Phase II Periodontal Therapy
Corrective phaseUNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
By:
Dr. Huda A. Salim
B.D.S, M.Sc. In Oral and Maxillofacial Surgery
Mosul University/College of Dentistry.
2020-2021
Department of:Oral and Maxillofacial Surgery
Department of:
HERE
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYp.d.surgery; specific surgical manipulation of p.d. soft tissue & bone.
Early problems can be corrected with successful phase I therapy, consisting of biofilm removal by the patient on a daily basis, scaling, and root planing when necessary.
moderate to advanced cases cannot be resolved without surgically gaining access to the root surface for root planing and reducing or eliminating pocket depth to allow the patient to remove biofilm.
The surgical phase of therapy is also referred to as phase II therapy.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY• Phase II therapy is used to surgically treat residual
periodontal pockets and bone defects remaining after
phase I therapy. All patients treated surgically need to
have a preoperative history of adequate plaque control
with 20% or more of tooth surfaces free of plaque afteroral hygiene procedure.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYAfter 1-3 m. of completion of phase I; Evaluation should
be done for the:
1- Resolution of Gingival inflammation2-Reduction of pocket depth & attachment loss
3- Reduction of tooth mobility
4- O.H. improvment
5- Rechecking presence of ca.,Root caries ,defective restoration
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYThe results of Evaluation showed the following
• Good O.H. but still BOP, no reduction of P.D.; p.d. surgery
• Good O.H., no G. inflammation, reduction of P.D. & CAL; maintenance phase
Poor O.H. lack compliance or ability for home care; motivation & instructionUNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYPurposes of periodontal surgery
Controlling or eliminating periodontal disease.
Correcting anatomic conditions that favor periodontal disease, impair aesthetics, or impede placement of prosthetic appliances.
Placing implants to replace lost teeth and improving the environment for their placement and function.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
Objectives of the Surgical Phase
The surgical phase of P.D. therapy has the following objectives:
1. To improve the prognosis for teeth and their replacements
2. To improve aesthetics.
Surgical techniques are used for pocket therapy and for correction of related morphologic problems (i.e., Mucogingival defects). In many cases, therapies are combined to provide one surgical intervention that fulfills both objectives.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYIndications for surgical treatment
1-Impaired access for scaling and root planing:
The difficulties in accomplishing proper root debridement with a non‐surgical approach increase with:
(1) increasing depth of the periodontal pockets,
(2) increasing width of the tooth surfaces, and
(3) The presence of root fissures, root concavities, furcation, and defective margins of dental restorations in the subgingival area.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY020-2021
2-Impaired access for self‐performed plaque control:
The level of infection control that can be maintained by the patient is determined not only by his/her interest and dexterity, but also, to some extent, by the morphology of the dentogingival area.
Pronounced gingival hyperplasia and presence of gingival craters are examples of morphologic aberrations that may impede proper home care.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYContraindications for periodontal surgery
1-Patient cooperation:
a patient who fails to cooperate during the cause‐related phase of therapy should not be exposed to surgical treatment.
A typical recall schedule for periodontal patients involves professional consultations for supportive periodontal therapy once every 3–6 months.
Patients who cannot maintain satisfactory oral hygiene standards over such a period should normally not be considered to be candidates for periodontal surgery.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY020-2021
2-Smoking:
Although smoking negatively affects wound healing, it may not be considered a contraindication for surgical periodontal treatment.
less resolution of probing pocket depth, smaller improvement in clinical attachment, and less bone regeneration might occur in smokers than in non‐smokers.
3-General health conditions:
It is important to re‐evaluate the patient’s medical history before any surgical intervention to identify whether there is any medical condition that may preclude periodontal surgery or whether certain precautions should be taken.UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY020-2021
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY020-2021
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYCriteria for Selection of the Method of Surgical Therapy
Selection of a technique for treating a particular periodontal lesion is based on the following considerations:
1. Characteristics of the pocket: depth, relation to bone, and configuration.
2. Accessibility to instrumentation, including furcation involvement.
3. Existence of mucogingival problems.
4. Response to phase I therapy.
5. Patient cooperation, including the ability to perform effective oral hygiene and stop smoking.
6. Age and general health of the patient.
7. Overall diagnosis of the case: various types of gingival enlargement and types of periodontitis (e.g., chronic marginal periodontitis, localized aggressive periodontitis, generalized aggressive periodontitis).
