The gall bladder and bile ducts Surgery Dr. Muhanned
Surgical anatomy
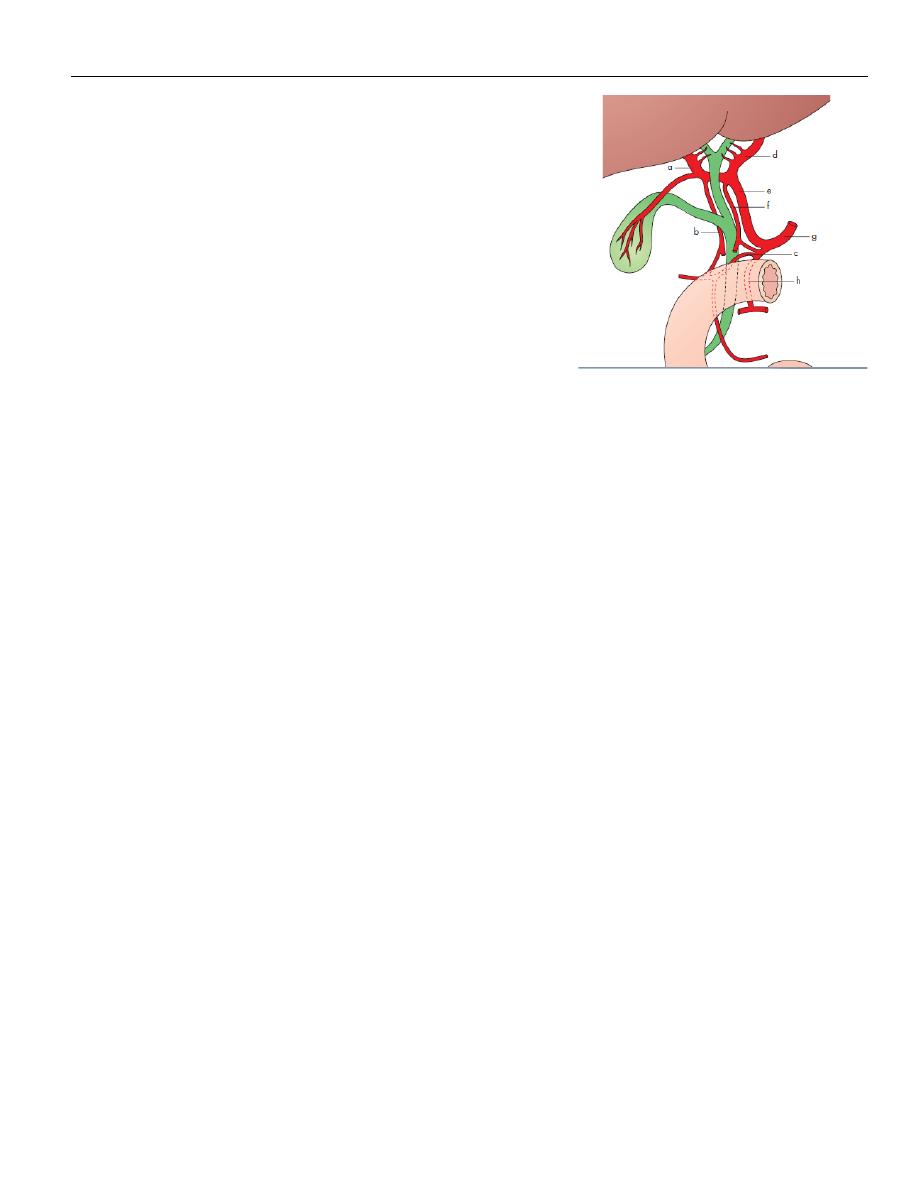
The gall bladder lies on the underside of the liver at the
junction of the right and left lobes of the liver. The
relationship of the gall bladder to the liver varies
between being embedded within the liver substance to
suspended by a mesentery. it is a pear-shaped structure,
7.5–12
cm
long,
with
a
normal
capacity
of about 35–50 ml. The anatomical divisions are a fundus,
a body and a neck that terminates in a narrow
infundibulum.
The
cystic
duct
is
about
3
cm
in
length
but
variable.
Its
lumen
is usually 1–3 mm in diameter. Its wall is surrounded by a sphincteric structure called the
sphincter of Lütkens. While the cystic duct joins the common hepatic duct in its
supraduodenal segment in 80% of cases, it may extend down into the retroduodenal or even
retropancreatic part of the bile duct before joining.
The common hepatic duct is usually less than 2.5 cm long and is formed by the union of the
right and left hepatic ducts. The common bile duct is about 7.5 cm long and is formed by the
junction of the cystic and common hepatic ducts. It is divided into four parts:
• the supraduodenal portion, about 2.5 cm long,
• the retroduodenal portion;
• the infraduodenal portion, on the posterior surface of the pancreas;
• the intraduodenal portion, which passes obliquely through the wall of the second part of
the duodenum, where it is surrounded by the sphincter of Oddi, and terminates by opening
on the ampulla of Vater.
The cystic artery, a branch of the right hepatic artery, Occasionally,. In 15% of cases, the
right hepatic artery and/or the cystic artery cross in front of the common hepatic duct and
the cystic duct. The most dangerous anomalies are where the hepatic artery takes a tortuous
course on the front of the origin of the cystic duct, or the right hepatic artery is tortuous and
the cystic artery short. The tortuosity is known as the ‘caterpillar turn’ .

