
External ear diseases
By Firas Al-Hameed
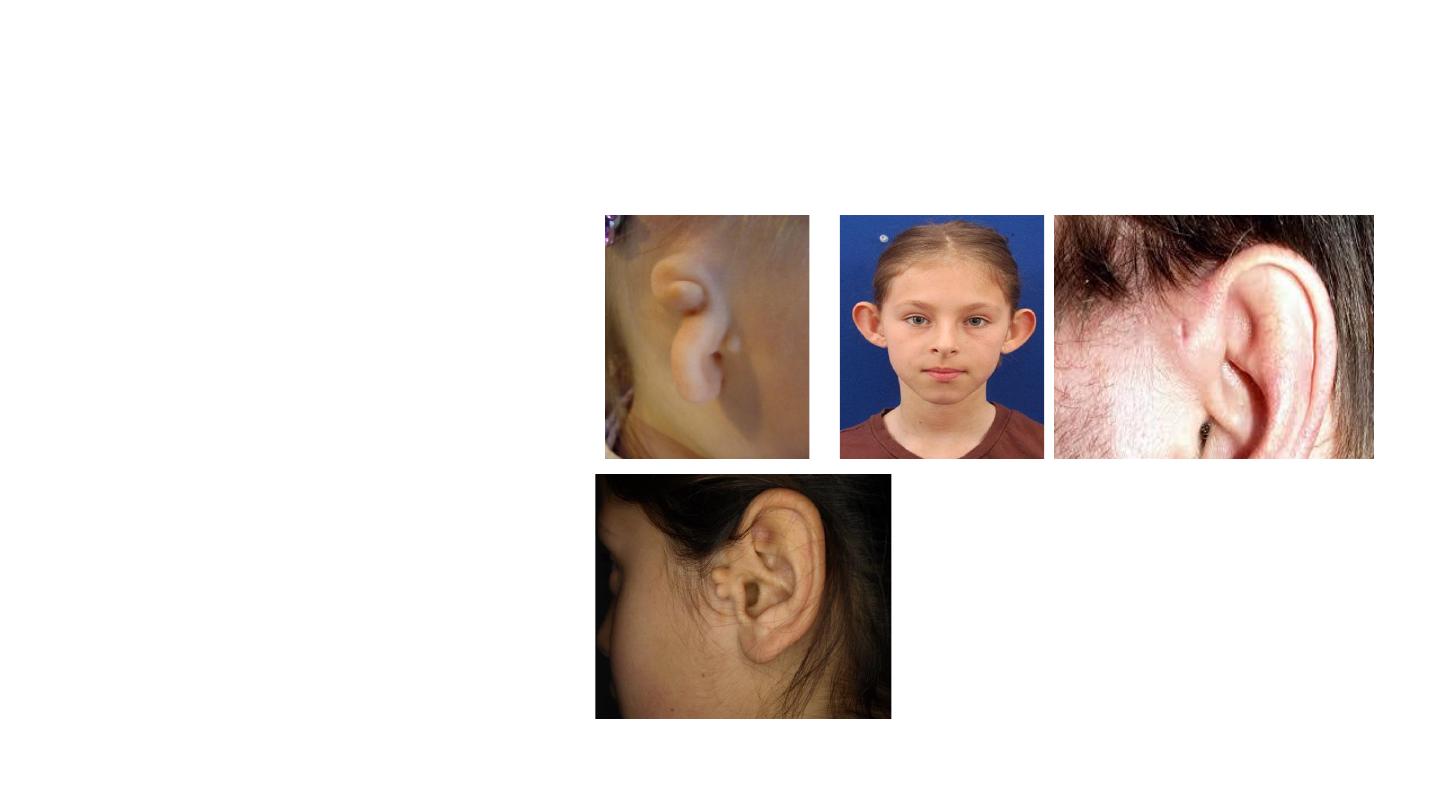
Congenital malformations
• Microtia, aural atresia,
prominent auricles,
preauricular pits, and
accessory auricular
appendages
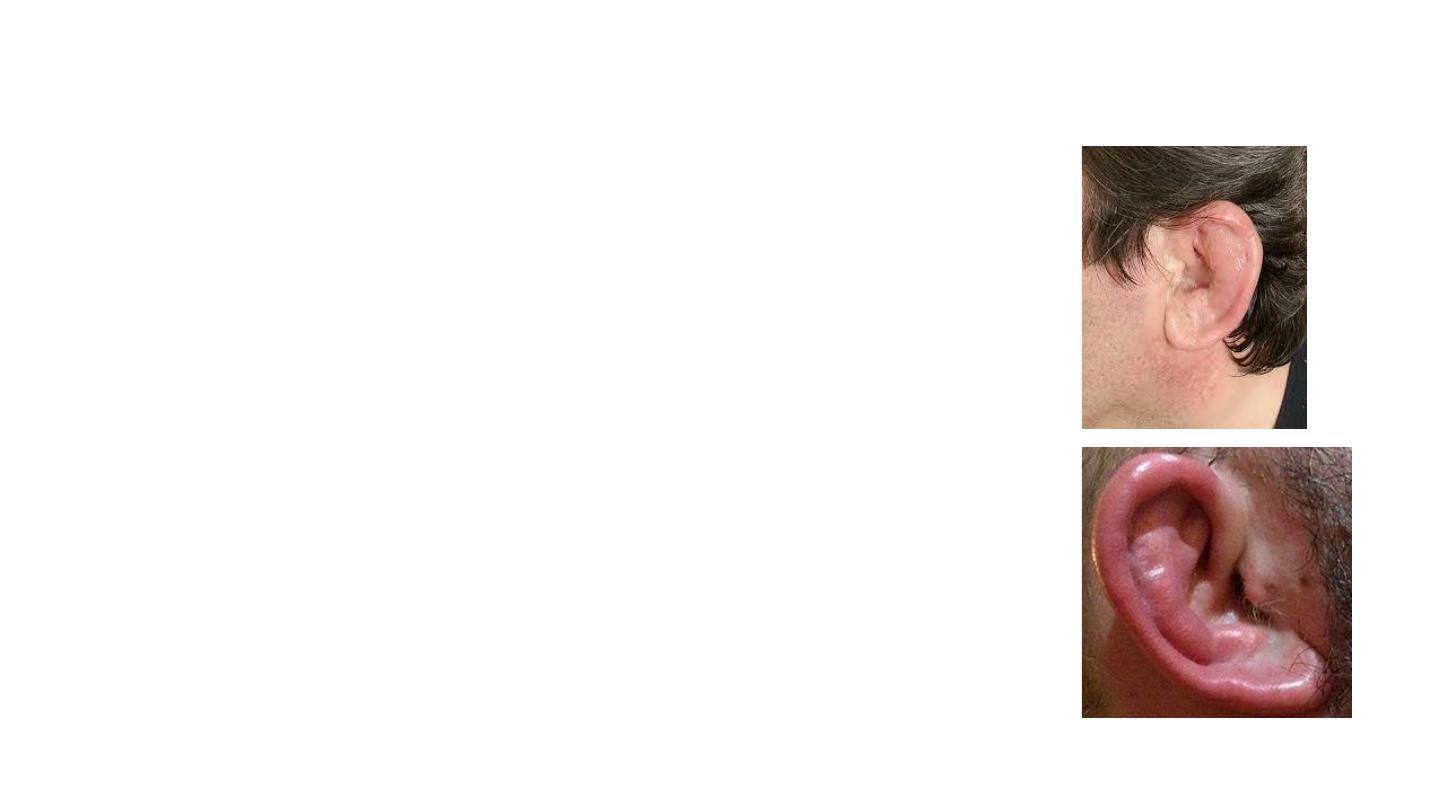
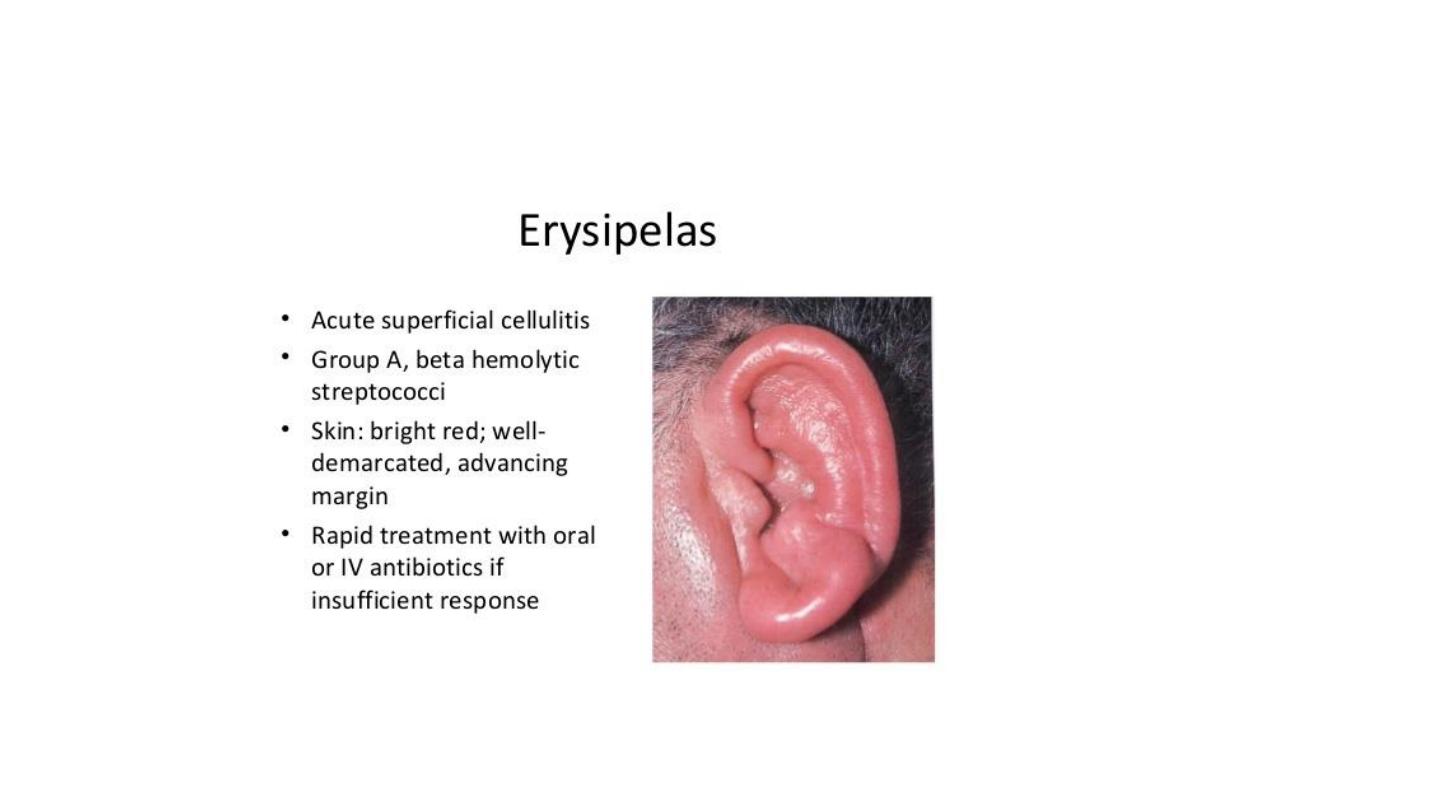
Pinna perichondritis and cellulitis
• Risk factors:
• Complication of acute otitis externa, eczema or
psoriasis, or from an insect bite.
• penetrating trauma, including ear piercing
Examination:
Cellulitis: Infection involve the whole pinna
Perichondritis: Spare earlobe
• Causative organism:
• Cellulitis it can be Staphylococcus aureus or
other skin organisms
• Perichondritis: Pseudomonas aeruginosa
• Management:
• Oral fluoroquinolones or co-amoxiclav
• Topical fusidic acid cream may help treat
