بسم الله الرحمن الرحيم
a.c. 17/01/2021 1442 هجريHospital-Acquired Pneumonia
OBJECTIVESTo know
the epidemiology ,
etiology,
pathogenesis ,
clinical presentation,
investigation ,
diagnosis ,
treatment ,
complication ,
prognosis
Hospital-acquired pneumonia
Hospital-acquired or nosocomial pneumonia is a new episode of pneumonia occurring at least 2 days after
admission to hospital
It is the second most common hospital-acquired infection (HAI) and the leading cause
of HAI-associated death.
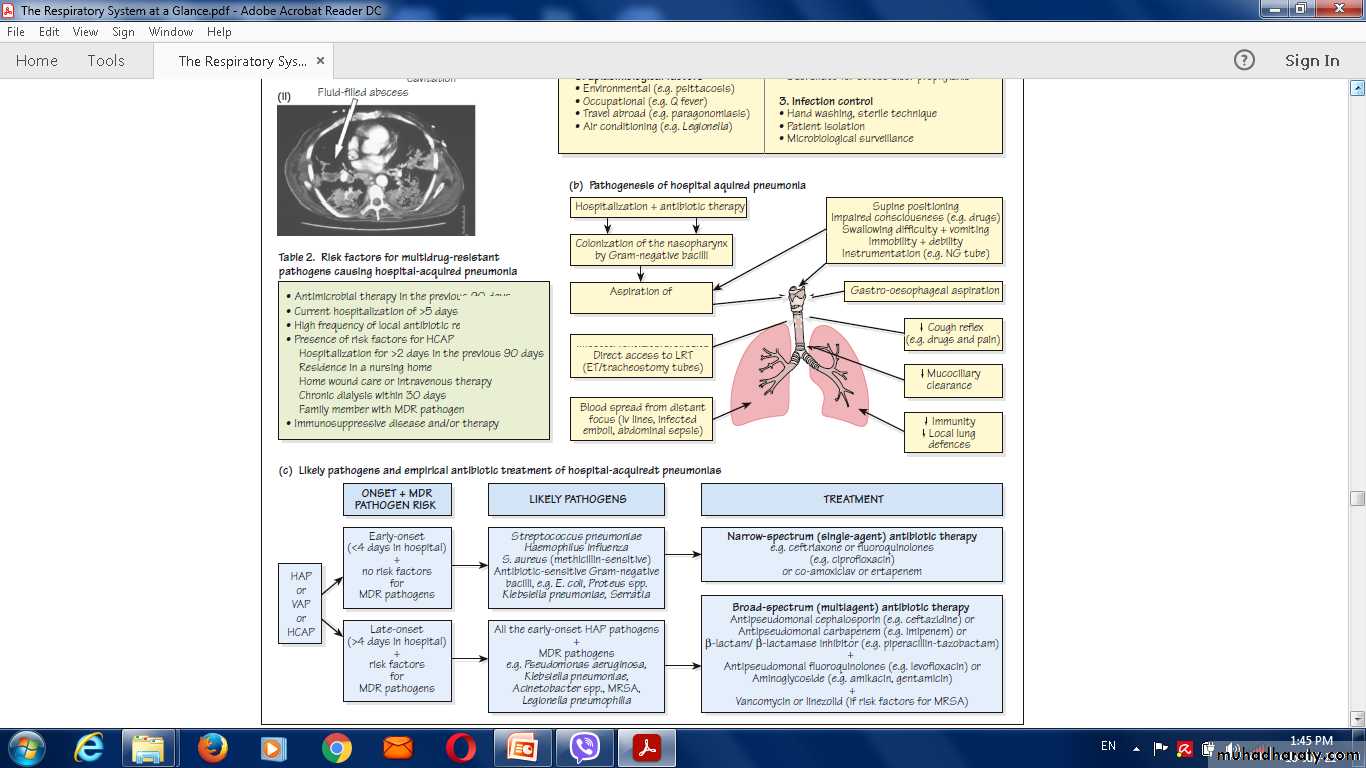
Classification of HAP
Ventilator-associated pneumonia’ (VAP)Pneumonia occurred patients in intensive care units, especially when mechanically ventilated;
Healthcare-associated pneumonia (HCAP)
pneumonia in a person
who has spentat least 2 days in hospital within the last 90 days.
has attended a haemodialysis unit.