Lymphatics
The lymphatic vessels of the gall bladder drain into the cystic lymph node of Lund . This lies in
the fork created by the junction of the cystic and common hepatic ducts. The subserosal
lymphatic vessels of the gall bladder also connect with the subcapsular lymph channels of the
liver.
Surgical physiology
Bile, as it leaves the liver, is composed of 97% water, 1–2% bile salts and 1% pigments,
cholesterol and fatty acids. The liver excretes bile at a rate estimated to be approximately 40
ml h–1.
The rate of bile secretion is controlled by cholecystokinin (CCK), which is released from the
duodenal mucosa. With feeding, there is increased production of bile.
FUNCTIONS OF THE GALL BLADDER
The gall bladder is a reservoir for bile. During fasting, resistance to flow through the sphincter
is high, and bile excreted by the liver is diverted to the gall bladder.
The second main function of the gall bladder is concentration of bile by active absorption of
water, sodium chloride and bicarbonate by the mucous membrane of the gall bladder.
The third function of the gall bladder is the secretion of mucus – approximately 20 ml is
produced per day.
RADIOLOGICAL INVESTIGATION OF THE BILIARY TRACT
Plain radiograph
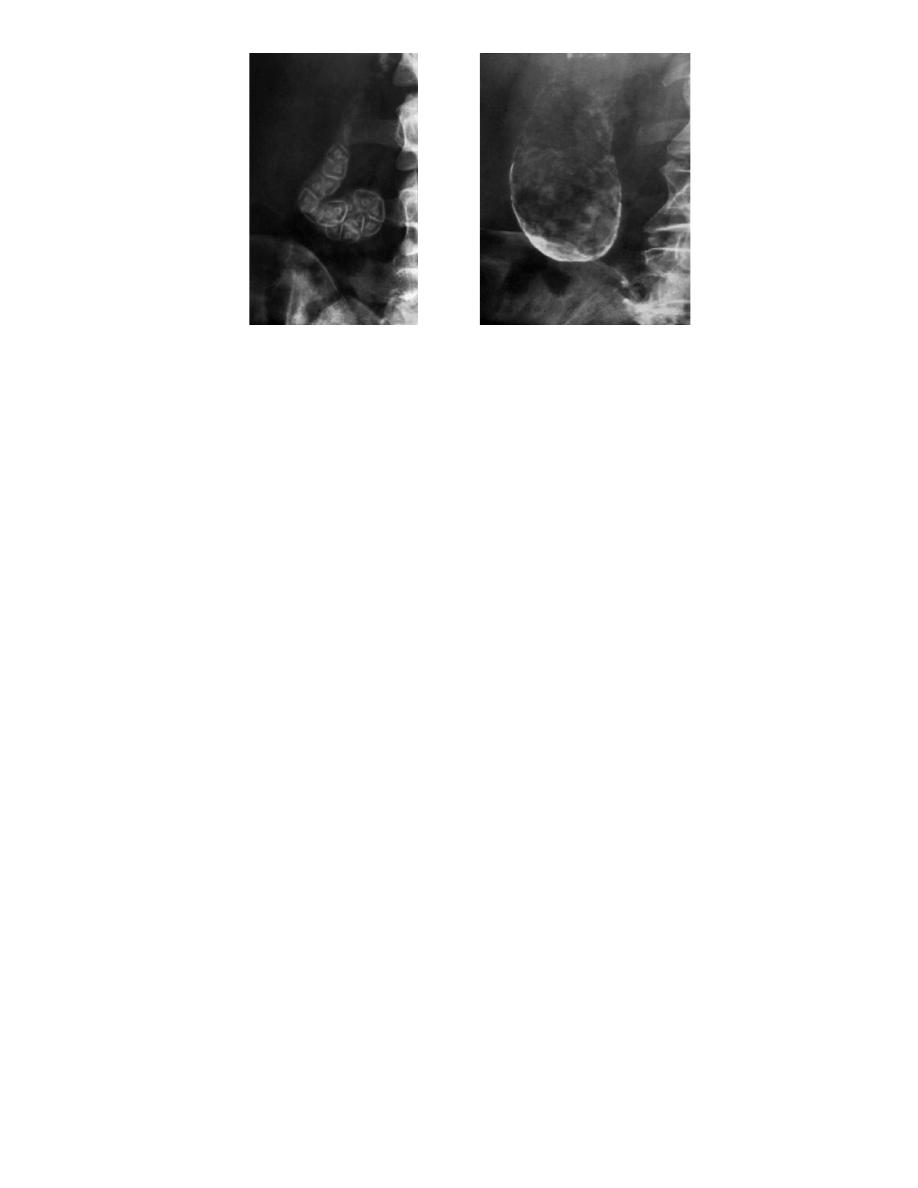
A plain radiograph of the gall bladder will show radio-opaque gallstones in 10% of patients
with gallstones . Rarely, the centre of a stone may contain radiolucent gas ‘Mercedes-Benz’
sign in the A plain X-ray may also show the rare cases of calcification of the gall bladder, a so
called ‘porcelain’ gall bladder .
The importance of this appearance is an association with carcinoma in up to 25% of patients.
Gas may be seen in the wall of the gall bladder (emphysematous cholecystitis). Gas in the
biliary tree may be seen after endoscopic sphincterotomy or surgical anastomosis
Oral cholecystography and intravenous cholangiography
Oral and intravenous cholecystography are of historical interest only .
Ultrasonography
Transabdominal ultrasonography is the initial imaging modality of choice as it is accurate,
readily available, inexpensive and quick to perform. However, it is operator dependent and
may be suboptimal due to excessive body fat and intraluminal bowel gas. It can demonstrate
biliary calculi, the size of the gall bladder, the thickness of the gall bladder wall, the presence
of inflammation around the gall bladder, the size of the common bile duct and, occasionally,
the presence of stones within the biliary tree.
In the patient who presents with obstructive jaundice, ultrasonography can identify
- intra- and extrahepatic biliary dilatation and the level of obstruction.
- the cause of the obstruction may also be identified, such as gallstones in the gall bladder,
common hepatic or common bile duct stones or lesions in the wall of the duct suggestive of a
cholangiocarcinoma or enlargement of the pancreatic head Endoscopic ultrasonography
uses a specially designed endoscope with an ultrasound transducer at its tip, which allows
visualisation of the liver and biliary tree from within the stomach and duodenum. it useful in
detecting stones within the bile ducts( choledocholithiasis). In addition, it has been shown to
be highly accurate in diagnosing and staging both pancreatic and periampullary cancers.
Radioisotope scanning (scintigraphy )
Technetium-99m (99mTc)-labelled derivatives of iminodiacetic acid (HIDA scan ) when
injected intravenously, selectively taken up by the retroendothelial cells of the liver and
excreted into bile. This allows visualisation of the biliary tree and gall bladder.

