
Gastrointestinalbleeding
L8
Acuteuppergastrointestinalhemorrhage
1. What are the causes of upper GIT bleeding?
2. Sign and symptoms of upper GIT bleeding.
3. Physical Examination and assessment.
4. Management of upper GIT bleeding.
This is the most common gastrointestinal emergency, accounting for large numbers of
population admissions to hospital each year. And with mortality of about 10%.
The common causes of upper GI bleeding are:
1. Peptic ulcer (35-50%): duodenal or gastric ulcer, which is caused by either NSAIDs or
H. pylori.
2. Gastric erosions (10-20%): which is caused either by NSAIDs or alcohol.
3. Esophagitis (10%): usually with hiatus hernia.
4. Oesophagogastric varices (2-9%): which is caused either by liver disease or portal vein
thrombosis.
Occur due to chronic liver disease lead to portal hypertension (defined as elevation of
hepatic venous pressure gradient to >5mmHg),this response for causing oesophageal
varices which is most important clinical feature of portal hypertension , commonly
located within 3-5cm of the oesophagogastric junction or from gastric varices.
There are several factors predict the risk of bleeding:
a. Severity of liver cirrhosis (Child's class)
b. Height of wedged-hepatic vein pressure.
c. Size & location of varix (certain endoscopic stigmata).
d. Patient with tense ascites.
5.Mallory-Weiss oesophageal tear (5%): caused by retching (gastric & oesophageal
movements of vomiting without expulsion of vomitus) , coughing & vomiting causing
mucosal tears at gastroesophageal junction.
It's often associated with alcoholism and eating disorder and it may be seen in pregnancy
also and there is some evidence that presence of hiatal hernia is predisposing condition.
6.Vascular malformations (5%): which cause recurrent & relapse bleeding. Such as :
bleeding disorder (hemophilia) , gastroduodenal vascular malformations , Osler-Weber-
Rendu syndrome (hereditary hemorrhagic telangiectasia) characterized by thinning of the
blood vessel wall resulting in abnormally wide & fragile blood vessels.patients may bleed
from nose,skin,lung,brain,mucous memb.,acute & chronic digestive tract bleeding.
7.Cancer of stomach or oesophagus (2%).
8.Aorto-duodenal fistula (0.2%): Which is caused by aortic graft & it's divided into:

Primary: is rare, in which communication between the lumen of the aorta & that of the
duodenum, when such a fistula occur in the absence of previous aortic aneurysm surgery.
Secondary: Which occurs as a result of previous aortic aneurysm surgery.
Any bleeding from the mouth down to the ascending colon leads to melena and any
b;eeding from the muoth down to the third part of the duodenum leads to heamatemesis.
Very rarely bleeding from the upper GIT leads to fresh bleeding per rectum
(haematochezia) if the bleeding is acute very severe.
Symptoms and Signs of Upper Gastrointestinal tract bleeding
1. Abdominal Pain or Epigastric pain
2. Hematemesis or coffee ground vomitus. May be red with clots when the bleeding
is profuse or black(coffee ground) when less severe.
3. Black tarry stools or Melena
4. Bright red blood per rectum or Hematochezia (if bleeding is brisk)
5. Weakness
6. Shortness of breath
7. Pale appearance
8. Syncope
9. Presyncope
10. Dyspepsia
11. Heartburn
12. Dysphagia
13. Weight loss
14. Jaundice
15. Long-term GI bleeding may go unnoticed or may cause fatigue, anemia( may
indicate chronic bleeding with haemodilution or chronic liver disease), black stools
16. Melena from upper GIT bleeding if the bleeding is severe leads to haematochesia.
History is very important as previous(pain, vomiting, weight loss)or pass medical
history(previous episodes, ulcer, liver disease) and ingestion of (alcohol, aspirin,
alcohol, steroids and NSAID).
The history and physical examination
A. History findings include weakness, dizziness, Haematemesis is red with clots
when bleeding is profuse, or black (‘coffee grounds’) when less severe.