staphyloccocal infection
• DDX: Relapsing perichondritis
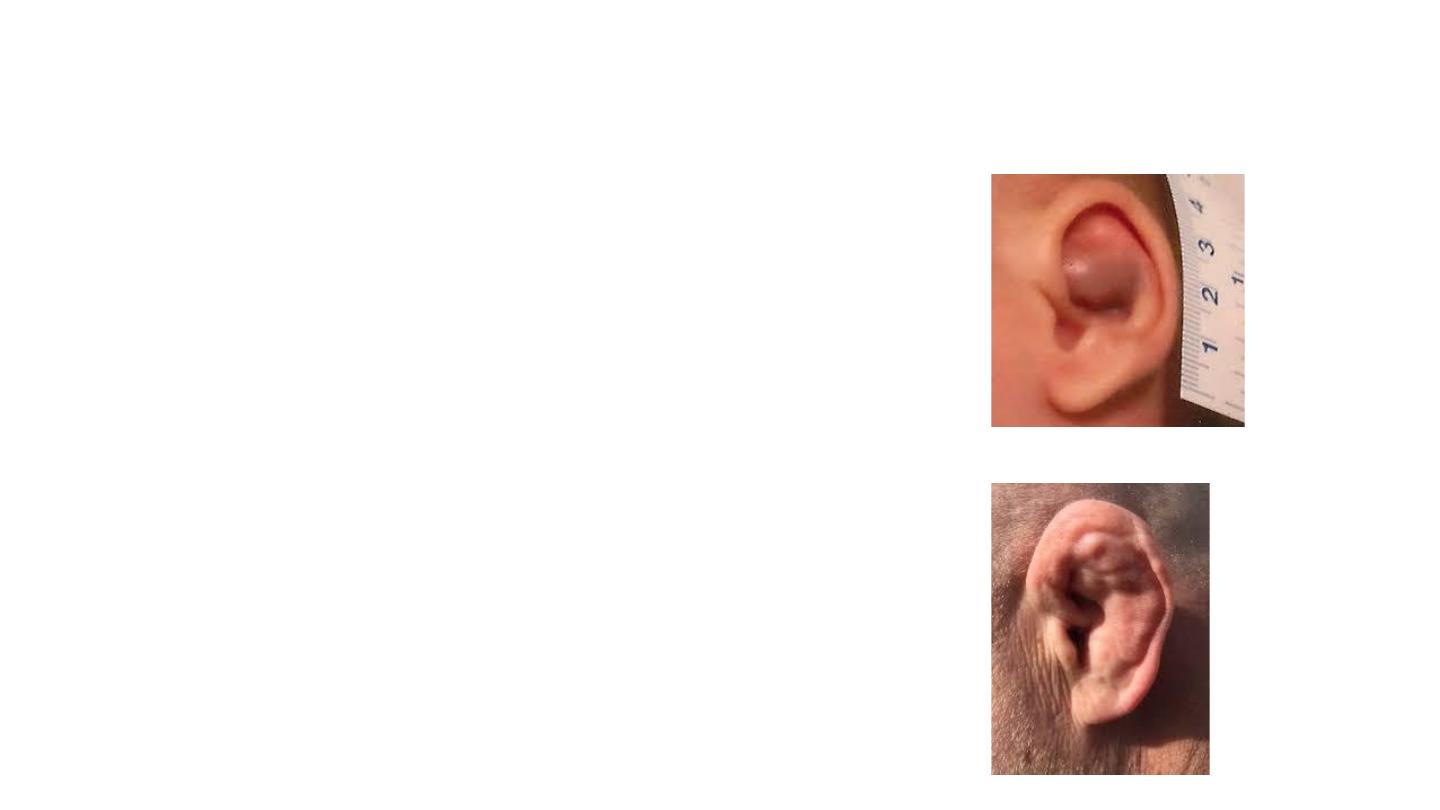
Pinna haematoma
• Collection of blood between the auricular
perichondrium and cartilage.
• Blunt injury (contact sports or assaults)
• Management:
• Drainage of the haematoma either by
aspiration or by incision followed by
compression.
• Broad-spectrum antibiotics are prescribed if
there is delayed presentation and high risk of
infection

Ear wax
• Desquamated keratin mixed with lipid and peptide
secretions from sebaceous and ceruminous glands,
respectively
• It has a protective role in the EAC (pH5.0–7.0)
• May become impacted
• migratory function of the EAC is impaired
• pushed medial in the EAC with cotton buds
• Management:
1. Ear syringing