Non-visualisation of the gall bladder is suggestive of acute cholecystitis. If the patient has a
contracted gall bladder, as often occurs in chronic cholecystitis, gall bladder visualisation may
be reduced or delayed.
Biliary scintigraphy may also be helpful in diagnosing bile leaks and iatrogenic biliary
obstruction. When there is a suspicion of a bile leak following a cholecystectomy,
radioisotope imaging should be performed.
Computerised tomography
This imaging modality allows visualisation of the liver, bile ducts, gall bladder and pancreas. It
is particularly useful in detecting hepatic and pancreatic lesions and is the modality of choice
in the staging of cancers of the liver, gall bladder, bile ducts and pancreas. It can identify the
extent of the primary tumour and defines its relationship to other organs and blood vessels .
In addition, the presence of enlarged lymph nodes or metastatic disease can be seen.
For benign biliary diseases, computerised tomography is not that useful an investigation.
Gallstones are usually not visualised Magnetic resonance cholangiopancreatography. It is
non-invasive , Contrast is not required and, excellent images can be obtained of the biliary
tree that demonstrate ductal obstruction, strictures or other intraductal abnormalities.
Endoscopic retrograde cholangiopancreatography
This technique remains widely used. Using a side-viewing endoscope, the ampulla of Vater
can be identified and cannulated.
Injection of water-soluble contrast directly into the bile duct provides excellent images of the
ductal anatomy and can identify causes of obstruction such as stones or malignant strictures
, Bile can be sent for cytological and microbiological examination, and brushings can be
taken from strictures for cytological studies. Therapeutic interventions such as stone removal
or stent placement to relieve the obstruction can be performed. Thus, ERCP has evolved into
a mainly therapeutic rather than a diagnostic uses .

Percutaneous transhepatic cholangiography
This is an invasive technique in which the bile ducts are cannulated directly. It is only done
once a bleeding tendency has been excluded, Antibiotics should be given prior to the
procedure. Usually,, a needle is introduced percutaneously into the liver substance. Under
radiological control (either ultrasound or CT), a bile duct is cannulated. Successful entry is
confirmed by aspiration of bile. Water-soluble contrast medium is injected to demonstrate
the biliary system. In addition, PTC enables the placement of a catheter into the bile ducts to
provide external biliary drainage or the insertion of stents.
Peroperative cholangiography
During open or laparoscopic cholecystectomy, a catheter can be placed in the cystic duct and
contrast injected directly into the biliary tree. The technique defines the anatomy and is
mainly used to exclude the presence of stones within the bile ducts .
Operative biliary endoscopy (choledochoscopy)
At operation, a flexible fibreoptic endoscope can be passed down the cystic duct into the
common bile duct enabling stone identification and removal under direct vision. After
exploration of the bile duct, a tube can be left in the cystic duct remnant or in the common
bile duct (a T-tube) and drainage of the biliary tree established. After 7–10 days, a track will
be established. This track can be used for the passage of a choledochoscope to remove
residual stones .
CONGENITAL ABNORMALITIES OF THE GALL BLADDER AND BILE DUCTS
Embryology
Absence of the gall bladder
Occasionally, the gall bladder is absent. Failure to visualise the gall bladder is not necessarily
a pathological problem.
The Phrygian cap
The Phrygian cap is present in 2–6% and may be mistaken for a pathological deformity of the
organ. ‘Phrygian cap’ refers to hats worn by the people of Phrygia.
Floating gall bladder
The organ may hang on a mesentery, which makes it liable to undergo torsion.
Double gall bladder
Rarely, the gall bladder is duplicated.
Absence of the cystic duct
This is usually a pathological, anomaly and indicates the
recent passage of a stone or the presence of a stone at
the lower end of the cystic duct, which is ulcerating into
the common bile duct. The main danger at surgery is
damage to the bile duct.
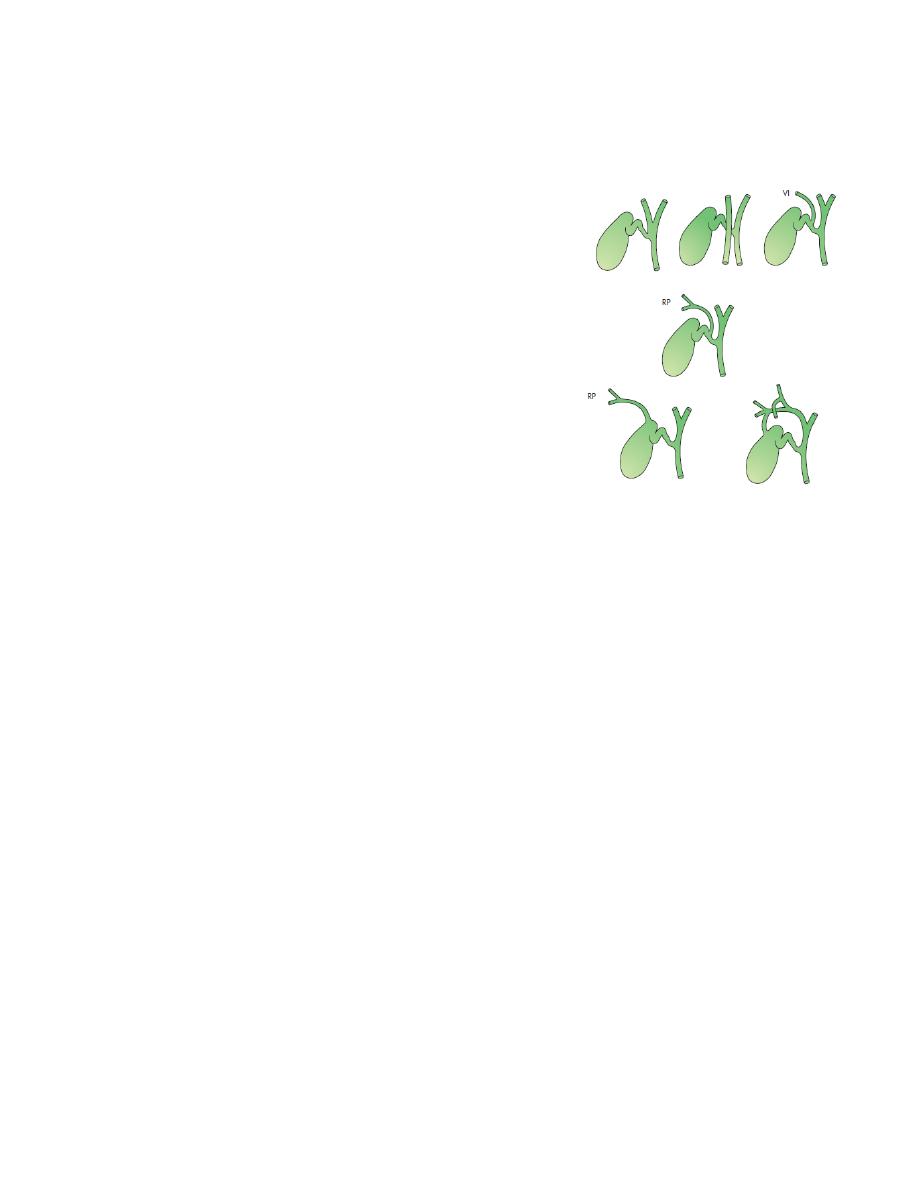
Low insertion of the cystic duct
The cystic duct opens into the common bile duct near the
ampulla.
All variations of this anomaly can occur .
An accessory cholecystohepatic duct
Ducts passing directly into the gall bladder from the liver do occur .
EXTRAHEPATIC BILIARY ATRESIA
Aetiology and pathology
Atresia is uncommon affects males and females equally. The extrahepatic bile ducts are
progressively destroyed by an inflammatory process, which starts around the time of birth.
eventually result in biliary cirrhosis and portal hypertension. Untreated, death from the
consequences of liver failure occurs before the age of 3 years.
The inflammatory destruction of the bile ducts has been classified into three main types
• type I: atresia restricted to the common bile duct;
• type II: atresia of the common hepatic duct;
• type III: atresia of the right and left hepatic ducts.

