
Complications of PUD:-
Objectives
1. What are the complications of PUD?
2. How could a patient with perforated DU present to you?
3. Gastric outlet stenosis.
These are
1. Perforation
2. Gastric outlet obstruction
3. Hemorrhage
Perforation:-
It occurs when the ulcer lies in the anterior wall of the duodenum usually, it
occur in the duodenum more than gastric, one forth of all perforation in acute
PU (NSAID)
Pathophysiological effect:-
When perforation occurs
1.
the content of the stomach escape into the peritoneal cavity ( peritonitis ),
because the escaped fluid contain large amount of an irritant enzymes and food
particles , therefore , the pt will have severe pain of sudden onset . the pt can
give the time exactly when the pain started, he will describe it as explosive
( pain in the epigastrium radiating to the shoulder tip increase with respiration
due to diaphragmatic irritation
The abdomen will be immobile and there is generalized board like rigidity,
bowel sound +ve . liver dullness to percussion is decreased due to the presence
of the gas under the diaphragm
2. Then fluid will collect in the abdomen, therefore the pain will decrease but
the rigidity still present, the pt will get rest (minor)
3. Deterioration then will be rapid and get shock.
Investigations:-
1. abdominal x- ray in erect position
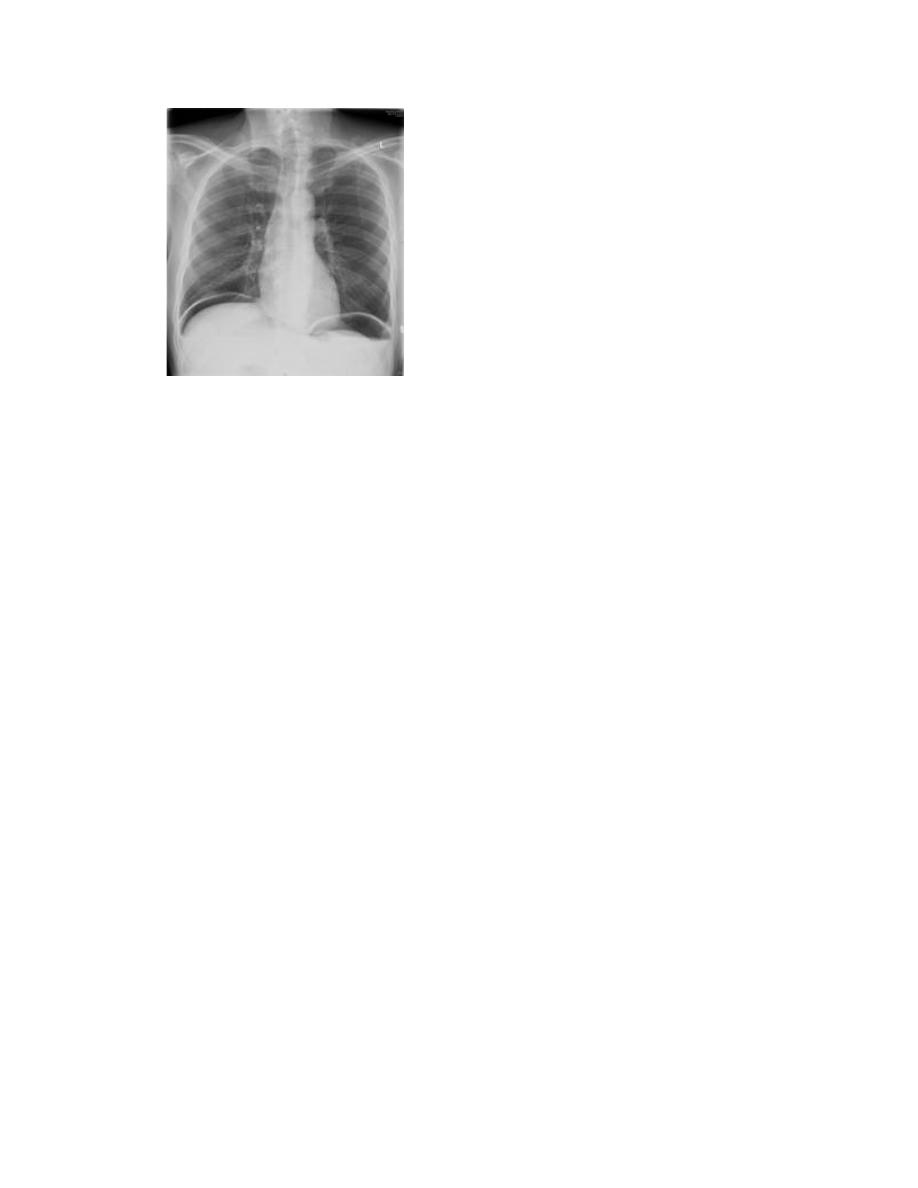
a. air under diaphragm in 50 %,
it may occur on the lateral border of the
abdomen especially in supine position
b. signs of intestinal obstruction may occur.
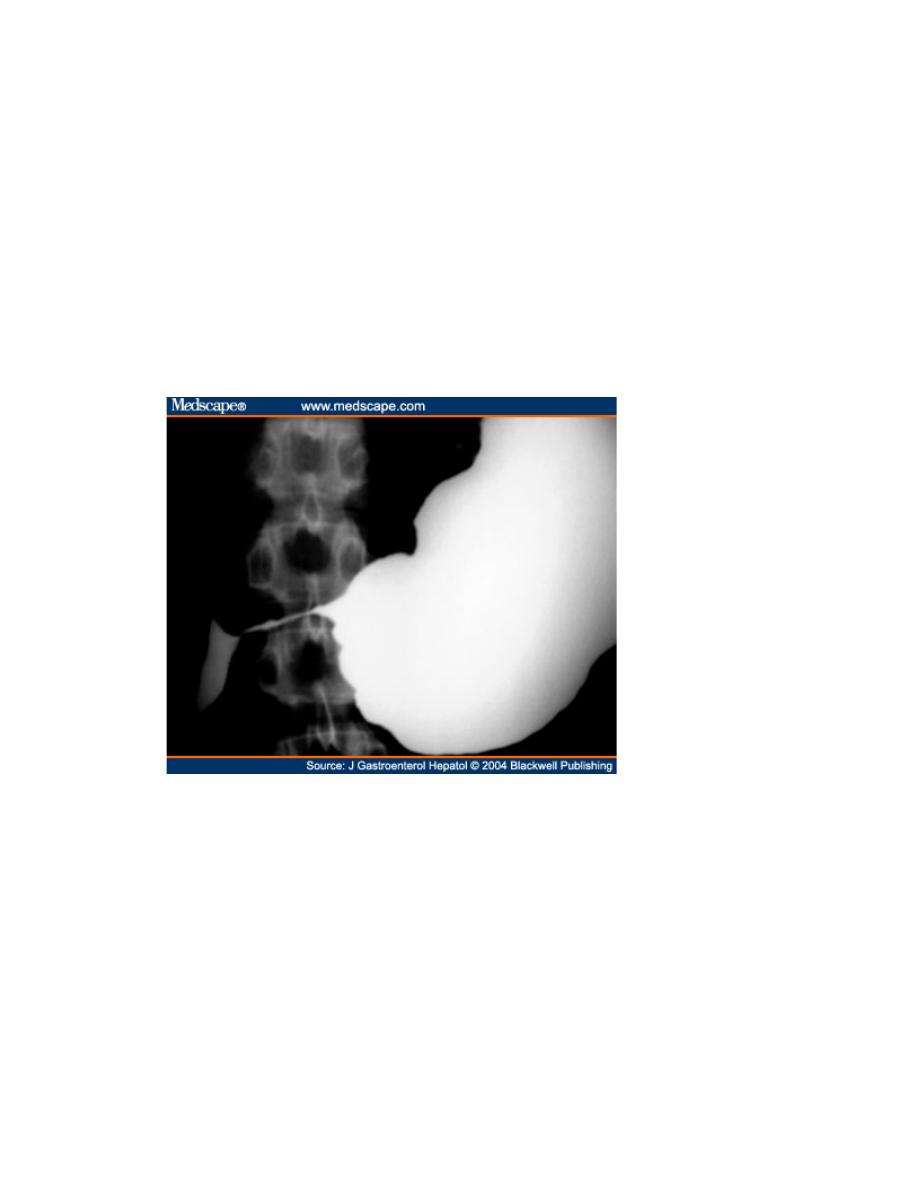
2. water soluble contrast swallow will confirm leakage of gastro duodenal
content.