• otitis externa, tympanic membrane perforation or damage to
the EAC.
2. Microscopic or endoscopic removal
Otitis externa
• Inflammation of the skin of the external auditory meatus or the
auricle or the outer surface of the tympanic membrane
• Predisposing Factors
1. Heat, humidity, bathing, swimming.
2. Trauma, especially from dirty fingernails, cotton buds and hairgrips.
3. Inherited—narrow ear canals.
4. Skin conditions—non-atopic eczema, psoriasis
• Classification:
• Acute or chronic,
• Diffuse or localized;
• Infective or reactive

Infective
• Bacterial
• Pseudomonas aeruginosa,
• S. aureus
• Furunculosis, usually caused
by S. aureus.
• Fungal
• Aspergillus niger
• Aspergillus fumigatus
• Candida albicans
• Viral
• Herpes simplex
• Herpes zoster
Reactive
–– Eczema.
–– Seborrhoeic dermatitis.
–– Neuro dermatitis.
–– Keratosis obturans.
–– Psoriasis.
–– Secondary to discharge from
an acute or chronic otitis media

Otitis externa
Examination:
Pinna/ tragus tender
EAC filled with
discharge
EAC swollen
Mycotic debris (‘
wet
cotton wool’ appearance or
the presence
of fungal hyphae)
TM often not seen
History:
Ear pain
Discharge
Itching
Sense of blockage
Hearing loss
Medical history
Diabetes
Skin diseases
Investigations
An ear swab for
microbiological culture,
including
fungal culture, and
antibiotic/antimycotic
sensitivity

Management
• Keep ears dry
• Analgesia
• Topical antibiotics + steroid
• Aural toilet
• Ear canal dressing
• In severe cases, particularly when there is a lot of pain and oedema
• expandable otowick can be used.