Clinical features
About one-third of patients are jaundiced at birth. In all, however, jaundice is present by the
end of the first week and deepens progressively. The meconium may be a little bile-stained,
but later the stools are pale and the urine is dark. Pruritus is severe. Clubbing and skin
xanthomas.
Differential diagnosis
This includes any form of jaundice in a neonate giving a cholestatic picture. Examples are
alpha-1-antitrypsin deficiency, cholestasis associated with intravenous feeding, choledochal
cyst and inspissated bile syndrome. Neonatal hepatitis is the most difficult to differentiate.
Liver biopsy and radioisotope scans are essential
Treatment
Patent segments of proximal bile duct are found in 10% of type I lesions. A direct Roux-en-Y
hepaticojejunostomy will achieve bile flow in 75%, but progressive fibrosis results in
disappointing long term results. A simple biliary–enteric anastomosis is not possible in the
majority of cases in which the proximal hepatic ducts are either very small (type II) or atretic
(type III). These are treated by the Kasai procedure. Liver transplantation should be
considered in children in whom a portoenterostomy is unsuccessful Postoperative
complications include bacterial cholangitis. Repeated attacks lead to hepatic fibrosis, portal
hypertension, with one-third having variceal bleeding.
CONGENITAL DILATATION OF THE INTRAHEPATIC DUCTS (CAROLI’S DISEASE)
This rare condition is characterised by multiple irregular saccular dilatations of the
intrahepatic ducts with a normal extrahepatic biliary system. The aetiology is unknown, but
it is considered to be hereditary. It can be divided into a simple and a periportal fibrotic
type. The periportal fibrotic type presents in childhood and is associated with biliary stasis,
stone formation and cholangitis. In contrast, the simple type presents later with episodes of
abdominal pain and biliary sepsis. Associated conditions include congenital hepatic fibrosis,
polycystic liver
treatment are antibiotics for the cholangitis and the removal of calculi, lobectomy may be
indicated.
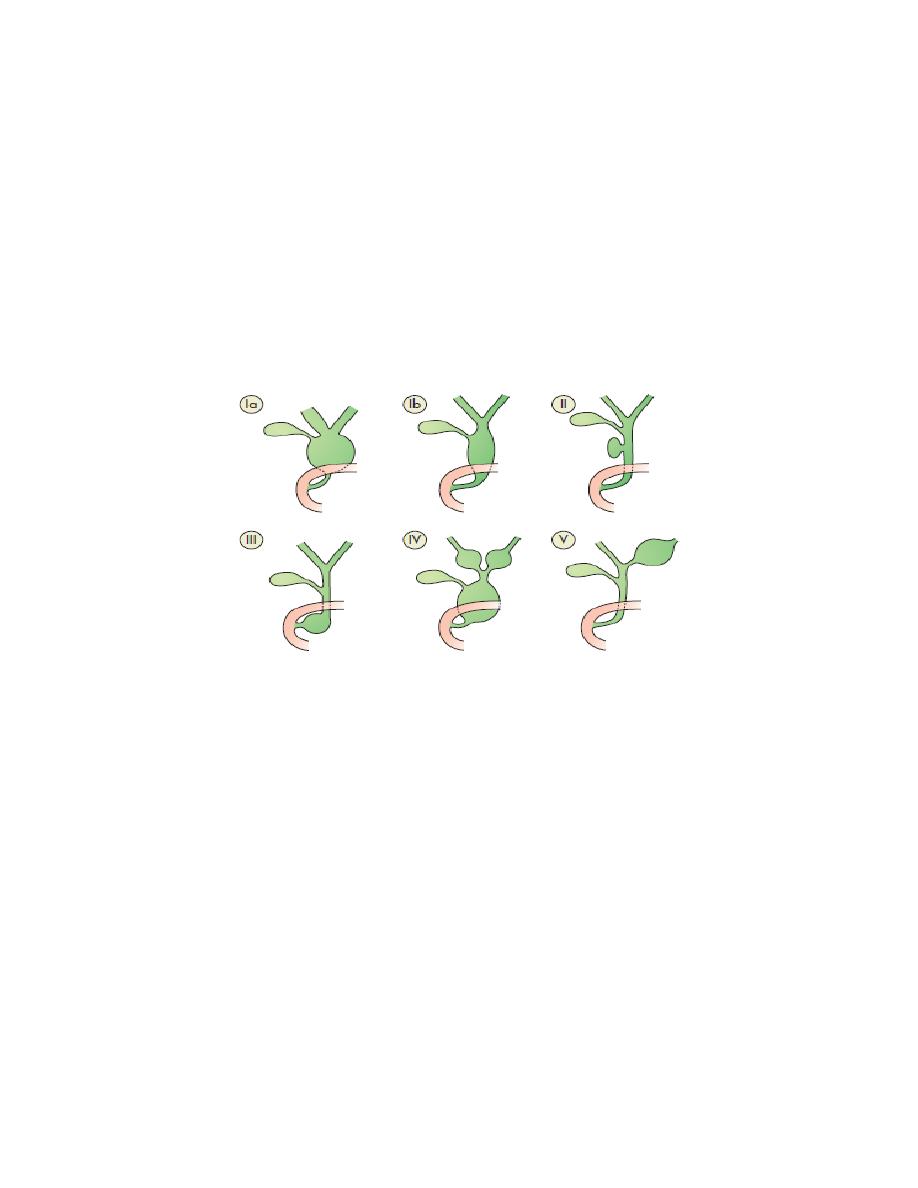
Choledochal cyst
Choledochal cysts are congenital dilatations of the intra- and/or extrahepatic biliary system.
The pathogenesis is unclear. Type I cysts are the most common 75% of patients.
Patients may present at any age with jaundice, fever, abdominal pain and a right upper
quadrant mass on examination. Pancreatitis is a not infrequent presentation in adults.
Patients with choledochal cysts have an increased risk of developing cholangiocarcinoma .
Ultrasonography will confirm the presence of an abnormal cyst and magnetic resonance
imaging (MRI/MRCP) will reveal the anatomy, CT is also useful for the extent of the intra- or
extrahepatic dilatation.
Type Ia and b: diffuse cystic. Note extension into the pancreas of type Ib. Type II:
diverticulum of the common bile duct. Type III: diverticulum within the pancreas. Type IV:
extension into the liver. Type V: cystic dilatation only of the intrahepatic ducts.
Radical excision of the cyst is the treatment of choice with reconstruction of the biliary tract
using a Roux-en-Y loop of jejunum. Complete resection of the cyst is important because of
the association with the development of cholangiocarcinoma.
TRAUMA
Injuries to the gall bladder and extrahepatic biliary tree are rare.
They occur as a result of blunt or penetrating abdominal trauma.
Operative trauma is perhaps more frequent than external trauma.
The physical signs are those of an acute abdomen.