8. Aesthetic considerations.
9. Previous periodontal treatments.
UNIVERSITY OF MOSUL
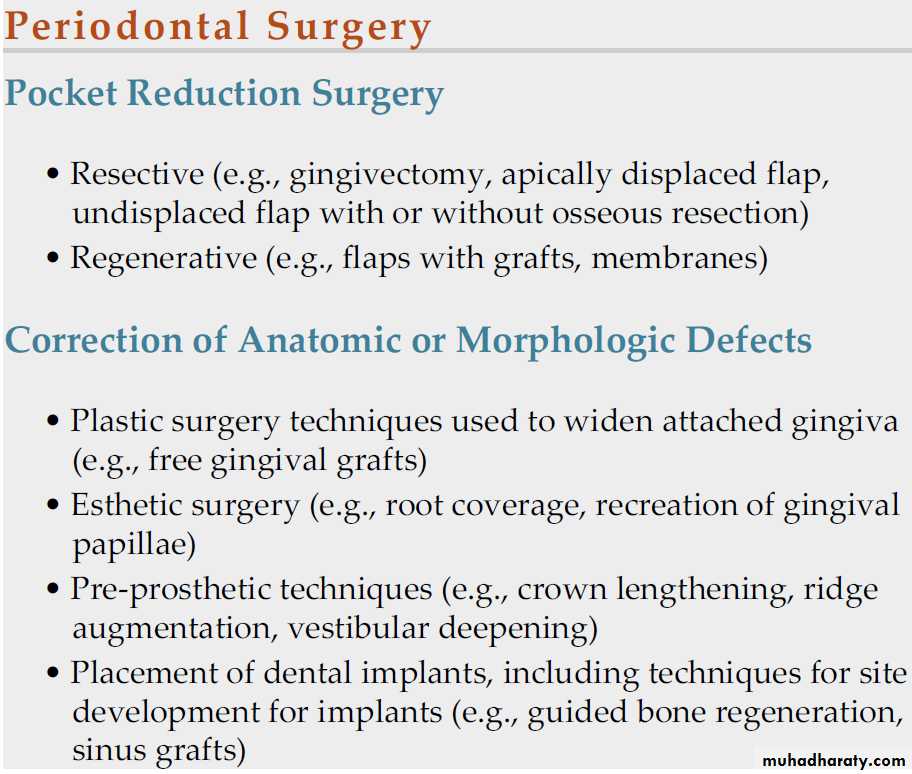
COLLEGE OF DENTISTRYSurgical Pocket Therapy
Surgical pocket therapy can be used to gain access to the diseased root surface to ensure the removal of calculus located subgingivally before surgery and to eliminate or reduce the depth of the periodontal pocket.
Successful periodontal therapy completely eliminates calculus, plaque or biofilm, and diseased Cementum from the tooth surface.
Pocket elimination is another important consideration. It consists of reducing the depth of the periodontal pocket to that of a physiologic sulcus to enable cleaning by the patient.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYDepartment of:
HERE
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYResults of Pocket Therapy
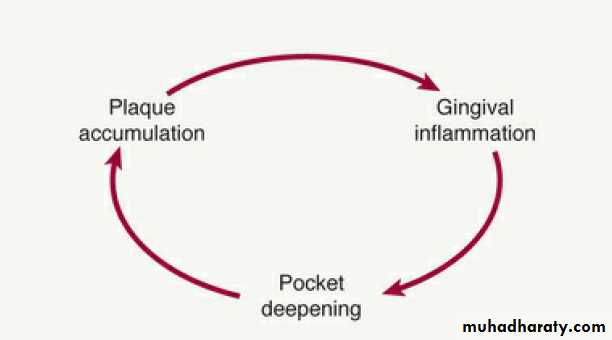
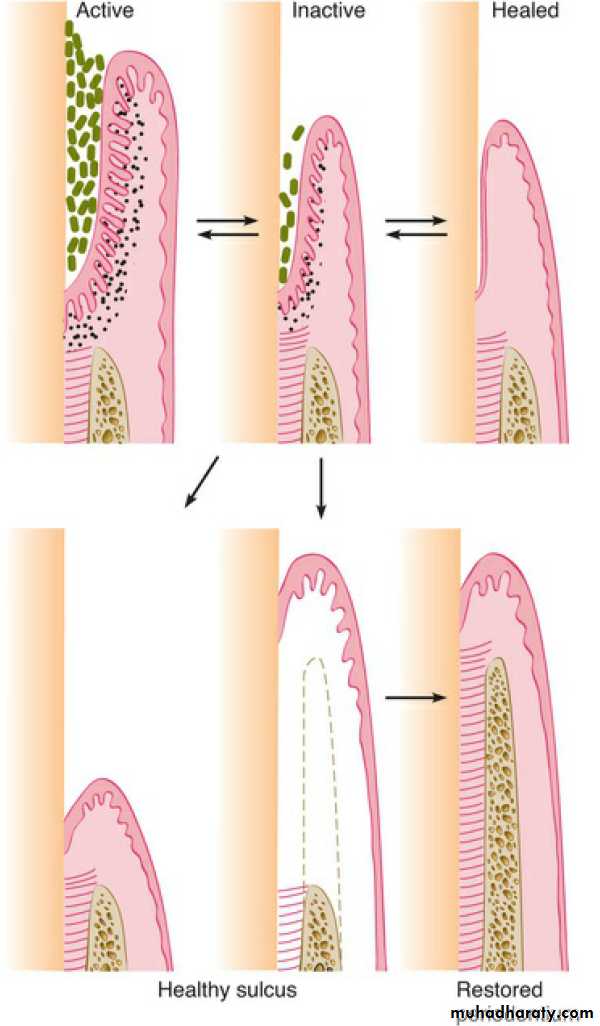
A periodontal pocket can be in an active state or a period of inactivity or quiescence.
In an active pocket, underlying bone is being lost.