Management:-

1. Resuscitation – NBM
- iv fluid
- Prepare blood.
3. Surgery is a must by a. simple closure
b. by converting the perforation into pyloroplasty if
it is large .
c. polya operation (partial gastrectomy)
d. H pylori eradication and NSAIDs avoidance.
Prognosis:-
Mortality of 25% in advance age
and
significant morbidity.
2. Gastric outlet obstruction:-
Causes
1. fibrotic strictures from duodenal ulcer( pylorus stenosis) which will be
treated by balloon dilatation or surgery
1. Edematous pylorus from PU in the pyloric channel. This is treated
conservatively by PPI .
2. CA antrum = surgery is treatment of choice
3. adult hypertrophy pyloric stenosis .= surgery is the treatment of choice.
Sign and symptoms
:-
Symptom
1. nausea vomiting and abdominal distention
2. vomiting of food eating before 24 hours and large quantities of gastric
secretion
3. usually pt has long history of epigastric pain due to PU
Sign
4. wasting and dehydration
5. suction splash (4 hours or more after the last meal or drink )
6. Visible gastric peristalsis is diagnostic of gastric outlet obstruction.
Investigations:-
1. metabolic alkalosis due to
a. loss of gastric content and gastric HCL and K
b. increase serum bicarbonate and urea
c. enhance renal absorption of Na in exchange for (H+ ) and paradoxical
acid urea.
2. Nasal gastric aspiration of at least 200 ml of fluid from the stomach after
and overnight fasting suggest diagnosis .
3. endoscope should be performed after the stomach has been embedded
by wide bore N|G tube .
Balloon dilatation of benign stenosis may be possible in some pt
4. barium studies of no benefit , Ba is difficult to be removed from the
stomach
5. Saline load test : give 750 ml of saline by NG tube , more than 400 ml of
gastric guise after 30 min.
Management:-
1. Suction and intravenous correction of dehydration.
2. in severe cases at least 4 letters of isotonic saline and 80 ml of K is
given during the first 24 hours.
3. Correction of metabolic alkalosis is needed.
4. an attempt should be made to treat all pt medically by PPI and
conservative treatment

