Clinical manifestations;
*Intrauterine; growth restriction and increased vascular resistance may be the 1st manifestation of fetal hypoxia.*During labor, the fetal heart rate slows down, and beat-to-beat variability declines. 1Continuous heart rate recording may reveal variable or late deceleration pattern, and 2fetal scalp blood analysis may show a pH <7.20. Particularly in infants near term, these signs should lead to the administration of high concentrations of 1oxygen to the mother and 2immediate delivery to avoid fetal death or CNS damage.
*At delivery; the presence of yellow, meconium-stained amniotic fluid is evidence that fetal distress has occurred.
*At birth; these infants are frequently depressed and fail to breathe spontaneously. During the ensuing hours, they may remain hypotonic or change from hypotonic to hypertonic, or their tone may appear normal. Pallor, cyanosis, apnea, a slow heart rate, and unresponsiveness to stimulation are also signs of HIE.
Cerebral edema may develop during the next 24 hr and result in profound brain stem depression. During this time, seizure activity may occur; it may be severe and refractory to the usual doses of anticonvulsants.
In addition to CNS dysfunction, systemic hypoperfusion occurs in 80% of cases including; heart failure and cardiogenic shock, hypotension, persistent pulmonary hypertension, respiratory distress syndrome, gastrointestinal perforation, acute tubular or cortical necrosis and hematuria, adrenal hemorrhage, inappropriate secretion of antidiuretic hormone and metabolic derangements are associated with perinatal asphyxia. After delivery, hypoxia is due to respiratory failure and circulatory insufficiency. During the initial hours after an insult, infants have a depressed level of consciousness. Periodic breathing with apnea or bradycardia is present, but cranial nerve functions are often spared with intact papillary responses and spontaneous eye movement. Seizures are common with extensive Injury. Hypotonia is also common as an early manifestation.
HIE in term infants:
Signs
Stage 1
Stage 2
Stage 3
Consciousness
Hyper-alert
Lethargic
Stuporous, coma
Muscle tone
Normal
Hypotonic
Flaccid
Posture
Normal
Flexion
Decrebrate
Tendon reflexes/ clonus
Hyperactive
Hyperactive
Absent
Myoclonus
Present
Present
Absent
Moro reflex
Strong
Weak
Absent
Pupils
Mydriasis
Miosis
Poor light reflex
Seizures
None
Common
Decerebration
EEG
Normal
Low voltage changing to severe seizure activity
Burst suppression to iso-electric
Duration
<24hr if progresses; or may remain normal
24hr to 14 days
Days to weeks
Outcome
Good
Variable
Death, severe deficits
Diagnosis;
*Diffusion-weighed MRI: is the preferred imaging modality because of its increased sensitivity and specifity.
*CT scans: are helpful in identifying focal hemorrhage, diffuse cortical injury, and damage to the basal ganglia; CT has limited ability to identify cortical injury within the 1st few days of life.
*Amplitude integrated EEG (aEEG): has a good reliability & positive predictive value of 85% for infants who will have adverse neurodevelopmental outcome.
*Ultrasound: has limited utility in evaluation of hypoxic injury in the term infant; it is preferred in evaluation of the preterm infant.
Treatment;
*Phenobarbital is the drug of choice, is given with an intravenous loading dose (20 mg/kg); additional doses of 5-10 mg/kg (up to 40-50 mg/kg total) may be needed. Phenytoin (20 mg/kg loading dose) or lorazepam (0.1 mg/kg) may be needed for refractory seizures. Phenobarbital levels should be monitored 24 hr after the loading dose and maintenance therapy (5mg/kg/24 hr) are begun. Seizures in HIE may also be due to hypocalcaemia, hypoglycemia, or infection.*Systemic or selective cerebral hypothermia for acute management of HIE is promising, as it decrease metabolism and suppress production of mediators known to be neurotoxic.
*Others include; supportive care for organ dysfunction, careful ventilation, blood pressure, acid-base balance and control of possible infection.
Prognosis;
it varies depending on 1. whether the metabolic & cardiopulmonary complication (hypoxia, hypoglycemia, shock) are treated, 2. the infant's gestational age (outcome is poorest if the infant is preterm), and 3. the severity of the encephalopathy. Severe encephalopathy is characterized by flaccid coma, apnea, and refractory seizures, and is associated with a poor prognosis.*Low Apgar score at 20 min, absence of spontaneous respirations at 20 min of age, and persistence of abnormal neurological signs at 2 weeks of age also predict death or severe cognitive or motor deficit.
*Normal MRI and EEG findings are associated with a good recovery, whereas severe MRI and EEG abnormalities predict a poor outcome.
*Microcephaly and poor head growth during 1st year of life also correlate with injury to the basal ganglia and white matter and adverse developmental outcome at 12 month.