It often is diagnosed clinically by bleeding that occurs spontaneously or in response to probing.
After phase I therapy, the inflammatory changes in the pocket wall subside, rendering the pocket inactive and reducing its depth.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYDepartment of:
HERE
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYDepartment of:
HERE
Critical Zones in Pocket Surgery
Criteria for the selection of a surgical technique for pocket therapy are based on clinical findings in the soft tissue pocket wall, tooth surface, underlying bone, and attached gingiva.
Zone 1: Soft Tissue Pocket Wall:
The clinician should determine the morphologic features, thickness, and topography of the soft tissue pocket wall and persistence of inflammatory changes in the wall.
Zone 2: Tooth Surface: The clinician should identify the deposits on and alterations of the cementum surface and determine the accessibility of the root surface to instrumentation.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYZone 3: Underlying Bone: The clinician should establish the shape and height of the alveolar bone next to the pocket wall through careful probing and clinical and radiographic examinations.
Zone 4: Attached Gingiva: The clinician should consider the presence or absence of an adequate band of keratinized, attached gingiva when selecting the pocket treatment method. An inadequate attached gingiva can be caused by a high frenum attachment, marked gingival recession, or a deep pocket that reaches the level of the Mucogingival junction.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYMethods of Pocket Therapy
The methods for pocket therapy can be classified as follows:1. New attachment techniques.
2. Removal of the pocket wall.
• Retraction or shrinkage
•Gingivectomy or the undisplaced flap technique.
• Apical displacement.
3. Removal of the tooth side of the pocket.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYReevaluation After Phase I Therapy
all patients should be treated initially with scaling, root planing, and plaque or biofilm control and that a final decision on the need for periodontal surgery should be made only after a thorough evaluation of the effects of phase I therapy.
Assessment typically is made no less than 1 to 3 months and sometimes as much as 9 months after the completion of phase I therapy.
Calculus, root caries, defective restorations, and signs of persistent inflammation should also be evaluated.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYApproaches to Specific Pocket Problems
Therapy for Gingival Pockets: Gingival pockets do not have an osseous component .Two factors are taken into consideration:
1- the character of the pocket wall
2-the accessibility of the pocket.
Edematous tissue: shrinks after the elimination of local factors, reducing or totally eliminating pocket depth. Scaling and root planing is the technique of choice for these cases.
Pockets with a fibrotic wall are not appreciably reduced in depth after scaling and root planing. These pockets are eliminated or reduced by surgical therapy.
gingivectomy was frequently used to reduce these pockets, but in cases of marked gingival enlargement (e.g., severe phenytoin-related enlargement), treatment could leave a large, open wound, and the patient had to endure a painful and prolonged healing process. Currently, a modified flap technique is used, and fewer postoperative problems are associated with primary closure of the wound.
laser therapy to manage gingival Enlargement.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYTherapy for Incipient Periodontitis
In patients with slight or incipient periodontitis with minimal attachment and bone loss, the pocket depths are shallow or a moderate depth.
In these patients, the conservative approach of good oral hygiene will generally suffices to control the disease.
Incipient periodontitis that recurs in previously treated sites may require a thorough analysis of the recurrence.
Occasionally, a surgical approach may be required to correct these problems.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYTherapy for Moderate to Severe Periodontitis in the
Anterior Sector
Because the maxillary anterior teeth are important aesthetically; therefore techniques that cause the least amount of visual root exposure should be considered.
The anterior dentition has two advantages for using a conservative (nonsurgical) approach:
(1) the teeth are all single rooted and easily accessible.
(2) patient compliance and thoroughness in plaque or biofilm control may be easier to attain.
Nonsurgical therapy is therefore the technique of choice for the maxillary anterior dentition.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYDepartment of:
HERE
In some situations, surgical therapy may be necessary to improve accessibility for root planing, or regenerative therapy.
The papilla preservation flap or modified papilla preservation flap can be used.
When the interdental space is minimal, papilla preservation techniques may not be feasible. Instead, a technique that splits the papilla and retains as much of the papilla as possible is the appropriate surgical technique.
When the aesthetic outcome is not the primary consideration and a flap procedure is necessary for root surface access, the modified Widman flap can be selected.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYTherapy for Moderate to Severe Periodontitis in Posterior Areas
Treatment for the maxillary and mandibular premolars and molars does not entail aesthetic problems but frequently involves difficult access for root therapy. Bone defects occur more often in the posterior area than the anterior sector.
A difficult problem encountered in the posterior area is the furcation lesion; therefore surgery is frequently indicated.
Surgery is used in the posterior area for enhanced access to the root surface or for definitive pocket reduction requiring osseous surgery.
Access can be obtained by an undisplaced or apically displaced flap.
Most patients with moderate to severe periodontitis have developed osseous defects that require some degree of bone remodeling or reconstruction.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY For osseous defects amenable to reconstruction, the papilla preservation flap or modified papilla preservation flap is the technique of choice because it better protects the interproximal areas.
For osseous defects with no possibility of reconstructive therapy, such as interdental craters, the technique of choice is an undisplaced or apically displaced flap with osseous contouring.
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY