Family & Community Medicine dept.
Control of Communicable diseases-Respiratory diseasesLecture-4-Fourth stage
December 23rd ,2020
Dr. Muslim N. Saeed
Mumps(Infectious parotitis)
What is mumps?It is a disease caused by the mumps virus.
Who gets mumps?
Past infection with mumps makes a person immune to mumps; most people born before 1957 most likely have already had mumps. In addition, people who receive two doses of the mumps vaccine are much less likely to be infected. The greatest risk of infection occurs among older children, adolescents, and adults.
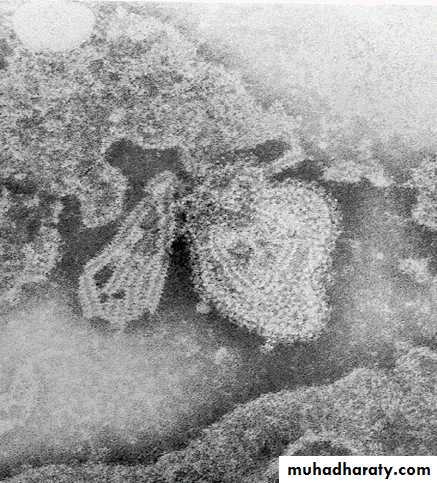
Mumps Virus
ParamyxovirusIt is a single-stranded RNA virus
One antigenic type
Rapidly inactivated by chemical agents (formalin, ether, chloroform), heat and ultraviolet light.
•
How is mumps spread?
Mumps is spread in droplets from the nose or throat of an infected person, usually when a person coughs or sneezes. Mumps can also spread by direct contact with saliva and discharges from the nose and throat of aninfected person.
Mumps Clinical Features
Incubation period 14 - 18 daysNonspecific prodrome of low-grade fever, headache, malaise, myalgias
Parotitis in 30% - 40%
Up to 20% of infections asymptomatic
May present as lower respiratory illness, particularly in preschool-aged children
The most common signs and symptoms of mumps include fever, headache, and swelling and tenderness of one or more salivary glands.
Swelling of the testicles occurs in 20-30% of infected males - this does not usually result in sterility.
Mumps can also cause CNS disorders such as encephalitis and meningitis.
Other complications include miscarriage, arthritis, pancreatic involvement, or deafness.How soon after infection do signs and symptoms occur?
Signs and symptoms of mumps usually appear within 18 days after exposure, but may appear any time within 12 to 25 days after exposure.
When and for how long is a person able to spread mumps?
Mumps is contagious from three days before until five days after the onset of swelling.What is the treatment for mumps?
Supportive care to relieve symptoms may include applying intermittent ice or heat to the affected neck area, and pain relievers. Warm salt water gargles, soft foods, and extra fluids may also help. Avoid fruit juice or acidic foods, since these stimulate the salivary glands, which can be painful.
CNS involvement
Orchitis
Pancreatitis
DeafnessDeath
15% of clinical cases
20% - 50% in post- pubertal males
2% - 5%1 / 20,000
1 - 3 / 10,000Mumps Complications
Mumps Epidemiology
Reservoir HumanTransmission Respiratory drop nuclei
Subclinical infections may transmit
Temporal pattern Peak in late winter and spring
Communicability Three days before to five
days after onset of activedisease
During adulthood, infection is likely to produce more sever disease including orchitis.
Death attributable to mumps is rare, the estimated case fatality rate is 3.8 per 10000. more than fatalities occur in people older than 19 years of age.Mumps infection during the first trimester of pregnancy is associated with an increased risk of spontaneous abortion.
There is no evidence exists that mumps infection during pregnancy causes congenital malformations.
Peak incidence was between January and May
Treatment: Supportive
Isolation of the hospitalized patient: in addition to standard precautions, droplet precautions are recommended until 9 days after onset of parotid swelling.
Control Measures:
1- School and child care : children should be excluded for 9 days from the onset of parotid swelling
2- Care of exposed people: vaccine not effective in preventing infection after exposure. However mumps vaccine can be given after exposure, because Immunization will provide protection against subsequent exposure. .Immunization during the incubation period has no increased risk. Mumps Ig is of no value
Mumps Vaccine
Composition Live virus
Efficacy 95% (Range, 90% - 97%)
Duration ofImmunity Lifelong
Schedule 2 Doses (as MMR)
Should be administered with measles and rubella (MMR)
Mumps Vaccine (MMR) IndicationsAll infants >12 months of age
Susceptible adolescents and adults without documented evidence of immunity
Second Dose Recommendations
First dose of MMR at 12-15 monthsSecond dose of MMR at 4-6 years
Second dose may be given any time >4 weeks after the first dose
What can be done to prevent the spread of mumps?