Pathological correlation of preterm infant with hypoxic ischemic encephalopathy
Pathology
Clinical sign
Periventricular leukomalacia
Spastic diaplegia
Status marmoratus of basal ganglia
Dystonia, choreoathetosis
Thalamus
Mental retardation
Cerebral cortex
Mental retardation
Pathological correlation of full term infant with hypoxic ischemic encephalopathy
Pathology
Pathology
Parasagittal cortical and subcortical neuronal necrosis
Spastic quadriplegia, especially arms. Intellectual deficits and cortical atrophy, focal seizures and hemiplegia
Cerebellum
Ataxia
Brain stem
Pseudobulbar palsy
THE PRINCIPLES OF NEONATAL RESUSCITATION;
Preparation for ResuscitationImmediate, effective resuscitation of the newborn infant can reduce or prevent morbidity and mortality and to establish adequate spontaneous respiration and cardiac output. Conditions requiring skilled resuscitation to be available at delivery are;
Intrapartum Problems
• Fetal distress (Persistent late decelerations, severe variable decelerations without baseline variability,
scalp pH <7.25, meconium-stained amniotic fluid and cord prolapse).
• Prolonged, unusual or difficult labor
• Emergency operative delivery
• Vaginal Breech delivery
Medical/Obstetric/Genetic Problems
• Diabetes mellitus • Suspected or confirmed maternal infection
• Substance abuse i.e. drugs • Third trimester bleeding
• Pregnancy-induced hypertension • Abnormal amniotic fluid volume
• Prolonged rupture of membranes • Multiple gestation
• Low-birth-weight infant (<2.5Kg) • Prematurity (<37weeks gestation)
• Isoimmunization i.e.Rh factor incompatibility • Fetal congenital anomalies
Resuscitation equipment and drugs should always be readily available in resuscitation trolley, functional, and assembled for immediate use in the delivery room.
Immediate steps after birth in an infant in need of resuscitation;
(1) Prevention of heat loss
• Place the infant under a radiant heat source.
• Dry the infant thoroughly and remove the wet linen.
(2) Clearing the airway
• Position the infant supine and flat with the neck slightly extended.
• Suction the mouth then the nasopharynx to clear the airway.
• Turn the head to the side to allow secretions to pool, and then remove with a bulb syringe or suction catheter. Deep pharyngeal suction should not be performed during the first few minutes after birth to avoid vagal depression and resultant bradycardia.
(3) Initiation of breathing
• Provide tactile stimulation by rubbing the back or gently slapping the feet
Assess the heart rate, respiratory effort and color.
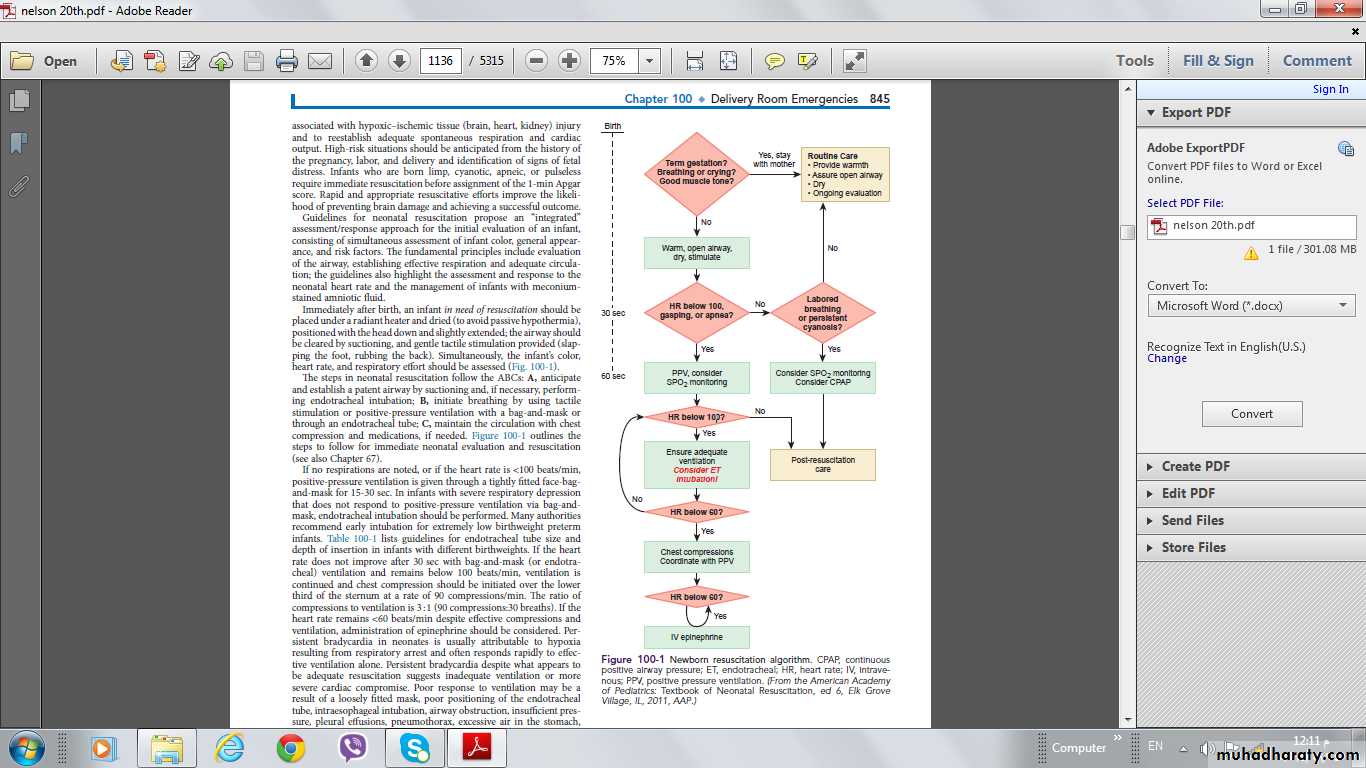
The steps of neonatal resuscitation following the standard ABCs of resuscitation:
• A- Airway (Establish an airway, Positioning, Suctioning and Endotracheal intubation if necessary).• B- Breathing (Initiate breathing, tactile stimulation, Positive pressure ventilation).
• C- Circulation (Maintain circulation, Chest compressions, Medications).
At each step of the resuscitation procedure, evaluation is based on the infant's respirations, heart rate, and color.