Management. In the stable patient, a transected bile duct is best repaired by a Roux-en-Y
choledochojejunostomy. Injuries to the gall bladder can be dealt with by cholecystectomy.
TORSION OF THE GALL BLADDER
This occurs mostly in an older patient with a large mucocele of the gall bladder. patient
presents with an acute abdomen.
Immediate exploration and cholecystectomy are indicated.
GALLSTONES (CHOLELITHIASIS)
Gallstones are the most common biliary pathology. It is estimated that gallstones are present
in 10–15% of the adult population in the USA. They are asymptomatic in the majority (>
80%). Approximately 1–2% of asymptomatic patients will develop symptoms requiring
cholecystectomy
Aetiology of gallstones
Gallstones can be divided into three main types:
1. cholesterol
2.pigment (brown/black)
3.mixed stones.
80% are cholesterol or mixed stones, whereas in Asia, 80% are pigment stones. Cholesterol
or mixed stones contain cholesterol plus an admixture of calcium salts, bile acids, bile
pigments and phospholipids
pathogenesis
1- bile is supersaturated with Cholesterol or bile acid concentrations are low, unstable
phospholipid vesicles form, from which cholesterol crystals may nucleate, and stones may
form.
2- Obesity, high-calorie diets and certain medications can increase the secretion of
cholesterol
and
supersaturate
bile,
increasing
the
lithogenicity
of
bile

.3- Abnormal emptying of the gall bladder may promote the aggregation of cholesterol
crystals; hence, removing gallstones without removing the gall bladder inevitably leads to
gallstone recurrence.
Pigment stone is the name used for stones containing less than 30% cholesterol. There are
two types – black and brown. Black stones are largely composed of an insoluble bilirubin
pigment mixed with calcium phosphate and calcium bicarbonate. Black stone associated with
haemolysis, usually hereditary spherocytosis or sickle cell disease. For unclear reasons,
patients with cirrhosis have a higher instance of pigmented stones. Brown stones are rare in
the gall bladder. They form in the bile duct and are related to bile stasis and infected bile
Clinical presentation
Patients typically complain of right upper quadrant or epigastric pain, which may radiate to
the back. This may be described as colicky, but more often is dull and constant. Other
symptoms include dyspepsia, flatulence, food intolerance, particularly to fats, and some
alteration in bowel frequency.
Biliary colic is typically present in 10–25% of patients. associated with nausea and vomiting.
Pain may radiate to the chest. The pain is usually severe and may last for minutes or even
several hours.
Frequently, the pain starts during the night, waking the patient.
Dyspeptic symptoms may coexist and be worse after such an attack. As the pain resolves, the
patient is able to eat and drink again,
When symptoms do not resolve, but progress to continued pain with fever and leucocytosis,
the diagnosis of acute cholecystitis should be considered.