The single most effective control measure is maintaining the highest possible level of immunization in the community.Children with mumps should not attend school, and adults should not work, until five days after swelling began or until they are well, whichever is longer.
Adverse Reactions:
febrile seizures, nerve defness,meningitis, encephalitis, rash ,pruritis .orchitis and parotitis have been reported rarely.
PertussisWhooping Cough
Epidemiology• Is an acute, communicable infection of the respiratory tract caused by the gram-negative bacterium, Bordetella pertussis.
• Whooping cough is a disease of infants and pre-school children.
• The highest incidence found before the age of 5 years.
• Outbreaks occur periodically every 3-4 years.
• Marked decline has occurred in incidence & mortality rates during the last four decades in communities with active immunization program, good nutrition and good medical care
Susceptibility & resistance
In non immunized susceptibility is universal.Highest incidence is in infants.
School children are often act as a source of infection for younger siblings at home
Incidence, mortality and morbidity are higher in females than males.
There is no maternal immunity.
One attack confers long immunity although second attacks can occasionally occur.
Susceptibility & resistance
Cases in previously immunized adolescents and adults occur because of waning immunity.Protection produced by the vaccine is greater against severe disease & begins to wane after about 3 years
Active immunization after exposure is not protective but it is not contraindicated
• Reservoir Human
• Mode of transmission
• Direct contact with respiratory discharge of infected person.
• Airborne
• Droplet
Incubation period 6-20 days
Period of communicabilityPatient not treated with proper antibiotic
onset of typical paroxysmEither early in the or 3weeks after
Catarrhal stage
In treated patient with erythromycin
5 days after the onset of therapy.(Pt is non-infectious).Clinical features
• Catarrhal phase:• is characterized by rhinorrhea, lacrimation, malaise, and cough that is mild and nonproductive. low-grade fever may also be present. This phase lasts between a few days and 1 week
• Paroxysmal phase :
• cough becomes more severe and frequent and eventually paroxysmal where five or more forceful coughs occur in a single episode; this phase usually lasts for 1-2 months or longer.
• Young infants, partially vaccinated children, adolescents and adults often do not exhibit the whoop or cough paroxysm.
Clinical features
• Convalescent phase:• The cough becomes less frequent and milder. This phase may last another 1-2 weeks or longer
• Complications
• Respiratory (bronchitis, otitis media ,bronchopneumonia,pneumothorax)
• Subcojuctival hemorrhage
• epistaxis
• CNS (convulsion, encephalitis)
Diagnosis
Laboratory methods currently available for the identification of B. pertussis include,Culture
polymerase chain reaction (PCR),
direct fluorescent antibody testing, and
serologic antibody testing.
Prevention and control
• 1.Public education• Danger of the disease.
• Importance of immunization.
• Adherence to the immunization schedule
• 2.Immunization
• is recommended with 3 doses of vaccine consisting of a suspension of killed bacteria with diphtheria & tetanus.
Prevention
• DPT whole cell vaccine
• DTaP a cellular preparation
• Iraq DPT
• 2 months
• 4 months
• 6 months
• 18 months first booster
• school entry second booster
Prevention cont.
3. Protection of health workers who have been exposed to pertussis cases by using a 14 days course of erythromycin, azithromycin, clarithromycin.Control
• Reporting is obligatory• Isolation
• Respiratory isolation for known cases
• Suspected cases should be removed from the presence of infants (especially unimmunized infants)& young children until:
• Patient have received at least 5 days of antibiotics.
• Those who do not receive antibiotics should be isolated for 3 weeks.
Control cont.
• Contacts
• Inadequately immunized household contacts <7 years should be excluded from Schools for 21 days after exposure or until the case and contacts have received 5 days course of antibiotics.
• Verification of immunization status up to date.
• Passive immunization is not effective.
• Initiation of active immunization following recent exposure is not effective.
• Close contacts <7 years who have not receive 4 DTP doses; or have not received a DTP dose within 3 years should be given a booster dose as soon as possible after exposure.
Control cont.
• Antibiotic prophylaxis• Initiation of postexposure prophylaxis in asymptomatic contacts within 21 days of the onset of cough in the index case can prevent the development of symptoms.
• Indications
• Close contacts.
• Individuals at high risk for severe or complicated pertussis.
• Regimins (Erythromycin for 14 days,Clarithromycin for 7 days,Azithromycin for 5 days)
Persons at high risk for severe or complicated pertussis include
• Infants particularly those younger than four months• Persons with immunodeficiency
• Persons with underlying medical conditions (chronic lung disease, respiratory insufficiency, cystic fibrosis)
Control cont.