B. Symptoms of anaemia suggest chronic bleeding.
C. Melaena is the passage of black, tarry stools containing altered blood; it is usually
caused by bleeding from the upper gastrointestinal tract
D.A brisk UGIB manifests as hematochezia (red or maroon stools); the redder the
stool, the more rapid the transit, which suggests a profuse upper tract hemorrhage.
E. Syncope may occur and is due to hypotension from intravascular volume depletion.
F. Patients may have a history of dyspepsia
G. Many patients with UGIB who are taking NSAIDs may present without dyspepsia
but with hematemesis or melena as their first symptom, owing to the analgesic
effect of the NSAID
H. A history of chronic alcohol use of more than 50 g/d or chronic hepatitis (B or C)
increases the risk of variceal hemorrhage, gastric antral vascular ectasia (GAVE),
or portal hypertensive gastropathy.
Physical Examination and assessment
The goal of the patient's physical examination is to evaluate for shock and blood loss .
The physical examination performed by the physician concentrates on the following
things:
Vital signs, in order to determine the severity of bleeding and the timing of intervention
Abdominal and rectal examination, in order to determine possible causes of hemorrhage
Assessment for portal hypertension and stigmata of chronic liver disease in order to
determine if the bleeding is from a variceal source.
Lab findings include anemia, coagulopathy.
Vital Signs
Pulse and blood pressure should be check.
include tachycardia of more than 100 beats per minute (bpm), systolic blood pressure of
less than 90 mm Hg, cold extremities, syncope, and other obvious signs of shock, such as
ongoing brisk hematemesis or the occurrence of maroon or bright-red stools, which requires
rapid blood transfusion.
Other Signs
1.The presence of postural hypotension indicates more rapid and severe blood
loss.
2.Signs of chronic liver disease should be noted, including spider angiomata,
gynecomastia, splenomegaly, ascites, pedal edema.
Investigations:
Eyes are the best witness.
Fecal occult tests: may give
1.false negative when bleeding is intermittent
2.false positive when patient eats meat or iron containing drugs or bleeding per gum.
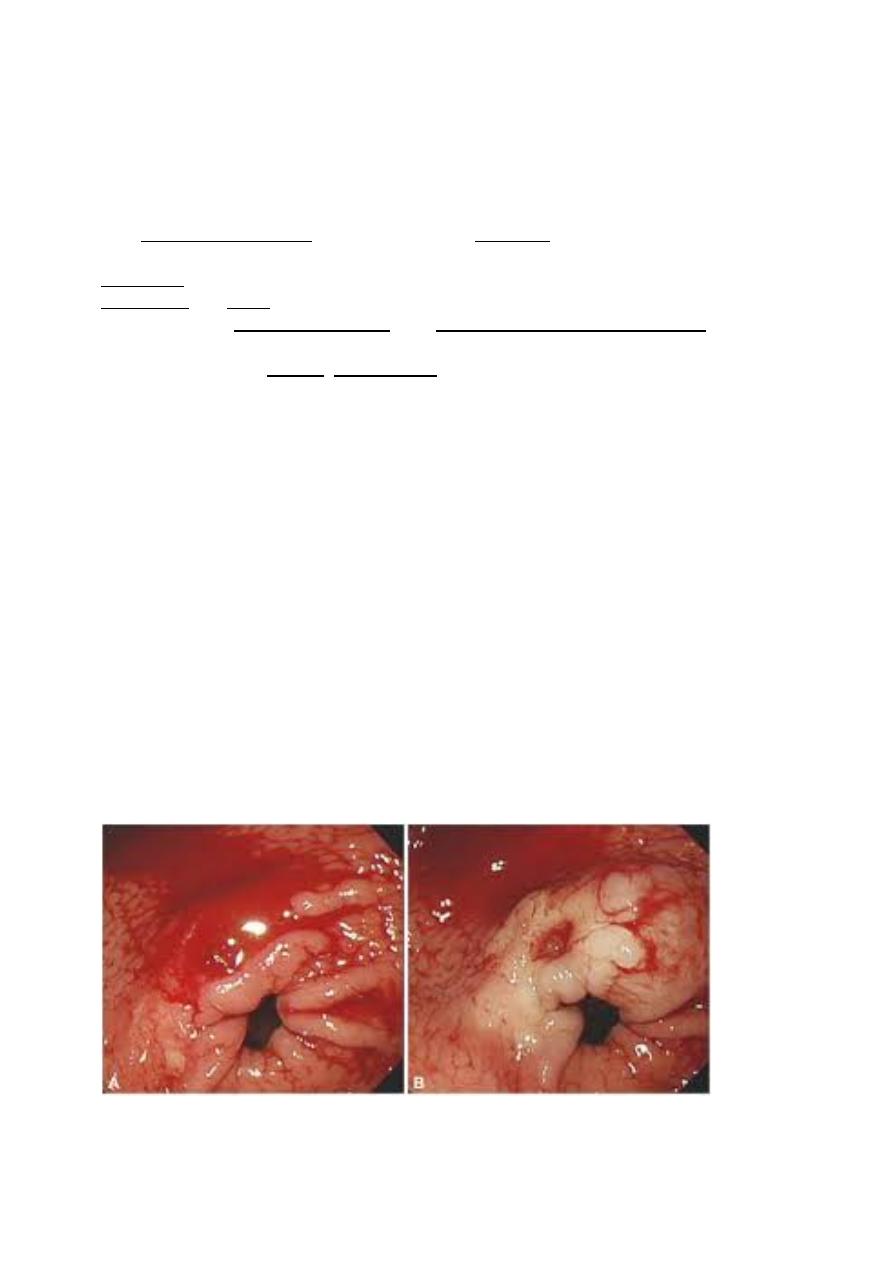
Endoscopy is a must for either diagnosis or therapy.
High risk patients:
1.Patients at higher risk of rebleeding

2.patients more than 70 years.
3.patients at other serious diseases.
4.hypovolumic shock.
