Dentoalveolar injuries are an important and common component of craniomaxillofacial trauma. The dentition serves as a vertical buttress of the face and fractures to this area may result in malalignment of facial subunits. Furthermore, the dentition is succedaneous with 3 phases—primary dentition, mixed dentition, and permanent dentition— mandating different treatment protocols.
DENTOALVEOLAR INJURIES
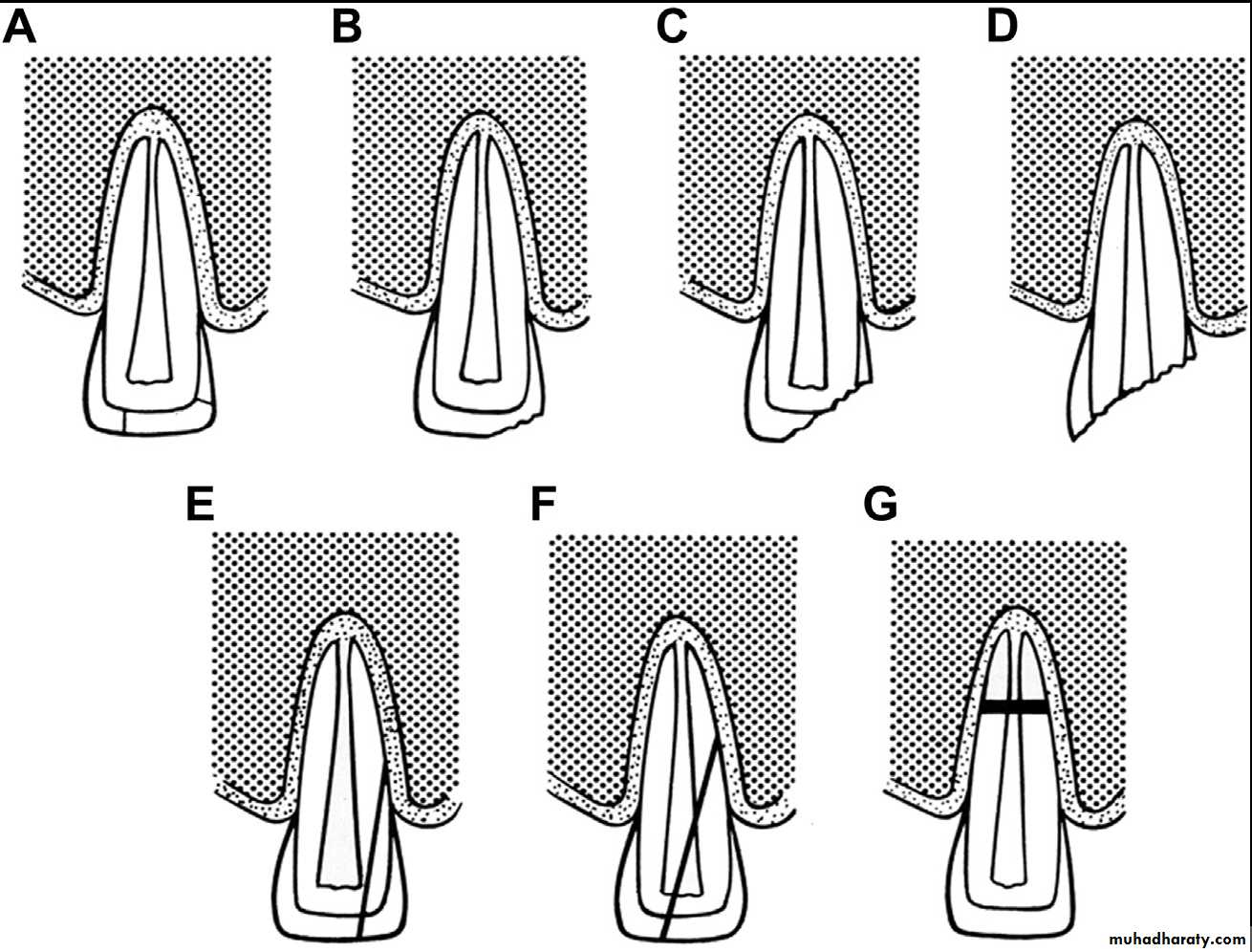
Infraction (A), uncomplicated enamel limited fracture (B), uncomplicated crown fracture (C), complicated crown fracture (D), uncomplicated crown-root fracture (E), complicated crown-root fracture (F), and root fracture (G).
