Surgical RX for obesity
Dheyaa Kadhim Al-Waeli - MD, FICMS, MSc. (Endo.)Assistant professor University of Thi-Qar, College of medicine , Department of Medicine
Adult Endocrinologist: Thi-Qar Specialized Daibetes Endocrine and Metabolism Center (TDEMC)
E-mail: dheyaaalwaeli@yahoo.com
Email: dhiaa.alwaeli@fdemc.iq
ORCID iD:http://orcid.org/ 0000-0001-8738-2205
L3 22 DEC 2020
Surgery• ‘Bariatric’ surgery is by far the most effective long-term treatment for obesity and is the only anti-obesity intervention that has been associated with reduced mortality.
• Bariatric surgery should be contemplated in:-
• Motivated patients
• Who have very high risks of complications of obesity
• When extensive dietary and drug therapy has been insufficiently effective.
Which patient can do surgery???
It is usually reserved for those with :-
• Severe obesity (BMI > 40 kg/m2 )• Those with a BMI > 35 kg/m2 and significant complications, such as T2DM or obstructive sleep apnoea (OSA)
• Some evidence-based guidelines now suggest surgery can be considered at a lower weight in people with recent-onset diabetes and a BMI > 30 kg/m2
Only experienced specialist surgeons should undertake these procedures, in collaboration with a multidisciplinary team. Several approaches are used and all can be performed laparoscopically.
What is the mechanism of WT loss ????
The mechanism of weight loss may not simply relate to
• limiting the stomach or absorptive capacity, but rather in• Disrupting the release of ghrelin from the stomach or
• Promoting the release of other peptides from the small bowel, thereby enhancing satiety signalling in the hypothalamus
• Hormonal
• Mechanical
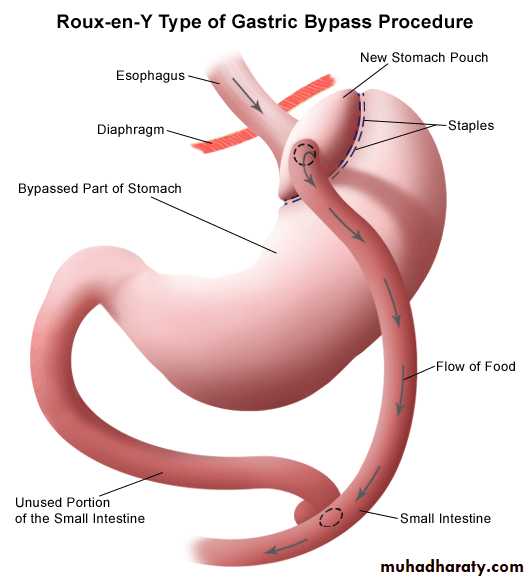
Diabetes may improve rapidly after surgery, particularly after gastric bypass, and although this may be attributed to severe energy restriction in the perioperative period, it is possible that increased release of incretin hormones such as GLP-1 may contribute to the improvement in glucose control.
Complications depend on the approach.
• Mortality is low in experienced centres but post-operative:- Respiratory problems
• Wound infection and dehiscence
• Staple leaks
• Stomal stenosis
• Marginal ulcers and venous thrombosis may occur.
Additional problems may arise at a later stage, such as:
• Pouch and distal oesophageal dilatation
• Persistent vomiting, ‘dumping’
• Hypoglycaemia and
• Micronutrient deficiencies, particularly of folate, vitamin B12 and iron, which are of special concern to women contemplating pregnancy; this should be delayed for at least 2 years following surgery.
??
??
