancies include leukemia, lymphoma and myeloma
9
10
Circulating blood contains a mix of cells, cell products, and fluids. Our bodies produce blood cells continuously from the time we are in the womb up to to old age. Millions of blood cells are replaced each day as they live out their lifespans.
11
Different types of cells have different life spans, and in healthy adults, red blood cells normally live about 100 to 120 days before they need to be replaced.
12
Blood-forming cells make for two different sides of the family tree:
The lymphoid side is easier to remember because it gives rise to the white blood cells known as lymphocytes. Lymphocytes can be further classified as T cells, B cells and natural killer cells.13
The myeloid side of the family
You have your red blood cells, which are also called erythrocytes, as well as your blood platelets, which are basically called megakaryocytes.14
But then, in addition to your red blood cells and platelets, you also have all of the white blood cells that come from myeloid progenitors: neutrophils, monocytes, eosinophils and basophils are all white blood cells that come from the myeloid progenitors.
15
16
White blood cells (leukocytes): These include lymphocytes, monocytes and polymorphonuclear white cells that provide our bodies with protection from infection. Problems with white blood cells can lead to infection.
17
Red blood cells (erythrocytes): These cells contain the hemoglobin that gives your blood its red color and carries oxygen to the cells and tissues in your body. Deficiency of red blood cells can lead to anemia, with symptoms such as fatigue, weakness and intolerance to exercise.
18
Platelets: Megakaryocytes in the bone marrow are the "monster" cells (they are large compared to others) that produce (platelets) that help control bleeding after injury. Platelet deficiencies can lead to easy bruising and trouble with bleeding.
19
20
Hematopoietic Cell Transplantation - Bone Marrow Transplants
The treatment of leukemia, lymphoma and other blood cancers may involve a transplant of hematopoietic stem cells. These can be your own cells, harvested from your bone marrow (autologous), or from a donor (allogenic).21
Extramedullary Hematopoiesis
This is the term used for blood cell production that occurs outside of the bone marrow. It can be seen in chronic anemia, with production of blood cells in the liver, spleen and sometimes in the lymph nodes.22
The number of leukocytes in the blood is often an indicator of disease, and thus the WBC count is an important subset of the complete blood count. The normal white cell count is usually between 4 × 109/L and 11 × 109/L.
23
An increase in the number of leukocytes over the upper limits is called leukocytosis. It is normal when it is part of healthy immune responses, which happen frequently. It is occasionally abnormal, when it is neoplastic or autoimmune in origin. A decrease below the lower limit is called leukopenia. It weakens the immune system.
24
All white blood cells are nucleated, which distinguishes them from the anucleated red blood cells and platelets. Two pairs of broadest categories classify them either by structure (granulocytes or agranulocytes) or by cell lineage (myeloid cells or lymphoid cells).
25
26
These broadest categories can be further divided into the five main types: neutrophils, eosinophils, basophils, lymphocytes, and monocytes.
27
These types are distinguished by their physical and functional characteristics. Monocytes and neutrophils are phagocytic.
28
Neutrophil
Neutrophils are the most abundant white blood cell, constituting 60-70% of the circulating leukocytes. They defend against bacterial or fungalinfection.
29
They are commonly referred to as polymorphonuclear (PMN) leukocytes, although, in the technical sense, PMN refers to all granulocytes.
30
They have a multi-lobed nucleus, which consists of three to five lobes connected by slender strands.This gives the neutrophils the appearance of having multiple nuclei, hence the name polymorphonuclear leukocyte.
31
Neutrophils are active in phagocytosing bacteria and are present in large amount in the pus of wounds. Neutrophils are the most common cell type seen in the early stages of acute inflammation. The life span of a circulating human neutrophil is about 5.4 days
32
Eosinophil
Eosinophils compose about 2-4% of the WBC total. This count fluctuates throughout the day, seasonally, and during menstruation. It rises in response to allergies, parasitic infections, collagen diseases, and disease of the spleen and central nervous system.33
34
The most important causes of eosinophilia include allergies such as asthma, hay fever, and hives; and also parasitic infections.
35
Basophil
Basophils are chiefly responsible for allergic and antigen response by releasing the chemical histamine causing the dilation of blood vessels. Because they are the rarest of the white blood cells (less than 0.5% of the total count)36
They excrete two chemicals that aid in the body's defenses: histamine and heparin. Histamine is responsible for widening blood vessels and increasing the flow of blood to injured tissue.
37
Heparin is an anticoagulant that inhibits blood clotting and promotes the movement of white blood cells into an area.