• An alternative strategy, particularly in resistant cases,
• is 12-mm ribbon gauze, impregnated with an antibiotic and steroid
• cream or ointment
• Systemic antibiotics
• Adjacent cellulitis involving the skin of the pinna or cheek.
• Immunosuppression
• Local factors that hinder the delivery of topical preparations.

Complications of acute OE
• Necrotising otitis externa (NOE; previously known as malignant otitis
externa)
• Abscess formation
• Peri-auricular or pinna cellulitis
• Chronic stenosis of the ear canal or false fundus
Malignant (or Necrotising)
Otitis Externa
• Otitis externa which progresses to an osteomyelitis initially
of the tympanic plate which then may spread to involve the
skull base and petrous portion of the temporal bone.
• P. aeruginosa
• Elderly patients with diabetes or those who are
immunocompromised
• Constant deep and severe otalgia
• Granulations over the deep ear canal
• May cause 7th to 12th cranial nerve palsies, meningitis,
sigmoid sinus thrombosis, brain abscess and
death
.

• Diagnosis is clinical
• High-definition computed tomography (CT) or(MRI) scans of the skull
base
• Blood sugar, C-reactive protein , ESR and full blood count
• Treatment: IV antibiotics for 6-12 weeks and monitored by the
improving CRP and ESR

Differential diagnoses
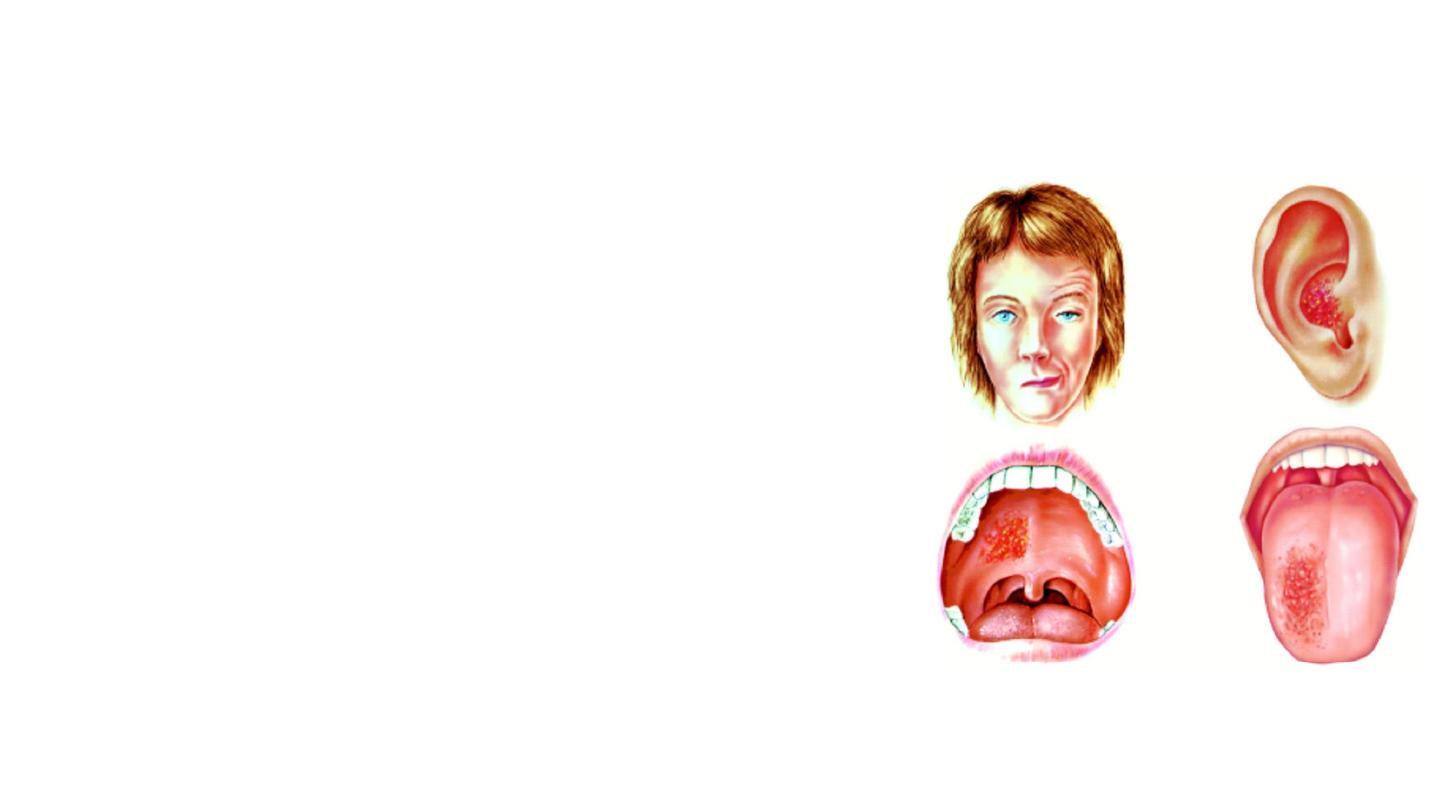
Otomycosis
• Aspergillus or Candida species.