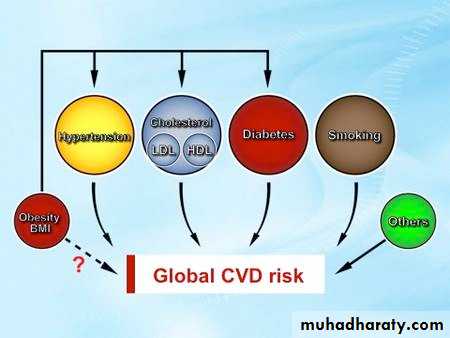
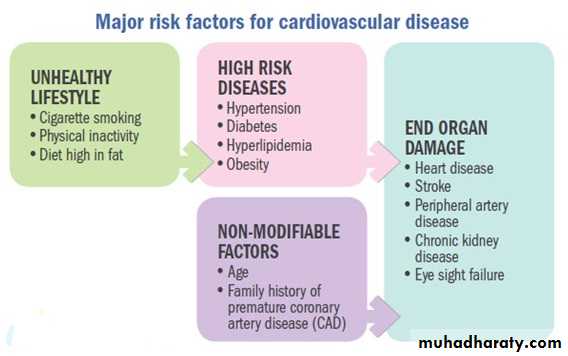
Obesity must not be treated in isolation and other risk factors must be addressed, including
• Smoking
• Excess alcohol consumption
• DM & HTN
• Hyperlipidemia
• OSA.
Treatment of additional risk factors
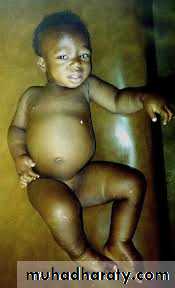
Under-nutrition Starvation and famine
There remain regions of the world, particularly rural Africa, where under-nutrition due to famine is endemic, the prevalence of BMI of less than 18.5 kg/m2 in adults is as high as 20%, and growth retardation due to under-nutrition affects 50% of children.The World Health Organisation (WHO) reports that chronic under-nutrition is responsible for more than half of all childhood deaths worldwide.
How does starvation present ???
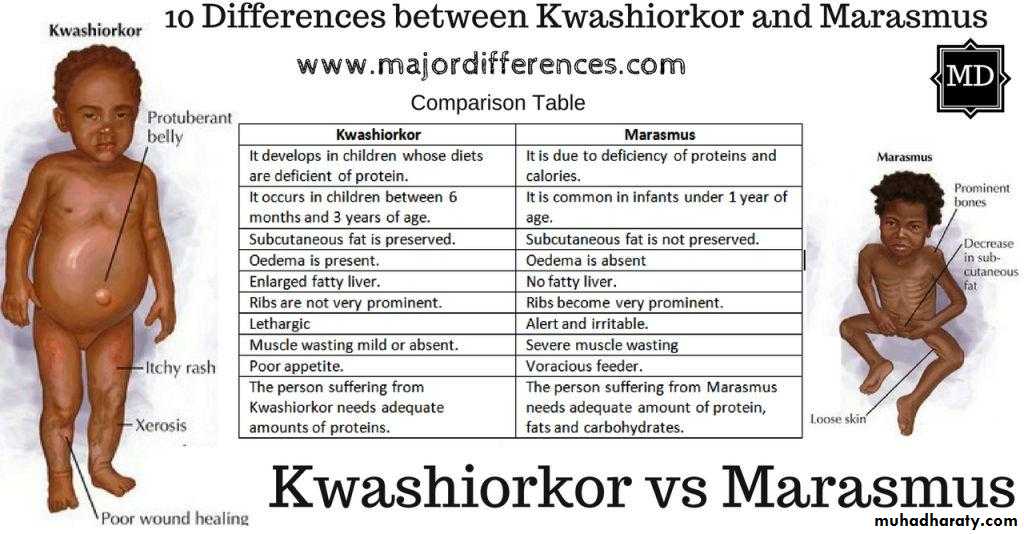
Starvation is manifest as marasmus (malnutrition with marked muscle wasting) or, when additive complications such as oxidative stress come into play, malnourished children can develop kwashiorkor (malnutrition with oedema).
Growth retardation is due to deficiencies of key nutrients (protein, zinc, potassium, phosphate and sulphur).