CLASSIFICATION
Dental hard tissue- Infraction
Craze/crack in enamel only
Crown of tooth intact and normal
Percussion test nontender, normal radiograph
- Uncomplicated enamel limited fracture
A fracture or chip of enamel onlyNontender to palpation, nonmobile, enamel loss visible on radiograph
- Uncomplicated crown fracture
Crown fracture with missing tooth structure, including enamel and dentin but no pulpal or root exposure
- Complicated crown fracture
Crown fracture through enamel and dentin with exposure of pulp tissues- Uncomplicated crown-root fracture
Fracture through enamel, dentin, and cementum without exposure of pulp tissues- Complicated crown-root tracture
Fracture through enamel, dentin, and cementum and with pulp tissue exposure- Root fracture
Dentin and cementum fractured and pulp tissue exposed to PDL or oral cavity with no fracture of enamel; classified based on coronal third, middle third, or apical third of tooth involvedA coronal fracture that involved enamel and dentin.
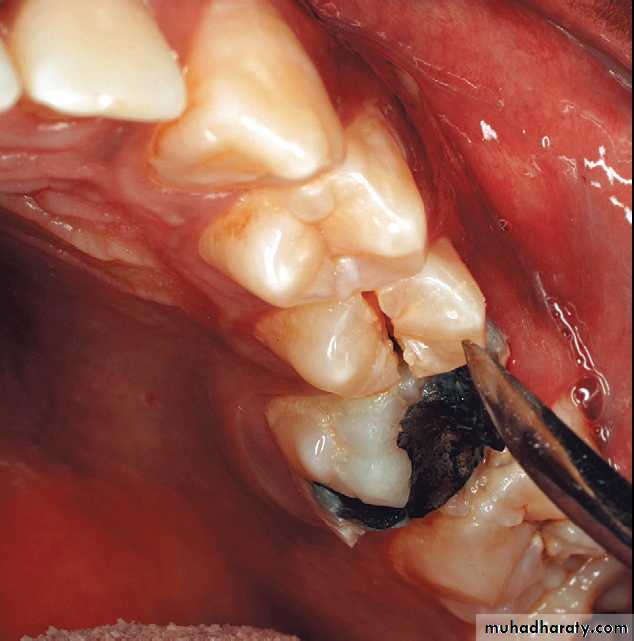
Crown-root fracture
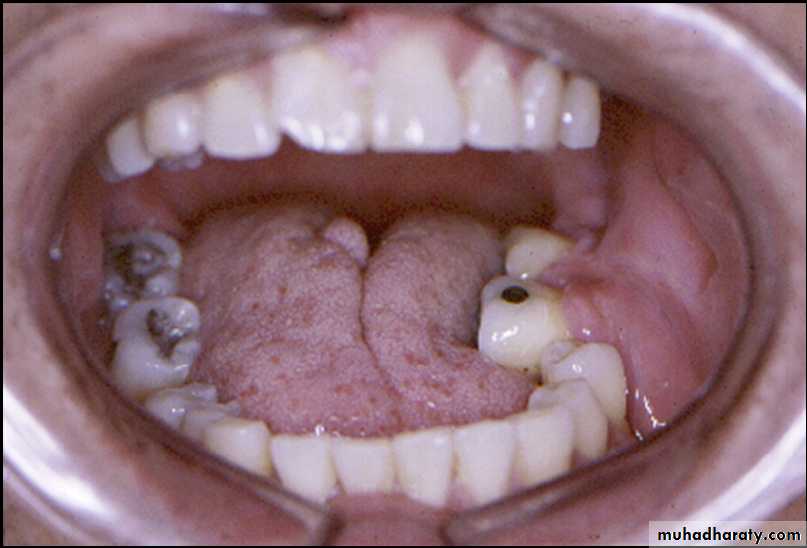
Incisors with crown-root fractures
Injuries to supporting bone- Comminution of both alveolar cortices
Often with intrusive or lateral luxation- Fracture of a single cortex
Buccal or lingual cortex fracture
- Fracture of alveolar process en bloc
Fracture may or may not propagate through socket, may contain 1 or multiple teeth but underlying maxilla or mandible grossly stable
- Mandible or maxillary fracture
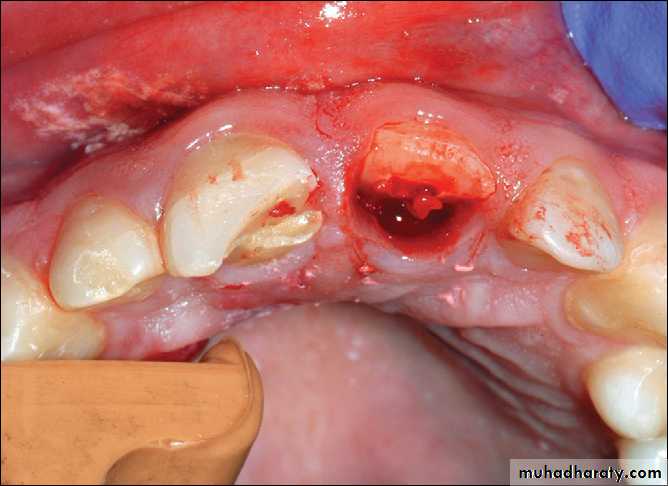
Nonreduced dentoalveolar fracture of the left posterior mandible interfering with occlusion.
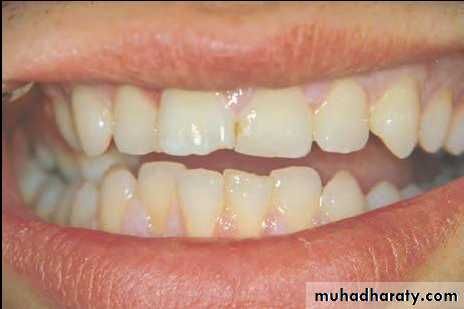
Primary contact in premolar region indicating an alveolar process fracture in the maxilla.
