Pelvic organ prolapse
Dr. Ezdehar Nassif AliPelvic organ prolapse (POP)
A prolapse is a protrusion of an organ or structure beyond its normalconfines .
• The herniation of the pelvic organs to or beyond the vaginal walls is a common condition. A prevalence of 41-50% of women over the age of 40 years.
Many women with prolapse experience symptoms that impact daily activities, sexual function, and exercise.
Its caused by injury to the muscles or tissues that support the pelvic organs.
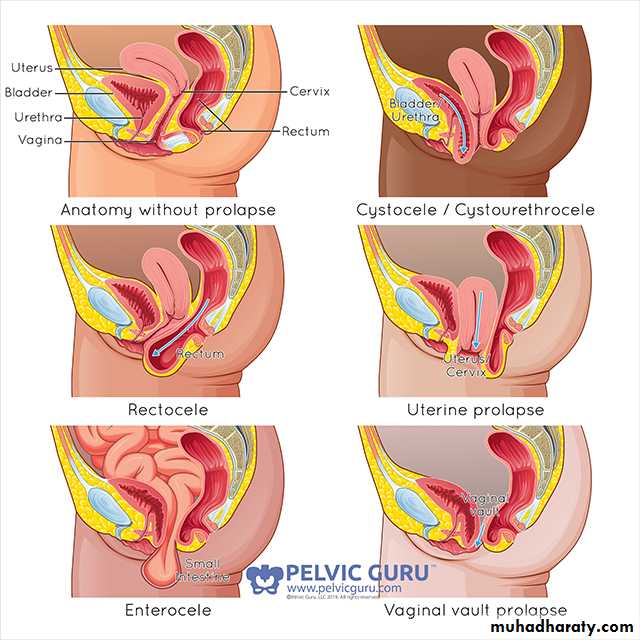
Classification:
Prolapses are classified according to their location and the organs contained within them.Anterior vaginal wall prolapse
• Urethrocele: Prolapse of the urethra through the vagina
• Cystocele: Prolapse of the bladder through the vagina
• Cystourethrocele: descent of bladder and urethra
Posterior vaginal wall prolapse
• Rectocele: Prolapse of the rectum through the vagina
• Enterocele : Prolapse of the small bowel through the vagina
Apical vaginal prolapse
• Uterovaginal : uterine descent with inversion of vaginal apex
• Vault: post-hysterectomy inversion of vaginal apex
Grading:
Three degrees of prolapse are described and the lowest or most dependent portion of the prolapse is assessed while the patient is straining:1st: descent within the vagina
2nd: descent to the introitus
3rd: descent outside the introitus.
In the case of uterovaginal prolapse, the most dependent portion of the prolapse is the cervix, and carful examination can differentiate utero vaginal descent from a long cervix.
Third-degree uterine prolapse is termed ‘procidentia’ and is usually accompanied by cystourethrocele and rectocele.
Structure and function of the pelvic floor
• The pelvic floor functions to support the pelvic and abdominal viscera and help maintain control of their contents. It has two major components, which are interdependent: the muscle and fascia.Muscle:
Levator ani muscles consist of pubococcygeus, coccygeus and ileococcygeus muscles on each side ,which together form a muscular floor to the pelvis.
Fascia:
Fascia envelopes levator ani, attaches it to bone at its origin and holds the two muscles together in the midline. The urethra, vagina and rectum perforate this midline fascia.
Thus ,the pelvic viscera are supported by both the levator ani muscle and the fascial attachments that are condensed in some areas and are often referred to as ligaments—the uterosacral, cardinal and round ligaments being examples.
Aetiology
The connective tissue, levator ani and intact nerve supply are vital for the maintenance of position of the pelvic structures, and are influenced by pregnancy , childbirth and ageing. Whether congenital or acquired, connective tissue defects appear to be important in the aetiology of prolapse and urinary
stress incontinence.
Two per cent of symptomatic prolapse occurs in nulliparous women , implying that there may be a congenital weakness of connective tissue.
Risk factors:
• Parity — The risk of POP increases with increasing parity• Obstetric factors _POP can develop during pregnancy prior to delivery. Vaginal delivery is associated with a higher incidence of POP than cesarean.
Advancing age — Older women are at an increased risk for POP
• Obesity — Overweight and obese women (body mass index >25) have a two-fold higher risk of having prolapse than other women. While weight gain is a risk factor for developing prolapse, it is controversial whether weight loss results in prolapse regression. However, there are reports of POP regression in women after bariatric surgery.
• Hysterectomy —It is associated with an increased risk of apical prolapse.
Race and ethnicity — Data suggest that African-American women have a lower prevalence of symptomatic POP than other racial or ethnic groups in the US.• Other risk factor — chronic constipation is a risk factor for POP, likely due to repetitive increases in intra-abdominal pressure, the risk of prolapse is increased in women with occupations that involve heavy lifting.
•Some connective tissue disorders (e.g, Ehlers- Danlos syndrome) or congenital abnormalities (e.g, bladder exstrophy)
• Endocrine (menstrual cycle, pregnancy and menopause) are the most significant endocrine event effect pelvic floor fascia, (effect of progesterone)
Prevention:
Prolapse prevention strategies have not been extensively studied. Although vaginal childbirth is associated with an increased risk of prolapse, it is unclear that cesarean delivery will prevent the occurrence of prolapse.• Some data suggest that women with prolapse who use a vaginal pessary have a lower stage of prolapse on subsequent exams. Interventions such as weight loss, treatment of chronic constipation, and avoidance of jobs that require heavy lifting are potential interventions to avoid the development or progression of POP and deserve further investigation.