38
Lymphocyte
Lymphocytes are much more common in the lymphatic system than in blood. Lymphocytes include:B cells make antibodies that can bind to pathogens.
39
T cells:
CD4+ helper T cells:CD8+ cytotoxic T cells:
Natural killer cells .
40
Monocyte
Monocytes, the largest type of WBCs, share the "vacuum cleaner" (phagocytosis) function of neutrophils, but are much longer lived.41
Monocytes eventually leave the bloodstream and become tissue macrophages, which remove dead cell debris as well as attack microorganisms.
42
Histiocytes
Dendritic cellsMast cells
43
44
Disorders
The two commonly used categories of white blood cell disorders divide them quantitatively into those causing excessive numbers (proliferative disorders) and those causing insufficient numbers (leukopenias).45
WBC proliferative disorders can be classed as myeloproliferative and lymphoproliferative. Some are autoimmune, but many are neoplastic.
46
Another way to categorize disorders of white blood cells is qualitatively. There are various disorders in which the number of white blood cells is normal but the cells do not function normally
47
Leucopenias
This type of white blood cell decreased is usually the neutrophil. In this case the decrease may be called neutropenia. Less commonly, a decrease in lymphocytes (called lymphocytopenia or lymphopenia) may be seen.48
Neutropenia
Neutropenia can be acquired or intrinsic. A decrease in levels of neutrophils on lab tests is due to either decreased production of neutrophils or increased removal from the blood.49
Medications - chemotherapy, sulfas or other antibiotics.
RadiationToxins - alcohol, benzenes
50
Intrinsic disorders - Fanconi's, cyclic neutropenia, Chédiak–Higashi
Immune dysfunction AIDS, rheumatoid arthritisBlood cell dysfunction - megaloblastic anemia, myelodysplasia, marrow failure, acute leukemia
Any major infection
Miscellaneous - starvation, hypersplenism
51
Lymphocytopenia
Like neutropenia, lymphocytopenia may be acquired or intrinsic and there are many causes.52
Inherited immune deficiency - severe combined immunodeficiency, common variable immune deficiency, ataxia-telangiectasia, Wiskott-Aldrich syndrome,,
Blood cell dysfunction - aplastic anemia
53
Infectious diseases - viral (AIDS, SARS, hepatitis)
bacterial (TB, typhoid, pneumonia), parasitic( malaria)54
Medications – chemotherapy
RadiationMajor surgery
Miscellaneous kidney or bone marrow transplant,
55
56
Immune dysfunction - arthritis, systemic lupus erythematosus,
Nutritional/Dietary - alcohol abuse, zinc deficiency57
58
Leukocytosis
An increase in the number of white blood cells in circulation is called leukocytosis
This increase is most commonly caused by inflammation.
59
There are four major causes: increase of production in bone marrow, increased release from storage in bone marrow, decreased attachment to veins and arteries, decreased uptake by tissues.
60
Leukocytosis may affect one or more cell lines and can be neutrophilic, eosinophilic, basophilic, monocytosis, or lymphocytosis.
61
Neutrophilia
Neutrophilia is an increase in the absolute neutrophil count in the peripheral circulation. Most cases of neutrophilia are secondary to inflammation62
Primary causes
Conditions with normally functioning neutrophils – hereditary neutrophilia, Pelger–Huet anomalyLeukemia (chronic myelogenous (CML)) and other myeloproliferative disorders
Surgical removal of spleen
63
Secondary causes
Chronic inflammation – especially juvenile rheumatoidinfections (for example, tuberculosis), and chronic hepatitis
Cigarette smoking – occurs in 25–50% of chronic smokers and can last up to 5 years after quitting
64
Stress – exercise, surgery, general stress
Medication induced – corticosteroidsCancer
65
Eosinophilia
Eosinophil counts are higher in newborns and vary with age, exercise, environment, and exposure to allergens. Eosinophilia is never a normal lab finding.66
Lymphocytosis
is a feature of infection, particularly in children. In the elderly, lymphoproliferative disorders, including chronic lymphocytic leukaemia and lymphomas, often present with lymphadenopathy and a lymphocytosis.67
Causes of absolute lymphocytosis include:
acute viral infections, such as infectious mononucleosis other acute infections such as pertussissome protozoal infections, such as toxoplasmosis
68
chronic intracellular bacterial infections such as tuberculosisor brucellosis
chronic lymphocytic leukemiaacute lymphoblastic leukemia
69
70