Injuries to PDL/dental supporting structures- Concussion
Injury to PDL producing sensitivity to percussion with no loosening or displacement of the tooth- Subluxation
Tooth loosened in socket but not displaced, sensitive to percussion
- Extrusion
Tooth loosened and partially displaced out of socket axially
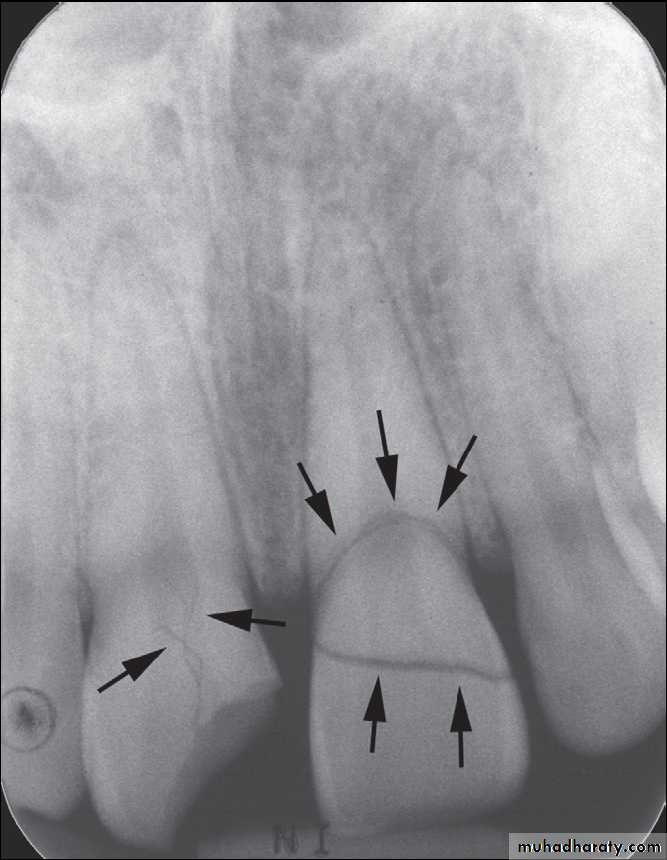
Radiographically widened PDL space at apex of tooth
PDL separated from alveolar bone
- Lateral luxation
Displacement of tooth other than axially (ie, medially, laterally, anteriorly, or posteriorly)
Radiographically, PDL space widened on side of tooth that was displaced away from
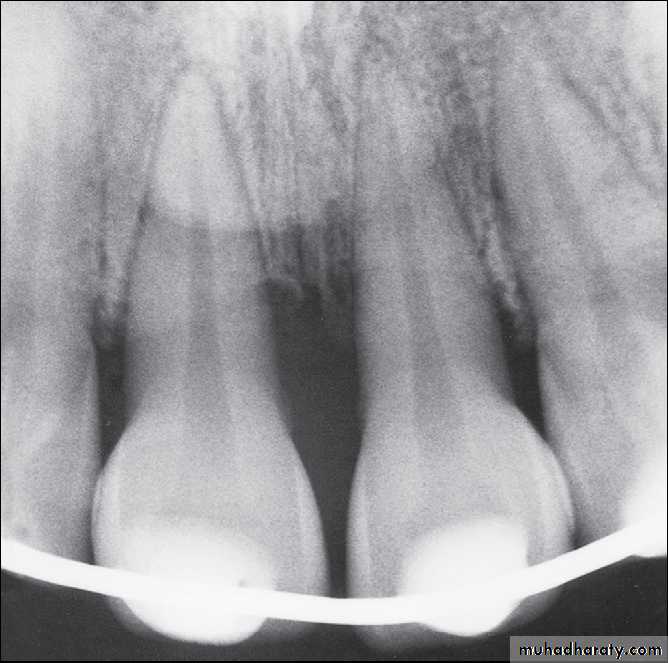
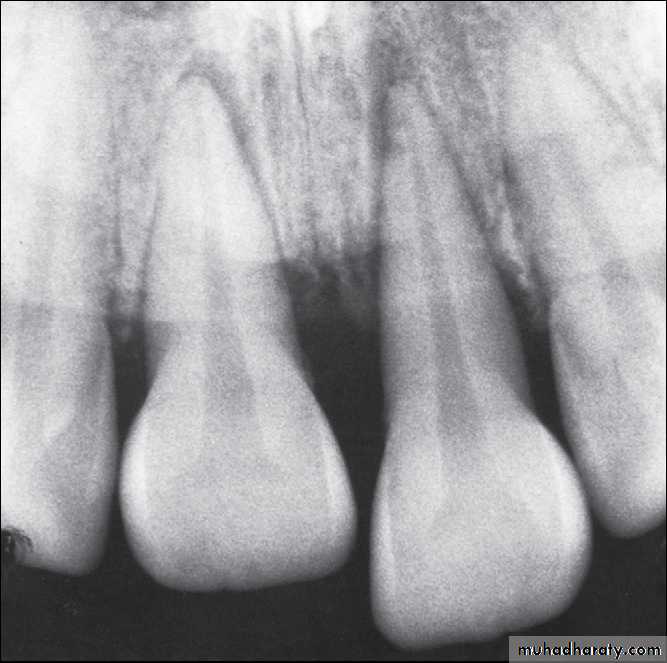
Radiographs of extruded tooth before and after repositioning and stabilization with acid-etch composite technique.
Platally displaced central and lateral incisors in apically mature tooth.