Received intravenous antibiotics .
Been resident in a nursing home or other long-term care facility
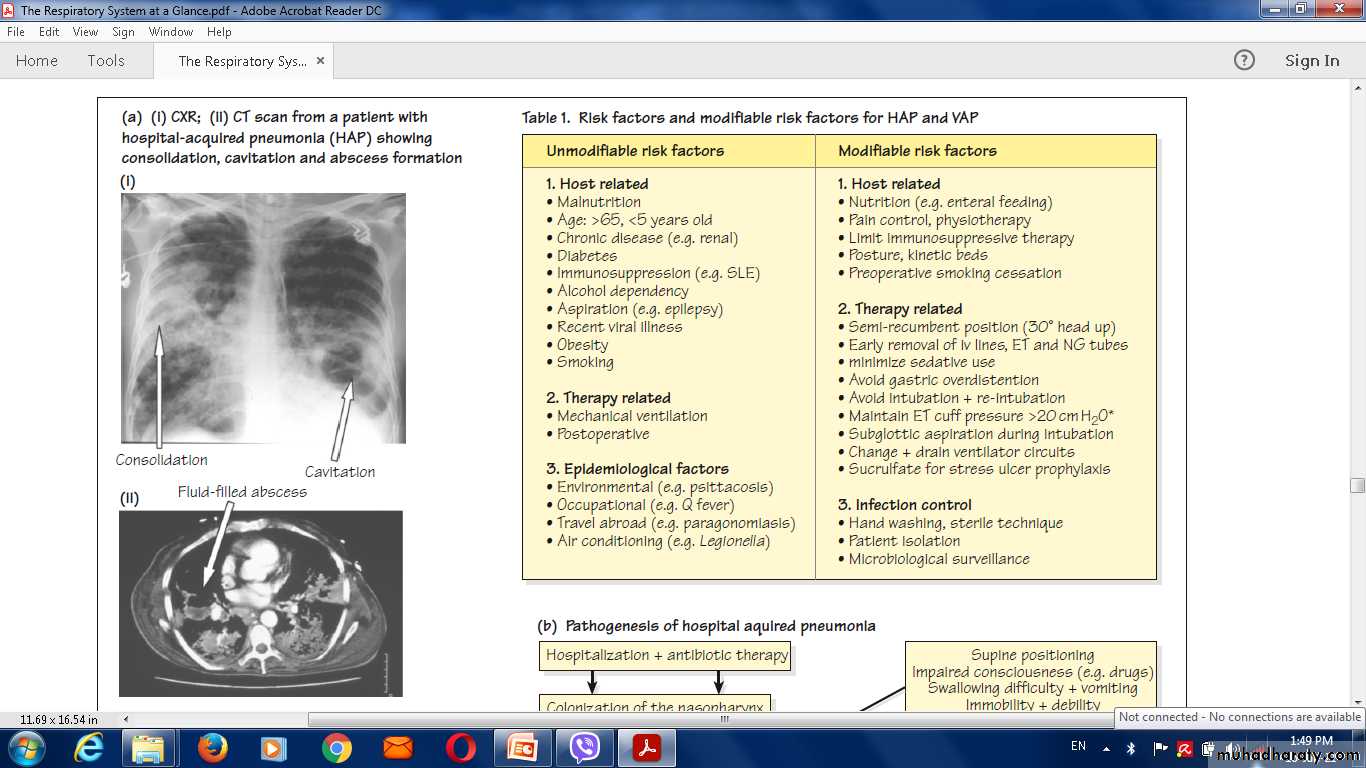
Factors predisposing to hospital-acquiredpneumonia
Reduced host defences against bacteria• Reduced immune defences (e.g.corticosteroid treatment, diabetes, malignancy)
• Reduced cough reflex (e.g. post-operative)
• Disordered mucociliary clearance (e.g. anaesthetic agents)
• Bulbar or vocal cord palsy
Aspiration of nasopharyngeal or gastric secretions