• At least 10 percent of otitis externa is caused by fungal infection.
• It is best treated by repeated careful microsuction and topical
antifungals for no less than 2 weeks.
Furunculosis
• Lateral third of the canal.
• Staphylococcus aureus.
• Severe pain
• The abscesses may rupture or need to be incised and drained to
give relief.
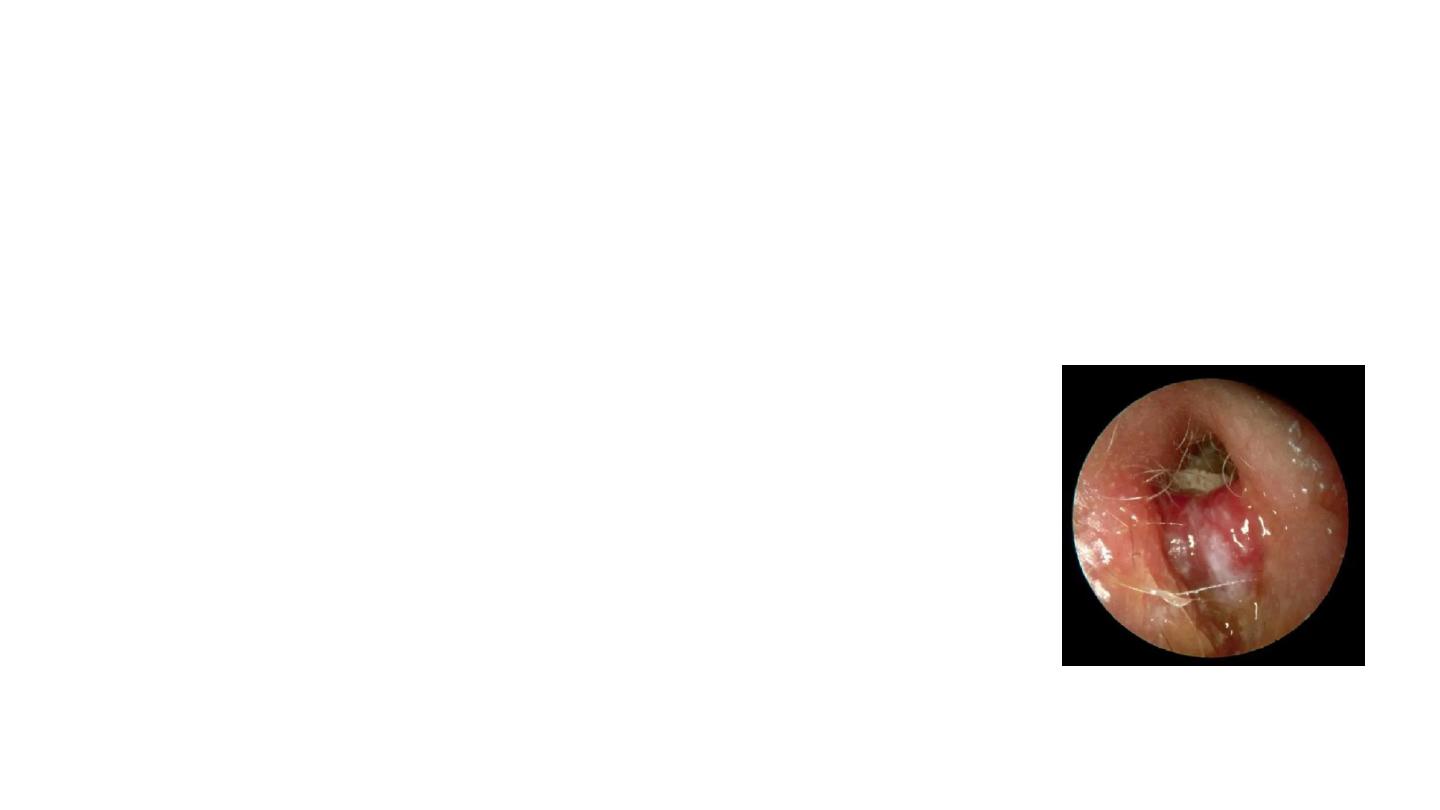
Herpes zoster oticus (Ramsay Hunt Syndrome)
• Varicella-zoster virus
• Unilateral marked otalgia and facial paralysis
accompanied by a vesicular rash in the
external ear
• Distributions of vesicles
• Sensorineural hearing loss, vertigo and
tinnitus.