Position of teeth after digital reduction and stabilization with bonded arch wire.- Intrusion
Axial displacement of tooth deeper into the alveolusNo PDL space evident radiographically
Tooth may appear shorter clinically
Percussion yields a high-pitched “ting” metallic sound or sound more solid relative to other teeth
Can be problematic with primary dentition
- Avulsion
Complete disarticulation of tooth from socket
CLINICAL PRESENTATION
- Extraoral findings, including other facial trauma
- Intraoral findings
* Best accomplished with good lighting and suction, examining all soft tissues for ecchymosis, hematomas, and lacerations
* Care must be taken to identify debris in the oral cavity and account for lost dentition, appliances, or other hardware that evidence seems to indicate might have possibly been dislodged and is not accounted for in its entirety
* Chest and abdominal imaging should be ordered as indicated
Tooth Vitality Testing…
Tooth Mobility….Percussion…
Imaging
As far as radiographs are concerned, periapical and occlusal radiographs are best, with panoramic imaging slightly less favorable, especially with the anterior dentition.
Treatment
- Concussion* No need for treatment, observation only
* Soft food for 1 week, good oral hygiene
* Follow-up
- Subluxation
* May be no need for treatment
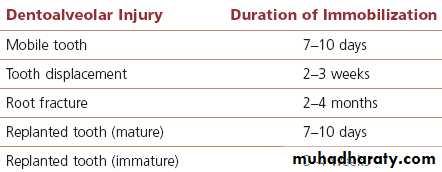
* Apply flexible composite splint for 2 weeks
* Soft food for 1 week, good oral hygiene, follow-up
- Extrusion and lateral luxation
* Cleanse area and carefully reposition tooth with axial pressure
* Apply flexible splint for 2 weeks
* Soft food for 1 week, good oral hygiene, Follow-up
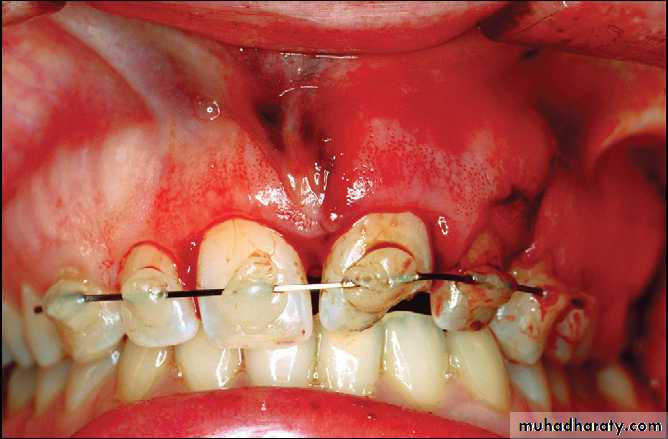
Fixation by wiring
Composite and orthodontic wire splint
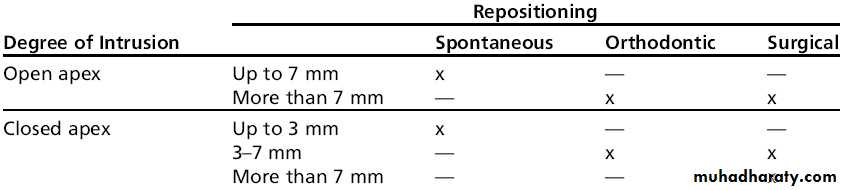
- IntrusionAssociated with a high incidence of tooth loss and tooth resorption
Dependent on extent of tooth root formation and amount of impaction
Early endodontic consultation recommended
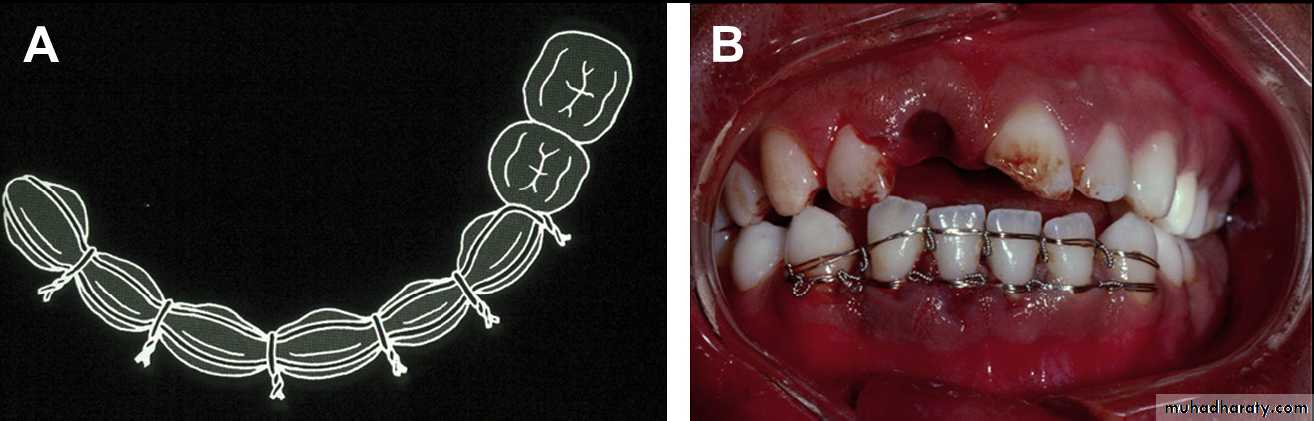
Intruded left central incisor treated by orthodontic repositioning.