5.evidence of chronic liver disease.
6.evidence of continued bleeding or rebleeding.
Management:
1.admit the patient to the hospital.
2.intravenous access.
It is the most important and first step using one or two large bore cannula or
CVP cannula.
3. initial clinical status assessment
a.assessment of circulatory status, if bleeding is severe: tachycardia, hypotention,
oliguria, the patient is cold, sweaty and agitated.
b. signs of chronic liver disease:
jaundice, cutaneous stigmata, hepatosplenomegaly and ascites may be present in
decompensated cirrhosis.
c. seek for signs of high risk patient.
Because patients with renal disease, respiratory disease or cardiac disease may
worsened by acute bleeding.
4. blood test:
*Complete blood count: acute bleeding doesn't change Hb because no time for
haemodilution, while chronic bleeding can do so.
*blood urea, S.creatinine, and serum electrolyte. Blood urea increase due to
absorption of luminal blood and metabolize by the liver later.
*liver function test: PT, INR,if the patient has signs of chronic liver disease or
patients received anticoagulants.
* blood group and cross match of at least two pints of blood.
5.resuscitation
Intravenous crystalloids fluids or colloid are given to restore the blood pressure.
Blood is transfused in
1.shoched patients.
2.Hb less than 10gm\dl
Normal saline should be avoided because it may leads to ascites in patient with
chronic liver disease
In patient with heart failure central venous pressure(CVP line)monitoring is
important during resuscitation .
6. O2 it should be given by mask to all patients with shock.
7. endoscope is a must after resuscitation and must not delay after 18 hour.
Diagnosis achieved in 80% of cases. If you find the bleeding site treat it
endoscopically by:
1.thermal modalityas heater probe.
2.by injection of diluted adrenaline into the bleeding points.
3.metalic clips.
4.lazer therapy,cryotherapy are other processes.

This injection will reduce ulcer rebleeding rate, the need for surgery, and
hospital mortality.
8. drug therapy for bleeding ulcer
intravenous proton pump inhibitors reduce rebleeding and need for surgery but
not mortality in patient who had been subjected to endoscopic therapy for
major peptic ulcer haemorrhage.
9.monitoring chart(hourly),pulse, BP, and urine output,
10. surgery indicated in
a. endoscopic hemostasis fails to stop active bleeding.
b.rebleeding occurs in once in an elderly or frail patients or twice in young or
fitter patients.