5. at least half of the pt so treated respond to therapy especially if the cause
is pyloric edema which resolve with in 7 days
6. If obstruction persist after 7 days surgery is indicated at that time .
Bleeding of PU
Under heading of upper GIT bleeding
Clinical indication for serum gastrin hormone measures
1. Family history of PU.
2. PU and hyper calcium or other manifestation of MEN (multiple endocrine
neoplasia.)
3. multiple ulcers
4. PU of post bulbar duodenum or jejunum
5. PU and diarrhea
6. chronic unexplained diarrhea
7. enlarged gastric folds in x- ray series
8. before surgery for intractable ulcer
9. recurrent ulcer after ulcer surgery
Zollinger – Ellison syndrome
rare disorder characterized by presence of CA pancreas ( non B-cell tumor )
with excessive gastrin secretion stimulate the acid secretion from the stomach
with shift of that acidity to the first part of duodenum or jejunum = very large
PU with inactivation of lipase leads to less digestion of fat and inactivation of
bile salt , leads to diarrhea and steatorrhea
Diagnosis:-
Is suspected in severe , extensive , multiple ulceration , or if it occur at
abnormal site as jejunum or esophagus or if PU or diarrhea or increase Ca level
in serum due to MEN 1 disease (PPP adenoma , pituitary , parathyroid and
pancreatic adenoma )

Treatment:-surgery.
Dyspepsia
Dyspepsia describes symptoms such as discomfort, bloating
and nausea, which are thought to originate from the upper
gastrointestinal tract. There are many causes, including some arising
outside the digestive system. Heartburn and other ‘reflux’ symptoms
are separate entities and are considered elsewhere. Although
symptoms often correlate poorly with the underlying diagnosis, a
careful history is important to detect alarm’ and features requiring
urgent investigation to detect atypical symptoms that might be due to
problems outside the gastrointestinal tract.

Causes of dyspepsia:
Upper gastrointestinal disorders
• Peptic ulcer disease
• Acute gastritis
• Gallstones
• Oesophageal spasm
• Non-ulcer dyspepsia
• Irritable bowel syndrome
Other gastrointestinal disorders
• Pancreatic disease (cancer, chronic pancreatitis)
• Colonic carcinoma
• Hepatic disease (hepatitis, metastases)
Systemic disease
• Renal failure
• Hypercalcaemia
Drugs
• Non-steroidal antiinflammatory drugs (NSAIDs)
• Glucocorticoids
• Iron and potassium supplements
• Digoxin
Others
• Psychological (anxiety, depression)
• Alcohol
Alarm features of dyspepsia:
.Weight loss
• Anaemia
• Vomiting
• Haematemesis and/or melaena
• Dysphagia
• Palpable abdominal mass
Dyspepsia affects up to 80% of the population at some time
in life and most patients have no serious underlying disease
.

People who present with new dyspepsia at an age of more
than 55 years and younger patients unresponsive to empirical
treatment require investigation to exclude serious disease.
Non ulcer dyspepsia
Abdominal discomfort and fullness or nausea may occur post eating although
no PU by OGD . it may be due to psychological causes , female more than
male 2:1
Diagnosis by exclusion of PU and other dis
Treatment :-
- reassurance
- symptomatic treatment
- antidepressant therapy.
Function causes of vomiting;
Vomiting at morning due to psychological instability
DDx;-
1. pregnancy
2. alcohol
3. Depression.
Gastroparesis:-
Lazy stomach, due to abnormal gastric motion with delay emptying, may be
due to DU.
, neuropathy or infiltrative dis as amyloidosis
Or systemic sclerosis, drug effect electrolyte and metabolic disorders
Treatment:-
1. Symptomatic and treat the cause.
2. Surgery jujenostomy.
3. Metoclopramide and cisaprid.
4. erythromycin may interact with motilin receptor in the stomach
5. Ciprofloxacin may be of benefit also.

-