In adults, starvation is the result of chronic sustained negative energy (calorie) balance.
Clinical features
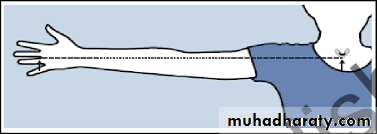
In starvation, the severity of malnutrition can be assessed by anthropometric measurements, such as BMI. Demispan and mid-arm circumference measurements are most useful in monitoring progress during treatment.
Under-nutrition often leads to vitamin deficiencies, especially of thiamin, folate and vitamin C.
Diarrhoea can lead to depletion of sodium, potassium and magnesium.
The high mortality rate in famine situations is often due to outbreaks of infection, such as typhus or cholera, but the usual signs of infection may not be apparent.
In advanced starvation, patients become completely inactive and may assume a flexed, fetal position. In the last stage of starvation, death comes quietly and often quite suddenly. The very old are most vulnerable.
All organs are atrophied at necropsy, except the brain, which tends to maintain its weight
What are the Clinical features of severe under-nutrition in adults
Clinical features of severe under-nutrition in adults
• Weight loss• Thirst, craving for food, weakness and feeling cold
• Nocturia, amenorrhoea or impotence
• Lax, pale, dry skin with loss of turgor and, occasionally, pigmented patches
Cold and cyanosed extremities, pressure sores
• Hair thinning or loss (except in adolescents)
• Muscle-wasting, best demonstrated by the loss of the temporalis and periscapular muscles and reduced mid-arm circumference
• Loss of subcutaneous fat, reflected in reduced skinfold thickness and mid-arm circumference
• Hypothermia, bradycardia, hypotension and small heart
• Oedema, which may be present without hypoalbuminaemia (‘famine oedema’)
• Distended abdomen with diarrhea
• Diminished tendon jerks
• Apathy, loss of initiative, depression, introversion, aggression if food is nearby
• Susceptibility to infections
Investigations
In a famine, laboratory investigations may be impractical but will show that• Plasma free fatty acids are increased and there is ketosis and a mild metabolic acidosis.
• Plasma glucose is low but albumin concentration is often maintained because the liver still functions normally.
• Insulin secretion is diminished, glucagon and cortisol tend to increase, and reverse T3 replaces normal triiodothyronine.
• The resting metabolic rate falls, partly because of reduced lean body mass and partly because of hypothalamic compensation.
• The urine has a fixed specific gravity and creatinine excretion becomes low.
• There may be mild anaemia, leucopenia and thrombocytopenia. The erythrocyte sedimentation rate (ESR) is normal unless there is infection.• Tests of delayed skin hypersensitivity, e.g. to tuberculin, are falsely negative.
• The electrocardiogram (ECG) shows sinus bradycardia and low voltage.
What are the most common Infections associated with starvation??
Infections associated with starvation
• Gastroenteritis and Gram-negative sepsis
• Respiratory infections, especially bronchopneumonia
• Certain viral diseases, especially measles and herpes simplex
• Tuberculosis
• Streptococcal and staphylococcal skin infections
• Helminthic infestations
Management
Whether in a famine or in wasting secondary to disease, the severity of under-nutrition is graded according to BMI.People with mild starvation are in no danger; those with moderate starvation need extra feeding; and those who are severely underweight need hospital care.
In severe starvation, there is atrophy of the intestinal epithelium and of the exocrine pancreas, and the bile is dilute.
It is critical for the condition to be managed by experts. When food becomes available, it should be given by mouth in small, frequent amounts at first, using a suitable formula preparation .
F-75 is prepared from milk powder (25 g), sugar (70 g), cereal flour (35 g), vegetable oil (27 g) and vitamin and mineral supplements, made up to 1 L with water.
F-100 (1 L) contains milk powder (80 g), sugar (50 g), vegetable oil (60 g) and vitamin and mineral supplements (no cereal).