Effects and complications of gallstones
In the gallbladder
Asymtomatic
Biliary colic
Acute cholecystitis
Chronic cholecystitis
Empyema of the gall bladder
Mucocele
Perforation
In the bile ducts
Biliary obstruction
Acute cholangitis
Acute pancreatitis
In the intestine
Intestinal obstruction (gallstone ileus)
Differential diagnosis of cholecystitis
Common
Appendicitis
Perforated peptic ulcer
Acute pancreatitis
Uncommon
Acute pyelonephritis
Myocardial infarction
Pneumonia – right lower lobe
Diagnosis
A diagnosis of gallstone disease is based on the history and physical examination.
In the acute phase, the patient may have right upper quadrant tenderness that is
exacerbated during inspiration by the examiner’s right subcostal palpation (Murphy’s sign). A
positive Murphy’s sign suggests acute inflammation and may be associated with a
leucocytosis and moderately elevated liver function tests.

A mass may be palpable as the omentum walls off an inflamed gall bladder. Fortunately, the
process is limited because stone is slipped back to gall bladder.
If resolution does not occur, an empyema of the gall bladder may result. The wall may
become necrotic and perforate, with the development of localised peritonitis. The abscess
may then perforate into the peritoneal cavity with a generlised peritonitis
A palpable, non-tender gall bladder (Courvoisier’s sign) usually results from a distal common
duct obstruction secondary to a pancreatic malignancy.
Rarely, a non-tender, palpable gall bladder results from complete obstruction of the cystic
duct with reabsorption of the intraluminal bile salts and secretion of uninfected mucus
secreted by the gall bladder epithelium, leading to a mucocele of the gall bladder.
Treatment
it is safe to observe patients with asymptomatic gallstones, with cholecystectomy only being
performed for those patients who develop symptoms or complications . However,
prophylactic cholecystectomy should be considered in diabetic patients, those with
congenital haemolytic anaemia and those due to undergo bariatric surgery
for morbid obesity.
For patients with biliary colic or cholecystitis, cholecystectomy is the treatment of choice in
the absence of medical contraindications.
The timing of surgery in acute cholecystitis remains controversial.
Many favour early operation , whereas others suggest that a delayed approach is preferable.
Conservative treatment followed by cholecystectomy
more than 90% of cases, the symptoms of acute cholecystitis subside with conservative
measures.
Nonoperative treatment is :
1 Nil by mouth (NPO) and intravenous fluid administration.
2 Administration of analgesics.
3 Administration of antibiotics. As the cystic duct is blocked in
most instances, the concentration of antibiotic in the serum is more important than its
concentration in bile. A broadspectrum antibiotic effective against Gram-negative aerobes is

most appropriate (e.g. cefazolin, cefuroxime or gentamicin).
4 Subsequent management. When the temperature, pulse and
other physical signs show that the inflammation is subsiding, oral fluids are reinstated
followed by regular diet. Ultrasonography is performed .
Cholecystectomy may be performed on the next available list.
Routine early operation operation is undertaken within 5–7 days of the onset of the attack,
the surgeon is experienced and excellent operating facilities. If an early operation is not
indicated, should wait 6 weeks for the inflammation to subside before proceeding to
operate.
EMPYEMA OF THE GALL BLADDER
The gall bladder appears to be filled with pus. It may be a sequel of acute cholecystitis or the
result of a mucocele becoming infected. The treatment is drainage and, later,
cholecystectomy.
Acalculous cholecystitis
Acute and chronic inflammation of the gall bladder can occur in the absence of stones and
give rise to a clinical picture similar to calculous cholecystitis.
Acute acalculous cholecystitis is seen particularly in patients recovering from major surgery
(e.g. coronary artery bypass), trauma and burns. In these patients, the diagnosis is often
missed, and the mortality rate is high
THE CHOLECYSTOSES (CHOLESTEROSIS, POLYPOSIS, ADENOMYOMATOSIS AND
CHOLECYSTITIS GLANDULARIS PROLIFERANS)
This is a not uncommon group of conditions affecting the gall bladder, in which there are
chronic inflammatory changes with hyperplasia of all tissue elements.
Cholesterosis (‘strawberry gall bladder’)
In the fresh state, the interior of the gall bladder looks something like a strawberry
Cholesterol polyposis of the gall bladder
Cholecystography shows negative shadows in a functioning gall bladder, or there is a well-
defined polyp present on ultrasound.
surgery is advised only if they change in size or are longer than 1 cm.
Cholecystitis glandularis proliferans (polyp, adenomyomatosis and intramural
diverticulosis)
A polyp of the mucous membrane is fleshy and granulomatous. All layers of the gall bladder
wall may be thickened, but sometimes an incomplete septum forms that separates the
hyperplastic from the normal. Intraparietal ‘mixed’ calculi may be present.
These can be complicated by an intramural, and later extramural, abscess. If symptomatic,
the patient is treated by cholecystectomy.
Diverticulosis of the gall bladder
Diverticulosis of the gall bladder is usually manifest as black pigment stones impacted in the
outpouchings in the wall of gall bladder . Diverticulosis of the gall bladder may be
demonstrated by cholecystography, especially when the gall bladder contracts after a fatty
meal. There are small dots of contrast medium just within and outside the gall bladder . The
treatment is cholecystectomy
CHOLECYSTECTOMY
Preparation for operation
An appropriate history is taken, and the patient’s fitness for the procedure is assessed. This
includes investigation of the cardiovascular and respiratory systems, and a full blood count
and biochemical are performed to exclude anaemia or abnormal liver function. Blood
coagulation is checked if there is a history of jaundice. The patient is given prophylactic
antibiotics either with pre-medication or at the time of anaesthetic induction. A second-
generation cephalosporin is appropriate. Subcutaneous heparin or anti-embolic stockings are
prescribed. Informed consent should be taken .