• Immobility or reduced conscious level
• Vomiting, dysphagia (N.B. stroke disease), achalasia or severe reflux
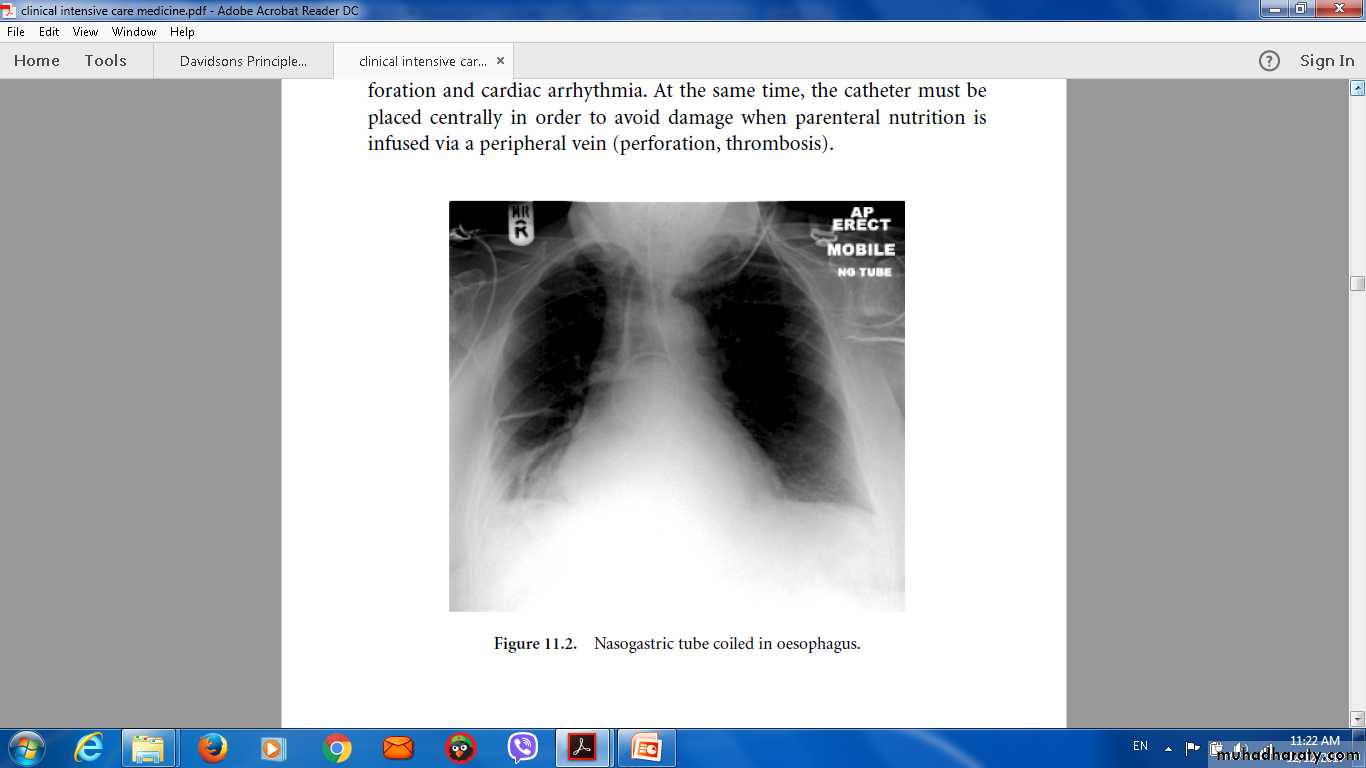
• Nasogastric intubation
Bacteria introduced into lower respiratory tract
• Endotracheal intubation/tracheostomy
• Infected ventilators/nebulisers/bron-choscopes
• Dental or sinus infection
Bacteraemia
• Abdominal sepsis
• IV cannula infection
• Infected emboli
Microbiology
The early-onset HAP (occurring within 4–5 days of admission) are similar to those involved in CAP.