• Specific treatment
• Treatment should be initiated within 21 days of start of symptoms
• The regimen for antimicrobial treatment is the same as that for prophylaxis
• Treatment shortens the period of communicability but does not affect symptomatology.
Diphtheria
EpidemiologyDiphtheria is an acute, communicable disease caused by the gram-positive bacillus Corynebacterium diphtheriae.
Among non immunized populations, diphtheria most often occurs during fall and winter, although summer outbreaks have occurred.
In tropical areas seasonality is less distinct.
Disease spreads more quickly and is more prevalent in poor socioeconomic conditions, where crowding occurs and immunization rates are low.
Epidemiology
Race No racial differences observedGender
No difference has been described for acute infections.
Age
Diphtheria affect children 1-5 years. In countries where wide spread immunization is practiced ,a shift in age incidence has been observed from preschool to school age.
Reservoir is Human
Mode of transmission
Direct contact with patients or carriersIndirect
Articles
Raw milk
Incubation period 2-5 days
• Period of communicability• Unless treated, the period of communicability varies from 14-28 days from the onset of disease.
• Carriers may remain infective for longer periods.
• A case or carrier may be considered non-communicable when 2 cultures from the nose and throat ,24 hr apart, negative for diphtheria bacilli.
Susceptibility & resistance
There is maternal immunity which usually lost by age of 6 months.(for infants of immune mothers).Disease or inapparent infection usually,but not always lead to life long immunity
Toxoid gives prolonged but not life long immunity which wanes with age.
Clinical features
Respiratory tract form of diphtheria consist of pharyngo-tonsillar ,laryngo-tracheal ,nasal and combination of these forms.
Pharyngo-tonsillar : sore throat, low grad fever,
O/E mild pharyngeal erythema and localized exudate or grey-black adherent membrane
Attempt to remove the membrane result in bleeding
Laryngo-tracheal disease most often proceeded by pharyngotonsillar diphtheria, patient presented with hoarseness of voice and croupy cough.
Diagnosis
• Clinical findings• Bacteriological examination
• Isolation of CoryneBacterium diphtheriae on cultures confirm the diagnosis.
• In all patients in whom diphtheria is suspected, obtain specimens from the nose and throat (i.e., nasopharyngeal and pharyngeal swab) for culture.
• Isolation of C .diphtheriae from close contacts may confirm the diagnosis, even if results of cultures on specimens taken from the patient are negative.
• Prevention
• Educational measures about the hazards of the disease and Importance of immunization• Active immunization should be initiated in infancy (DTaP, DTP)
• Children <7 years of age (in Iraq)
• 2 months 1st dose
• 4 months 2nd dose
• 6 months 3rd dose
• 18 moths 1st booster dose
• 4-6 years 2nd booster dose
• This schedule does not need to be restarted because of delay in administering the scheduled dose .
• If pertusis component of DTP is contra-indicated; use DT form.
Prevention cont.
Person age 7 years &older
Adult (Td) is usually used (highly purified) for previously unimmunized.
3doses of Td is given,
1st,2nd doses at 4-8 weeks intervals.3rd dose after 6 months - 1 years after the 2nd dose.
Active protection is maintained by giving a dose of Td every 10 years.
Prevention cont.
• Protection of highly risk group;• They should be fully immunized and receive a booster dose every 10 years.
• HIV & immunocompromised children should be vaccinated. Use the same schedule
Control
• Reporting obligatory• Isolation:
• Strict isolation for pharyngeal type.
• Until 2cultures both from nose &throat
• taken( not less than 24 hours apart after cessation of antibiotic therapy) fail to show the microorganism.
• If there is no facility; isolation may end after 14 days course of appropriate antibiotic therapy.
• Disinfection
Control cont.
4-Contacts
7 days surveillance
Cultures from nose &throat
Single dose of benzathin penicillin IM
(600,000units for younger persons < 6years &
(1.200.000units for older persons) or
7-10 days course of erythromycin is recommended for all persons with household exposure, regardless of their immunization status
5- specifice treatment (antitoxine and antibiotics)
Control cont.
AntitoxinSensitivity testing
Single daily dose 20000 units for anterior nasal diphtheria to100000 units for extensive disease by IM route for 14 days.
Antibiotics
Procaine penicillin G (IM) 600000 U for children and 1.2 million U for adults in 2 divided doses)
Recommended duration is 14 days
Epidemics measures
• Immunize all <5 & highly risk groups . Repeat immunization one month later to provide at least 2 doses to the recipient.• Identify contacts, population at risk.
• Carry out special investigation of reported cases to verity diagnosis &to determine biotype & toxigenicity of the organism.
Thanks