Individual energy requirements can vary by 30%. During rehabilitation, more concentrated formula can be given with additional food that is palatable and similar to the usual staple meal.
Salt should be restricted and micronutrient supplements (e.g. potassium, magnesium, zinc and multivitamins) may be essential.
Between 6.3 and 8.4 MJ/day (1500–2000 kcal/day) will arrest progressive under-nutrition but additional energy may be required for regain of weight.
During refeeding, a weight gain of 5% body weight per month indicates satisfactory progress..
Other care is supportive and includes:-
• Attention to the skin
• Adequate hydration
• Treatment of infections and
• Careful monitoring of body temperature, since thermoregulation may be impaired.
Circumstances and resources are different in every famine but many problems are non-medical and concern organisation, infrastructure, liaison, politics, procurement, security and ensuring that food is distributed on the basis of need.
Lastly, plans must be made for the future for prevention and/or earlier intervention if similar circumstances prevail.
Under-nutrition in hospital
In the general UK population, 30% of those requiring acute admission to hospital show evidence of serious under-nutrition and 65% of those admitted will lose an verage of 5% of their total body weight during that admission.In the older population, levels of under-nutrition and vitamin deficiencies parallel levels of independent living. In Scotland, 33% of those aged over 65 who are living in their own home are deficient in folic acid and 10% are deficient in vitamin C.
The prevalence of vitamin deficiencies rises further in less independent groups in residential or nursing homes.
Under-nutrition is poorly recognized in hospitals and has serious consequences:-
Physical effects include impaired immunity and muscle weakness, which in turn affect cardiac and respiratory function, and delayed wound healing after surgery with increased risks of post-operative infection.The under-nourished patient is often withdrawn and this may be mistaken for depressive illness. Engagement with treatment and rehabilitation can be adversely affected.
Much of this can be avoided through better awareness of the prevalence of under-nutrition, prompt nutritional assessment and monitoring with appropriate intervention.
Scoring systems, such as the MUST tool, raise awareness across multidisciplinary teams, and encourage staff to assess and monitor food intake and weigh patients regularly. Causes are often complex.
Social issues impact on food choices and may cause or exacerbate disease.
Social isolation, low levels of disposable income and a lack of knowledge or interest in healthy eating may increase reliance on calorie-dense convenience foods of poor nutritional quality.
In turn, the non-specific effects of
• chronic inflammation
• infection or malignancy, as well as
• specific gastrointestinal disorders, may adversely affect appetite, reducing food intake.
Patients may report avoidance of certain foods that exacerbate their symptoms (often fibre-rich, otherwise healthy foods).
Factors affecting adequacy of nutritional intake in hospitalised patients
Factors affecting appetite• Altered taste
• Nausea and/or vomiting
• Non-specific effects of illness and/or drugs
Issues of quantity
• Is there enough food on the plate?
• Social, cultural, financial, general and mental health issues may all be relevant, individually or in combination
Getting the food from the plate to the mouth
• Generalised reduced mobility
• Reduced manual dexterity
• Loss of limb function
Difficulties chewing the food
• Poorly fitting dentures• Pain in the oral cavity
Specific problems with GIT
• Obstruction
• Ischaemia
• Inflammation
• Malabsorption
Cultural issues
• Is the food provided appropriate to the patient’s beliefs?
More general evidence of self-neglect
• Evidence of chronic coexisting illness
• Evidence of mental health problems – low mood may be ‘cause’ or ‘effect’ in under-nutrition
Specific issues arising after intestinal surgery
Gastrectomy or partial gastrectomy
• There may be a loss of gastric capacity, leading to intolerance of larger volumes of food and early satiety or vomiting.
• Vagotomy and gastroenterostomy may cause symptoms of dumping syndrome, which can lead to food avoidance and weight loss.
• Many patients who have had gastric surgery will develop iron deficiency (and, less commonly, vitamin D and vitamin B12 deficiency) unless adequately supplemented post-operatively.