Laparoscopic cholecystectomy
The preparation and indications for cholecystectomy are the same whether it is performed
by laparoscopy or by open techniques.
Laparoscopic cholecystectomy is the procedure of choice for the majority of patients with
gall bladder disease .
Serious complications of laparoscopic cholecystectomy fall into two major areas: access
complications or bile duct injuries. In the main, access complications occur during the
insertion of the Verres needle to establish pneumoperitoneum or the insertion of trocars. If
insertion is performed blindly or is found to be difficult, visceral injury should be excluded. If
either a visceral or a bile duct injury is suspected, conversion to an open technique is
recommended by most surgeons.
Open cholecystectomy
For patients in whom a laparoscopic approach is not indicated or in whom conversion from a
laparoscopic approach is required, an open cholecystectomy is performed.
A cholecystostomy is rarely indicated but, if necessary, as many stones as possible should be
extracted, and a large Foley catheter (14F) placed in the fundus of the gall bladder with a
direct track externally.
Indications for choledochotomy
1-palpable stones in the common bile duct;
2- jaundice, a history of jaundice or cholangitis;
3- a dilated common bile duct;
4- abnormal liver function tests, in particular a raised alkaline phosphatase.

‘post-cholecystectomy’ syndrome
cholecystectomy fails to relieve the symptoms for which the operation was performed. Such
patients may be considered. However, such problems are usually related to the preoperative
symptoms and are merely a continuation of those symptoms. Full investigation should be
undertaken to confirm the diagnosis and exclude the presence of a stone in the common bile
duct, a stone in the cystic duct stump or operative damage to the biliary tree.
Management is best performed by MRCP or ERCP.
Management of bile duct obstruction following cholecystectomy
Incidence of bile duct injury is 0.05% Patients with symptoms developing either immediately
or delayed after a cholecystectomy, particularly if jaundice is present, need urgent
investigation. This is especially true if the jaundice is associated with infection, a condition
called cholangitis.
The first step in management is to do ultrasound scan. This will demonstrate whether there
is intra- or extrahepatic ductal dilatation. The anatomy needs to be defined by either an ERCP
or an MRCP. The latter investigation will also allow for therapeutic manoeuvres such as
removal of an obstructing stone or insertion of a stent across a biliary leak. If a fluid
collection is present in the subhepatic space, drainage catheters may be required.
the injury declares itself postoperatively by: (1) a profuse and persistent leakage of bile if
drainage has been provided, or bile peritonitis if such drainage has not been provided; and
(2) deepening obstructive jaundice.
Treatment
In the debilitated patient, temporary external biliary drainage may be achieved by passing a
catheter percutaneously into an intrahepatic duct. Also, stents may be passed through
strictures at the time of ERCP and left to drain into the duodenum.
When the general condition of the patient has improved, definitive surgery can be
undertaken, Roux-en-Y choledochojejunostomy by an experienced surgeon. For a stricture of
recent onset through which a guidewire can be passed, balloon dilatation with insertion of a
stent is an acceptable alternative.
Stones in the bile duct
Duct stones may occur many years after a cholecystectomy or be related
to the development of new pathology, such as infection of the biliary tree
or infestation by Ascaris lumbricoides or Clonorchis sinensis. Any
obstruction to the flow of bile can give rise to stasis with the formation of
stones within the duct. The consequence of duct stones is either
obstruction to bile flow or infection. Stones in the bile ducts are more
often associated with infected bile (80%)
Symptoms
The patient is often ill and feels unwell. The term ‘cholangitis’ is given to the triad of pain,
jaundice and fevers, sometimes known as ‘Charcot’s triad’.
Signs
Tenderness may be elicited in the epigastrium and the right hypochondrium. In the jaundiced
patient, it is useful to remember Courvoisier’s law – in obstruction of the common bile duct
due to a stone, distension of the gall bladder rarly occurs; In obstruction from other causes,
distension of the gall bladder is common .
Management
It is essential to determine whether the jaundice is due to liver disease, disease within the
duct, such as sclerosing cholangitis, or obstruction of the biliary tree. Ultrasound scanning,
liver function tests, liver biopsy and MRI or ERCP will delineate the nature of the obstruction.
The patient may be ill. Pus may be present within the biliary tree, and liver abscesses may
develop.
Full supportive measures are required with
1- rehydration,
2- correction of clotting abnormalities
3- treatment with appropriate broad-spectrum antibiotics.

Once the patient has been resuscitated, relief of the obstruction is essential. ERCP with a
sphincterotomy, removal of the stones using a Dormia basket or the placement of a stent if
stone removal is not possible.
If this technique fails, percutaneous transhepatic Cholangiography can be performed to
provide drainage and subsequent percutaneous choledochoscopy. Surgery, in the form of
choledochotomy, is now rarely used .
Choledochotomy
The aim of this surgery is to drain the common bile duct and remove the stones by a
longitudinal incision in the duct. When the duct clear of stones, a T-tube is inserted and the
duct closed ; the bile is allowed to drain externally. When the bile has become clear and the
patient has recovered, a cholangiogram is performed, usually 7–10 days following operation.
If residual stones are found, the T-tube is left in place for 6 weeks so that the track is
‘mature’.
Stricture of the bile duct
Causes of benign biliary stricture
Congenital
■ Biliary atresia
Bile duct injury at surgery
■ Cholecystectomy
■ Choledochotomy
■ Gastrectomy
■ Hepatic resection
■ Transplantation
Inflammatory
■ Stones
■ Cholangitis
■ Parasitic
■ Pancreatitis
■ Sclerosing cholangitis
■ Radiotherapy
Trauma
Idiopathic

Radiological investigation of biliary strictures
■ Ultrasonography
■ Cholangiography via T-tube, if present
■ ERCP
■ MRCP
■ PTC
■ CT
PRIMARY SCLEROSING CHOLANGITIS
Primary sclerosing cholangitis is an idiopathic fibrosing inflammatory condition of the biliary
tree that affects both intrahepatic and extrahepatic ducts. It is of unknown origin, but
association with elevated markers such as smooth muscle antibodies and anti-nuclear f actor
suggests an immunological cause. The majority of patients are 30 - 60 years of age.
Strongly association with inflammatory bowel disease, especially ulcerative colitis.
Common symptoms include right upper quadrant discomfort, jaundice, pruritus, fever,
fatigue and weight loss.
Investigation
reveals a cholestatic pattern in liver function tests with elevation of serum alkaline
phosphatase and gamma-glutamyl transferase.
Imaging studies
such as MRCP or ERCP may demonstrate stricturing and beading of the bile ducts
A liver biopsy is helpful in confirming the diagnosis
and may help to guide therapy by excluding cirrhosis.
The important differential diagnoses are secondary sclerosing cholangitis and
cholangiocarcinoma.
Management with antibiotics, vitamin K, cholestyramine, steroids and immunosuppressants
such as azathioprine is generally unsuccessful. Endoscopic stenting of dominant strictures in
extrahepatic disease, operative resection may be worthwhile. For patients with cirrhosis,
liver transplantation is the best option