• Management:
• Early urgent treatment with antivirals and
steroids is essential
• Analgesia
• Eye care
Myringitis
• Inflammation of the tympanic membrane.
• Granular myringitis:
• History of trauma to outer surface of TM.
• Recurrent episodes of painless otorrhea, ear
fullness or ear blockade. Hearing is normal or
mild conductive hearing loss.
• Examination: granular areas over the TM
• Treatment: Topical anti pseudomonal
antibioitics +/- steroid,
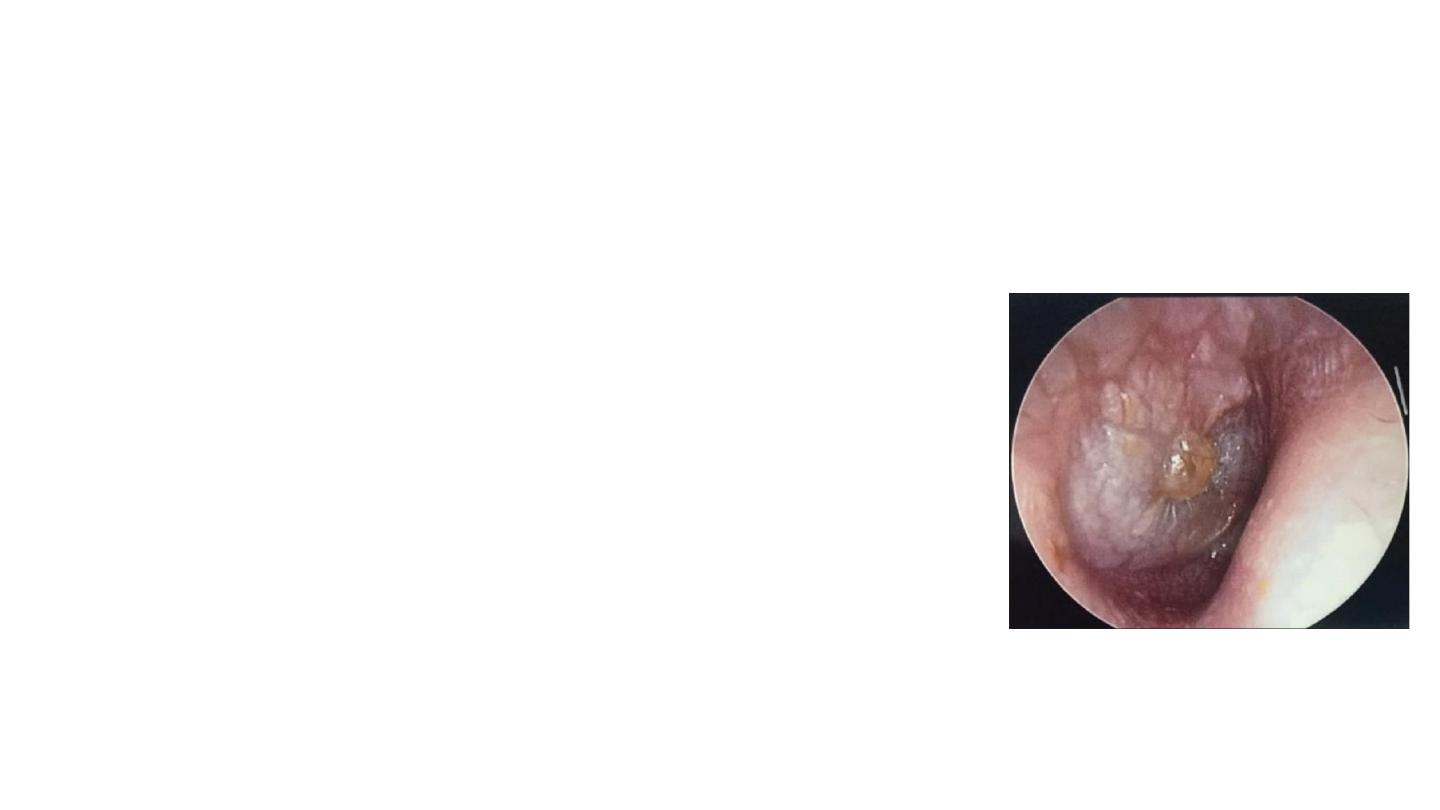