Late onset HAP
Gram-negative bacteria (e.g. Escherichia, Pseudomonas, Klebsiella species and Acinetobacterbaumannii),
Staph. aureus (including the meticillinresistant
type (MRSA)) and anaerobes
Clinical features
The hospitalised or ventilated patient .Purulent sputum (or endotracheal secretions).
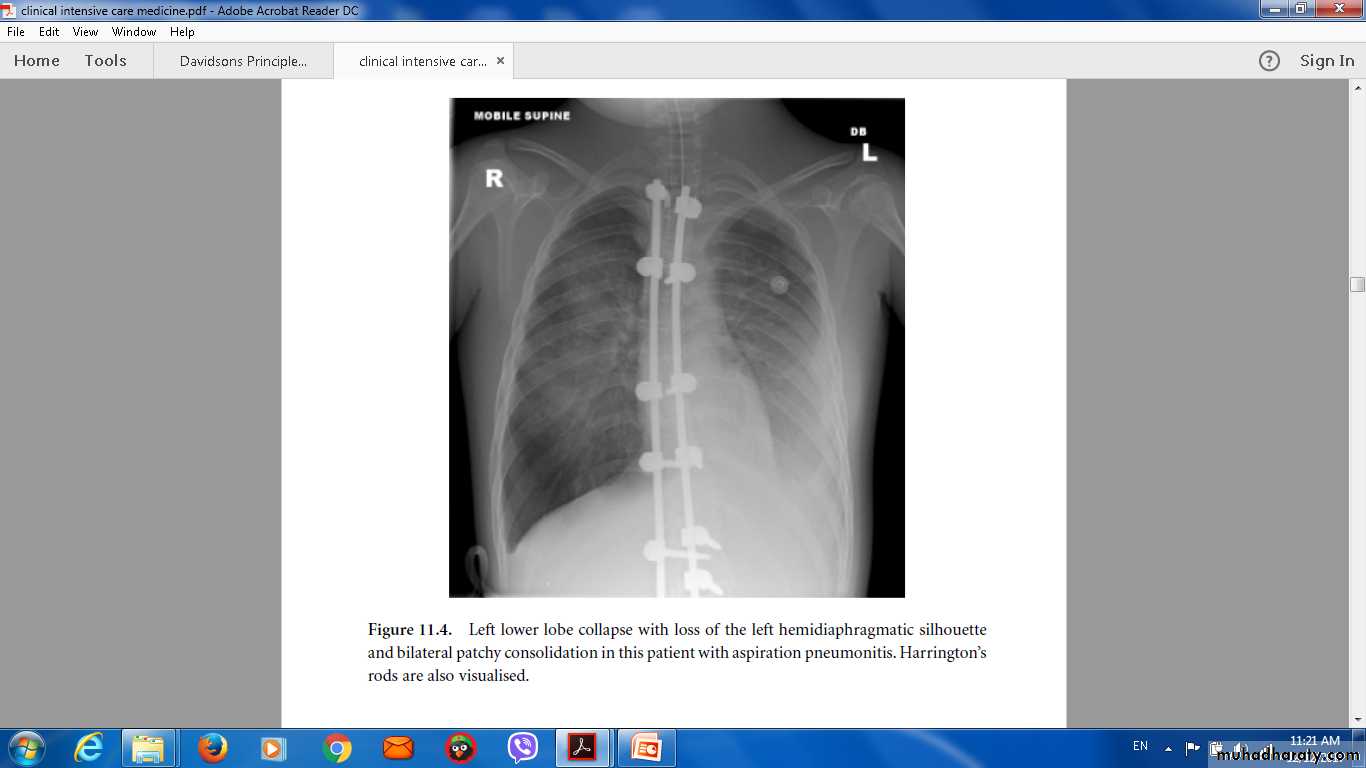
New radiological infiltrates.
Unexplained increase in oxygen requirement,
A core temperature of more than 38.3°C,
A leucocytosis or leucopenia.