PARASITIC INFESTATION OF THE BILIARY TRACT
Biliary ascariasis
The round worm, Ascaris lumbricoides, commonly infests the intestine of inhabitants of Asia,
Africa and Central America. It may enter the biliary tree through the ampulla of Vater and
cause biliary pain
Complications include strictures, suppurative cholangitis, liver abscesses and empyema of
the gall bladder. In the uncomplicated case, anti-spasmodics can be given to relax the
sphincter of Oddi, and the worm will return to the small intestine to be dealt with by
antihelminthic drugs. Operation may be necessary to remove the worm or deal with
complications.
Worms can be extracted via the ampulla of Vater by ERCP
Hydatid disease
A large hydatid cyst may obstruct the hepatic ducts. Sometimes,a cyst will rupture into the
biliary tree and its contents cause obstructive jaundice or cholangitis, requiring appropriate
surgery
TUMOURS OF THE BILE DUCT
Benign tumours of the bile duct
These are uncommon and need to be distinguished from other benign conditions such as
choledocholithiasis, sclerosing cholangitis,Caroli’s disease and choledochal cysts.
Benign neoplasms causing biliary obstruction may be classified as follows:
• papilloma and adenoma;
• multiple biliary papillomatosis;
• granular cell myoblastoma;
• neural tumours;
• leiomyoma;
• endocrine tumours.

Malignant tumours of the bile duct(cholangiocarcinoma)
Carcinoma may arise at any point in the biliary tree, from the common bile duct to the small
intrahepatic ducts .
Incidence
This is a rare malignancy accounting for 1–2% of new cancers .
with two-thirds of patients being older than 65 years.
Histologically, the tumour is usually an adenocarcinoma (cholangiocarcinoma).
Associations
Patients with a history of ulcerative colitis, hepatolithiasis, choledochal cyst or sclerosing
cholangitis . In addition liver fluke infestations in the Far East . Opisthorchis viverrini
infestation is important in Thailand and Malaysia. These parasites induce DNA changes and
mutations through production of carcinogens and free radicals, which stimulate cellular
proliferation in the intrahepatic bile ducts and lead to invasive cancer .
Clinical features
Biliary tract cancers tend to be slow-growing tumours that invade locally and metastasise to
local lymph nodes. Distant metastases to the peritoneal cavity, liver and lung do occur.
Jaundice is the most common presenting feature. Abdominal pain, early satiety and weight
loss are also commonly seen. On examination, jaundice is evident, cachexia and a palpable
gall bladder is present if the obstruction is in the distal common bile duct (Courvoisier’s sign).
Investigations
1-Biochemical investigations will confirm the presence of obstructive jaundice (elevated
bilirubin, alkaline phosphatase and gamma-glutamyl transferase).
2-The tumour marker CA19-9 may also be elevated.
3- Non-invasive studies such as ultrasound and CT
scanning define the level of biliary obstruction, the extent of disease and the presence of
metastases .

For proximal tumours, percutaneous transhepatic cholangiography is the most useful
modality, it allows percutaneous biliary drainage, and samples can be obtained for cytology
to confirm the diagnosis.
For distal tumours, an ERCP is preferred as an endobiliary stent can be placed across the
obstructing lesion.
Again, cytology or biopsies can be taken for diagnosis
Treatment
The treatment depends on the site and extent of disease. Most patients are inoperable,
surgical resection, , resection may involve partial hepatectomy and reconstruction of the
biliary tree. Distal common duct tumours may require a pancreaticoduodenectomy. with
20% of patients surviving 5 years post resection. Adjuvant chemotherapy or radiotherapy has
a limited role.
Carcinoma of the gall bladder
Incidence
This is a rare disease ,The highest incidence is in Chileans, American Indians and in parts of
northern India, In western practice,gall bladder cancer accounts for less than 1% of new
cancer diagnoses.The patients are usually older, in their sixties or seventies.
The aetiology is unclear, but there may be an association with -----1-preexisting gallstone
disease.
2- Calcification of the gall bladder is associated with cancer . 3-Infection may promote
the development of cancer as the risk of carcinoma in typhoid carriers is significantly
increased.
Pathology
The majority of cases are adenocarcinoma (90%). Grossly, carcinomas are difficult to
differentiate from chronic cholecystitis

Clinical features
Patients may be asymptomatic at the time of diagnosis. If symptoms are present, they are
usually indistinguishable from benign gall bladder disease such as biliary colic or cholecystitis,
Jaundice and anorexia are late features.
A palpable mass is a late sign.
Investigation
Laboratory findings may be consistent with biliary obstruction or non-specific findings such
as anaemia, leucocytosis, mild elevation in transaminases and increased erythrocyte
sedimentation rate (ESR) or C-reactive protein (CRP). The level of serum CA19-9 is elevated in
80% of patients. The diagnosis is made on ultrasonography and CT scan, with a percutaneous
biopsy confirming the histological diagnosis.
In selected patients, laparoscopy is useful in staging the disease, as it can detect peritoneal or
liver metastases .
Treatment and prognosis
Occasionally, the diagnosis is made by histological examination of a gall bladder removed for
‘benign’ gallstone disease. For earlystage disease confined to the mucosa or muscle of the
gall bladder, no further treatment is indicated. However, for transmural disease, a radical en
bloc resection of the gall bladder fossa and surrounding liver along with the regional lymph
nodes should be performed. a 5-year survival is 5%.