Avulsion
Closed root apex, extraoral dry time or storage in physiologic media for less than 60 minutes:* Clean root surface and irrigate socket with saline
* Reimplant tooth with gentle digital pressure and verify position
* Apply flexible splint for 2 weeks
* Antibiotic coverage for 7 days; ensure tetanus coverage
* Early endodontic consultation recommended
* Soft food for 1 to 2 weeks, good oral hygiene, follow up
TREATMENT OF INJURIES TO THE SUPPORTING DENTOALVEOLAR BONE
Isolated alveolar bone injury often presents as a segment of teeth (usually 2–3) that has been displaced as a unit in one direction, with the involved teeth not independently mobile.- Fracture of both alveolar cortices
* Generally poorest prognosis of alveolar fractures but most common due to high incidence of combined dentoalveolar injuries. Often involves comminution of at least one cortex.
* Avoid performing full-thickness mucoperiosteal flaps that may devitalize bone fragments.
* Apply rigid splinting for 4 to 6 weeks with Erich arch bars, or acrylic splints that are wired in place. The stabilized segment should extend at least to 2 solid teeth on either side of the mobile teeth.
* Soft diet, good oral hygiene, follow up
- Fracture of a single cortex
Same as for comminution of both cortices but generally with better prognosis
Patient requires rigid fixation for 4–6 weeks
Follow-up the general/pediatric dentist in 1 week
Soft diet, good oral hygiene
- Mandible or maxillary fracture
Patient with mandibular body fracture and luxated incisors. The mandibular fracture has been fixated by plate and a separate fiberglass splint has been applied to the luxated and repositioned teeth.
SOFT TISSUE INJURIES
AbrasionA wound caused by friction between an object and the surface of the soft tissue.
The abraded areas should be thoroughly cleansed to remove foreign material. A topical application of an antibiotic ointment is adequate treatment. A loose bandage can be applied if the abrasion is deep but is unnecessary in superficial abrasions.
Contusion
A contusion is more commonly called a bruise and indicates that some amount of tissue disruption has occurred within the tissues, which resulted in subcutaneous or submucosal hemorrhage without a break in the soft tissue surface.If a contusion is seen early, application of ice or pressure dressings may help constrict blood vessels and thereby decrease the amount of hematoma that forms. If a contusion does not stop expanding, a hemorrhaging artery within the wound is likely. The hematoma may require surgical exploration and ligation of the vessel.
Laceration
A laceration is a tear in the epithelial and subepithelial tissues. A laceration is perhaps the most frequent type of soft tissue injury and is caused most commonly by a sharp object such as a knife or a piece of glass.Treatment
Wound cleansingDebridement
Hemostasis
And Closure by layered suturing.