Differential diagnosis
Venous thromboembolism .ARDS .
Pulmonary oedema.
Pulmonary haemorrhage.
Drug toxicity.
Investigations
Microbiological confirmation .
The full blood count (FBC).
Urea and electrolytes (U&E),
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
Arterial blood gas.
Chest X-ray.
Management
Adequate oxygenation.Appropriate fluid balance.
antibiotics.
Treatment
In early-onset HAP,1-If not received antibiotics
treated with co-amoxiclav or
cefuroxime.
2- Received antibiotics piperacillin/tazobactam
or a third generation
Cephalosporin..
In late-onset HAP,
the antibiotics must cover the
1-Gram-negative bacteria
2-Staph. aureus (including MRSA)
3- anaerobes.
Prevention
The mortality from HAP is approximately 30%,Good hygie regard to handwashing and any equipment used.
The risk of aspiration should be minimised,
ventilator associated pneumonia by limiting use of proton pump inhibitors.
decontaminate the upper airway, by Oral antiseptic (chlorhexidine 2%)
selective decontamination of the digestive tract.
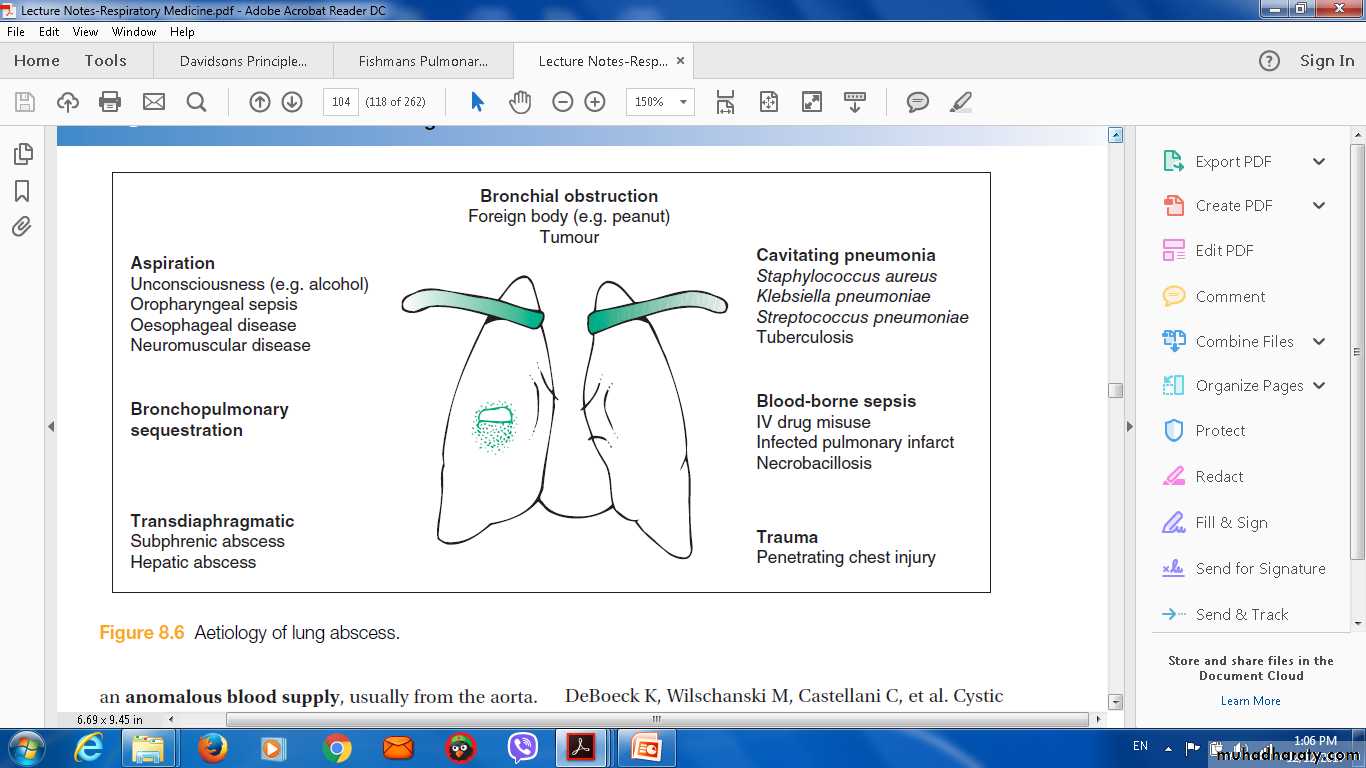
Suppurative pneumonia, Aspirationpneumonia and Pulmonary abscess
These conditions are considered together, as their aetiology and clinical features overlapSuppurative pneumonia is characterised by destruction of the lung parenchyma by the inflammatory process .