Clinical manifestations
Patients with POP may present with symptoms related specifically to the prolapsed structures, such as a bulge or vaginal pressure or with associated symptoms including urinary, defecatory or sexual dysfunction. Symptoms such as low back or pelvic pain have often been attributed to POP.
Severity of symptoms does not correlate well with the stage of prolapse. Symptoms are often related to position; they are often less noticeable in the morning or while supine and worsen as the day progresses.
Many women with prolapse are asymptomatic; treatment is generally not indicated in these women.
Bulge or pressure symptoms — Women with POP often present with the complaint of vaginal or pelvic pressure and/or the sensation of a vaginal bulge or something falling out of the vagina.
Some women are able to see a protrusion of the prolapse beyond the introit us (precidential).
Protrusion of the vagina may result in chronic discharge and/or bleeding from ulceration.
Urinary symptoms — Loss of support of the anterior vaginal wall or vaginal apex may affect bladder and/or urethral function. Symptoms of stress urinary incontinence often coexist with stage I or II prolapse, obstructive symptoms, incomplete bladder emptying , urinary retention.
Women with POP have a two- to five-fold risk of overactive bladder symptoms (urgency, urge urinary incontinence, frequency) compared with the general population.
In addition, some women with POP experience enuresis or incontinence with sexual intercourse.
Defecatory symptoms — the most common bowel symptom associated with prolapse is constipation. Other defecatory symptoms include fecal urgency and fecal incontinence and obstructive symptoms, e.g. incomplete emptying, straining, or the need to apply digital pressure to the vagina or perineum (splint) to completely evacuate; some women report fecal incontinence during sexual intercourse.
Effects on sexual function — Prolapse does not appear to be associated with decreased sexual desire or with dyspareunia.
Diagnosis :
Women usually present with non-specific symptoms . Specific symptoms may help to determine the type of prolapse.• A medical history is also important to elicit prolapse-associated symptoms, since treatment is generally indicated only for symptomatic prolapse, the Pelvic Organ Prolapse Quantitation (POPQ) system has become the most commonly used prolapse staging system.
Prolapse has traditionally been regarded as a progressive disease, with mild prolapse leading to more advanced disease. However, data suggest that the course is progressive until menopause, after which the degree of prolapse may follow a course of alternating progression and regression.
• Abdominal examination should be performed to exclude organomegaly or
• abdominopelvic mass.
Vaginal examination.
Prolapse may be obvious when examining the patient in the dorsal position if it
protrudes beyond the introitus; ulceration and / or atrophy may be apparent, and should be pelvic mass excluded.
The anterior and posterior vaginal walls and cervical descent should be assessed with the patient straining in the left lateral position, using a Sims
speculum .
Combined rectal and vaginal digital examination can be an aid to differentiate
rectocele from enterocele.
Differential diagnosis:
Anterior wall prolapse : congenital or inclusion dermoid vaginal cyst , urethral diverticulum.
Utero vaginal prolapse : large uterine polyp.
Treatment:
The choice of treatment depends on the patient’s wishes , level of fitness and desire to preserve coital function.Prior to specific treatment, attempts should be made to correct obesity ,chronic cough or constipation . If the prolapse is ulcerated ,a 7- day course of topical oastrogen should be administered.
If a woman is found to have uterovaginal prolapse on examination but has no symptoms, then it would be inappropriate to offer any surgical treatment and either observation or conservative therapy would be best.
• If symptoms are mild, then pelvic floor physiotherapy is offered but there are no randomized controlled trials examining the effectiveness of physiotherapy on prolapse.
• Vaginal pessary — the mainstay of non-surgical treatment for POP is the vaginal pessary.
• Pessaries are silicone-rubber-based-ring devices are the most popular form of conservative therapy, a variety of shapes and sizes, which support the pelvic organs. Approximately half of the women who use a pessary continue to do so in the intermediate term of one to two years. Pessaries must be removed and cleaned on a regular basis and need replacement at annual intervals.
Shelf pessary used in hysterectomies patient, patient do not desired sexual function and incase of vaginal ulceration and infection.
• The use of pessaries can be complicated by vaginal ulceration and infection. The vagina should therefore be carefully inspected at the time of replacement.
Indications for pessary treatment are:
• patient’s wish;
• as a therapeutic test;
• childbearing not complete;
• medically unfit;
• during and after pregnancy
• while awaiting surgery.
Ring pessary Shelf pessary
Surgery:The aim of surgical repair is to restore anatomy and function.
• There are vaginal and abdominal operations designed to correct prolapse , and choice often depends on a woman’s desire to preserve coital function.
Surgical treatment — Surgical candidates include women with symptomatic prolapse who have failed or declined conservative management of their prolapse.
Surgical prognosis depends upon the severity of symptoms, extent of the prolapse, physician experience, and patient expectations. Surgery has traditionally been associated with a recurrence/reoperation rate of up to 30%.
Cystourethrocele
Anterior repair (colporrhaphy) is the most commonly performed surgical procedure but should be avoided if there is concurrent stress incontinence.Rectocele
Posterior repair (colporrhaphy) is the most commonly performed procedure.
Enterocele
The surgical principles are similar to those of anterior and posterior repair , but the
peritoneal sac containing the small bowel should be excised.
In addition, the Pouch of Douglas is closed by approximating the peritoneum and /or the uterosacral ligaments.
Vault prolapse
Sacrocolpopexy, sacrospinous ligament fixation
Utero vaginal prolapse
If the woman dose not wish to conserve her uterus:
Vaginal hysterectomy with adequate support of the vault to the uterosacral ligament is sufficient.
Total abdominal hysterectomy and sacrocolpopexy.
Subtotal abdominal hysterectomy and sacrocervicopexy.
If uterine conservation is required; and then may choose this option:
Hysterosacropexy.Manchester operation.
Le Fort colpocleisis.