If no respirations are noted or if the heart rate is below 100/min, 1 positive pressure ventilation is given through a tightly fitted face mask and bag for 15-30 sec. In Infants with severe respiratory depression who do not respond to positive pressure ventilation via bag and mask, 2 endotracheal intubation should be performed. If the heart rate does not improve after 30 sec with bag and mask (or endotracheal) ventilation and remains below 100/min, 3 ventilation is continued and chest compression should be initiated over the lower third of the sternum at ratio of compressions to ventilation is 3:l.
If the heart rate remains <60 despite effective compressions and ventilation, 4 administration of epinephrine should be considered. Persistent bradycardia in neonates is usually due to hypoxia resulting from respiratory arrest and often responds rapidly to effective ventilation alone. Persistent bradycardia despite what appears to be adequate resuscitation suggests more inadequate ventilation technique or severe cardiac compromise. Traditionally, the inspired gas for neonatal resuscitation has been 100% oxygen. Resuscitation with room air is equally effective.
Although the 1st breath normally requires pressures as low as 15-20 cm H2O, pressures as high as 30-40 cm H2O may be needed. Subsequent breaths are given at a rate of 40-60/min with a pressure of 15-20 cm H2O.
Successful ventilation is determined by;
1. adequate chest rise, 2. symmetric breath sounds, 3. improved pink color, 4. heart rate >100/min, 5. spontaneous respirations, 6. presence of end-tidal CO2, and 7. improved tone.
If the infant has respiratory depression and the mother has a history of analgesic narcotic drug administration within 4 hr prior to delivery, naloxone hydrochloride (0.1 mg/kg) is given while adequate ventilation is maintained, repeated doses of naloxone may be needed.
Medications are rarely required but should be administered when the heart rate is < 60/min after 30 sec of combined ventilation and chest compressions or during asystole. The umbilical vein can generally be readily cannulated and used for immediate administration of medications during neonatal resuscitation.
*Administration of epinephrine (0.1- 0.3 ml/Kg of 10 000 solution) via endotracheal tube or IV may be used, may be repeated every 3-4 min.
*Volume expanders: in acute bleeding and hypovolemia; poor response to other resuscitative measures(0.9% N/S, 10ml/Kg, IV).
*Sodium bicarbonate: in documented or suspected metabolic acidosis in the presence of adequate ventilation (2meq/Kg, IV).
*Dobutamine and fluids should be started to improve cardiac output in an infant with poor peripheral perfusion, weak pulses, hypotension, tachycardia, and poor urine output.
If any meconium staining is present in the amniotic fluid, the obstetrician should suction the mouth, nose, and hypopharynx immediately after delivery of the head and before delivery of shoulders. If the baby is vigorous, with good respiratory effort & Heart rate >100/min, tracheal intubation to aspirate meconium should not be attempted, otherwise in a depressed infant with poor muscle tone and or a heart rate < 100/min, tracheal intubation and suctioning should be performed.
Newborn resuscitation algorithm.
CPAP, continuous positive airway pressure; ET, endotracheal; HR, heart rate; IV, intravenous; PPV, positive pressure ventilation