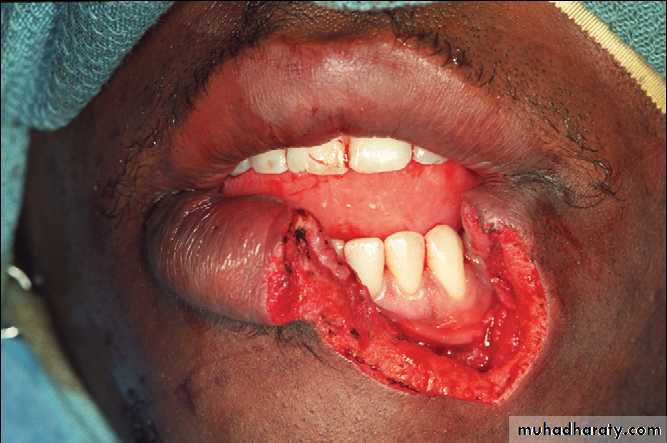
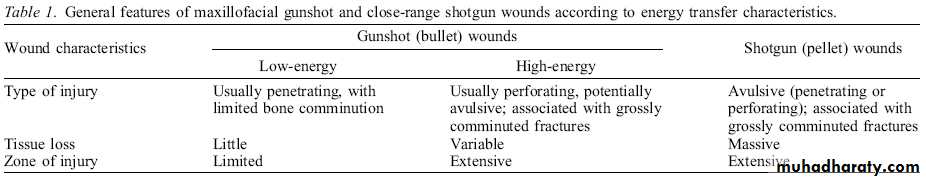
MAXILLOFACIAL GUNSHOT INJURIES
General features of maxillofacial ballistic injuries
Maxillofacial firearm-related injuries are customarily classified as either penetrating or perforating; each of these categories is determined by the terminal location of the projectile and its wounding effects.• Penetrating wounds are caused by missiles of low impact velocity, such as handgun bullets, with a small point of entry leading to the missile embedded in tissue.
• Perforating wounds are typically produced by higher velocity bullets, which create an exit wound that is often larger than the entrance.
• A third category is the avulsive or ablative injuries, characterized by significant bone and soft tissue loss. These are caused either by close-range shotgun blasts, with avulsion created by multiple pellets close to each other, or by high-velocity rifle bullets which may produce massive exit wounds as a result of bullet tumbling, bone fragmentation, or both.
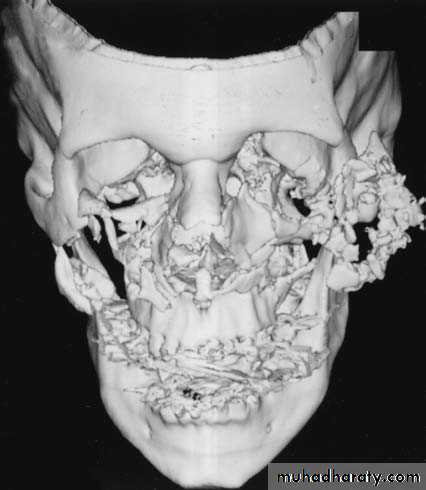
Differences between gunshot and civilian injuries:
• The fractures are usually extensively comminuted.• Always compound and contaminated.
• The viability of bone fragments and the extent of dental injuries cannot be accurately evaluated preoperatively.
• Fracture treatment is complicated by soft tissue injury or loss.
High-velocity entrance wound of the right cheek and exit wound of left cheek
Primary Management
Wound toilet under copious irrigation, debridement of dead tissue, removal of bone and tooth fragmens, layered wound closure, drainage, and temporary fixation.In wounds with extensive soft and hard tissue damage and true loss of soft and hard tissue, an approach using early stabilization of bone fragments with IMF, external fixation, or internal fixation with reconstruction plates combined with conservative management of soft tissue is indicated.
Late management
Bone GraftingBone grafts are frequently required in the management of GSWs to the face, whether for replacement of true loss of bone (avulsive injuries) or in cases in which comminuted and misplaced fragments need to be replaced or reinforced.
Improvements in imaging and fixation techniques have resulted in an evolution in management, with an emphasis on earlier repair and a focus on improvement in quality of life.