Proximal small bowel surgery
Those who have had roux-en-Y reconstruction or have blindending or excluded loops of small bowel are prone to small intestinal bacterial overgrowth. This may impair absorption of iron, folic acid and vitamin B12. Very rarely, it can cause
hyperammonaemia and metabolic coma, in which bacterial metabolism of amino acids leads to a lack of citrulline and impairment of the urea cycle.
• small intestinal bacterial overgrowth
• Impair absorption of iron, folic acid and vitamin B12
• Hyperammonaemia and metabolic coma
•
Pancreatic resection/Whipple’s operation:-
Without adequate post-operative supplementation, this can be a very serious insult to the digestive tract. There is loss of pancreatic exocrine function (causing steatorrhoea and malabsorption of protein, fats and fat-soluble vitamins), as well as the potential for small intestinal bacterial overgrowth (malabsorption of iron, folic acid and vitamin B12 ).• Steatorrhoea and malabsorption of protein, fats and fat-soluble vitamins), as well as the
• Potential for small intestinal bacterial overgrowth (malabsorption of iron, folic acid and vitamin B12 ).
Ileal resection
May give rise to vitamin B12 deficiency and, rarely, to steatorrhoea and malabsorption of fat-soluble vitamins.
Massive small bowel resection
This may cause short bowel syndrome and intestinal failure, with impaired ability to absorb fluids, electrolytes and macronutrients adequately without parenteral support.
An approach to assisted nutrition in hospital patients
Once the problems leading to under-nutrition have been recognised, it is important to make an individualized plan to address these issues specifically.In most cases, this means a decision to intervene, to tackle and reverse nutritional difficulties. This may involve simply ensuring that adequate supplies of food are delivered and prepared regularly or that dentures fit properly, but may require an assessment of a patient’s ability to swallow or of the intestine’s ability to digest foods. This must include consideration of the potential for disruption of the normal physiology of absorption and digestion in the context of the patient’s medical and surgical history.
Whenever possible, it is best to use the most physiological means of feeding, reserving more invasive interventions for when normal physiological mechanisms of swallowing and digestion are impaired or absent.
Enteral feeding is preferred to parenteral, provided the intestine is accessible and functioning.
Refeeding syndrome
In severely malnourished individuals, attempts at rapid correction of malnutrition switch the body from a reliance on fat to carbohydrate metabolism.Release of insulin is triggered, shifting potassium, phosphate and magnesium into cells (with water following the osmotic gradient) and causing potentially fatal shifts of fluids and electrolytes from the extracellular to the intracellular compartment. Rapid depletion of (already low) thiamin exacerbates the condition.
Release of insulin
shifting potassium, phosphate and magnesium into cells
Clinical features include nausea, vomiting, muscle weakness, seizures, respiratory depression, cardiac arrest and sudden death.
The risks of refeeding are greatest in those who are most malnourished (especially chronic alcoholics), but even those who have gone without food for 5 days can be at risk and restitution of feeding should always be done slowly, with careful monitoring of serum potassium, phosphate and magnesium in the first 3–5 days
Oral nutritional supplements
Poor appetite, immobility, poor dentition or even being kept ‘nil by mouth’ for hospital procedures all contribute to weight loss. As a first step, patients should be encouraged and helped to eat an adequate amount of normal food.
Where swallow and intestinal function remain intact, the simplest form of assisted nutrition is the use of oral nutritional supplements.
Most branded products are nutritionally complete (fortified with the daily requirements of vitamins, minerals and trace elements).
They most often come in the form of liquid drinks but various formulations and textures exist, including ‘shakes’ and ‘puddings’ with a thicker consistency.
They are cost-effective and very useful for people who may require just a small number of additional calories each day to maintain or gain weight in the short or longer term.
However, in spite of their nutritional value, small volume and range of flavours, many people find them unpalatable or difficult to tolerate.