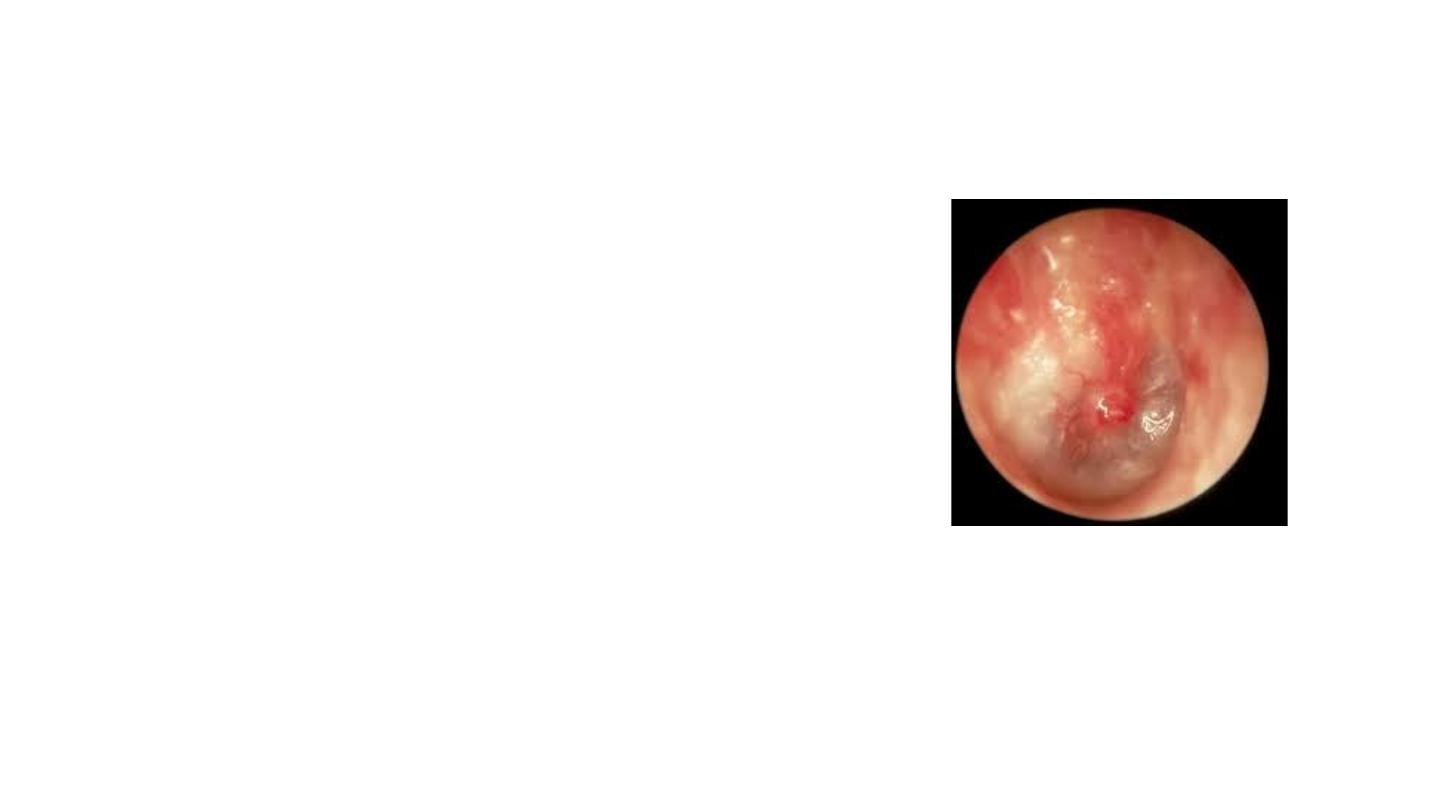
Bullous myringitis
• Due to infection (viral)
• More common in children and in winter
• Sudden onset severe pain
• hearing: normal and can be conductive hearing
loss. Over half of the patients with bullous
myringitis demonstrate sensorineural hearing
changes.
• Bubbles filled with blood on the surface of the
tympanic membrane that can burst; however, the
tympanic membrane itself is not perforated.
• Treatment: analgesia, topical antibiotics