Microabscess formation is a characteristic histological feature.
Pulmonary abscess’ is usually taken to refer to lesions in which there is a large localised collection of pus, or a cavity lined by chronic inflammatory tissue, from which pus has escaped by rupture into a bronchus.
Risk
Inhalationseptic material during operations on the nose, mouth or throat under general anaesthesia,
vomitus during anaesthesia coma, particularly if oral hygiene is poor.
bulbar palsy
vocal cord palsy,
stroke,
achalasia
oesophageal reflux,
alcoholism.
local bronchial obstruction from a neoplasm or foreign body.
Aetiology of lung abscess
Microbilogy
Mixture of anaerobes and aerobes from flora in the mouth and upper respiratory tract.In a previously healthy lung,
Staph. aureus
Klebsiella pneumoniae.
Pulmonary infarct or a collapsed
Strep. pneumoniae, Staph. aureus, Strep. pyogenes,
H. influenzae and, in some cases, anaerobic bacteria.
In many cases, no pathogen can be isolated, particularly when antibiotics have been given.
Clinical Features of Suppurative Pneumonia
Symptoms• Cough with large amounts of sputum, sometimes fetid and blood-stained
• Pleural pain common
• Sudden expectoration of copious amounts of foul sputum if abscess ruptures into a bronchus
Clinical signs
• High remittent pyrexia
• Profound systemic upset
• Digital clubbing may develop quickly (10–14 days)
• Consolidation on chest examination; signs of cavitation rarely found
• Pleural rub common
• Rapid deterioration in general health, with marked weight loss if not adequately treated
Investigations
Radiological features
Abscesses are characterised by cavitation and fluid level.
Occasionally, a preexisting emphysematous bulla becomes infected and appears as a cavity containing an air–fluid level
Managment
ANTIBIOTICSIntravenous co-amoxiclav 1.2 g 3 times daily.
Metronidazole 500 mg 3 times daily If an anaerobic bacterial infection is suspected (e.g. from fetor of the sputum), oral
Other can be use
trimethoprim/sulfamethoxazole,
Clindamycin,
Parenteral therapy with
Vancomycin
Clindamycin and third-generation cephalosporins.
Prolonged treatment for 4–6 weeks may be required in some patients with lung abscess.
Physiotherapy
Prognosis
In most patients, there is a good response to treatment and, although residual fibrosis and bronchiectasisSurgery may be required.
Pneumonia in theimmunocompromised patient
Patients immunocompromised by drugs or disease are at high risk of pulmonary infection.The majority of cases are caused by the same pathogens that cause pneumonia
Patients with more profound immunosuppression, unusual organisms or those normally considered to be of low virulence or non-pathogenic may become ‘opportunistic’pathogens
Clinical features
fever,cough
breathlessness,
Diagnosis
Invasive investigations, such asBronchoscopy.
BAL.
Transbronchial biopsy.
Surgical lung biopsy.
Management
Broad-spectrum antibiotic
a third-generation cephalosporin or aquinolone,
plus an antistaphylococcal antibiotic,
Or
an antipseudomonal penicillin plus an aminoglycoside.
Antifungal
ANTIVIRAL
Respiratory infection in old age
Increased risk of and from respiratory infection.Predisposing factors: .
Atypical presentation .
Mortality
Influenza
TB