
Alveoli
There are about 200 million alveoli in a normal lung. The total area of the alveolar
surface of each lung is extensive. It has been estimated to be about 75 square meters. The
total capillary surface area available for gaseous exchanges is about 125 square meters.
Structure of Alveolar Wall
Each alveolus has a very thin wall. The wall is lined by an epithelium consisting mainly
of flattened squamous cells. The epithelium rests on a basement membrane. Deep to the
basement membrane there is a layer of delicate connective tissue through which
pulmonary capillaries run. These capillaries have the usual endothelial lining that rests on
a basement membrane.
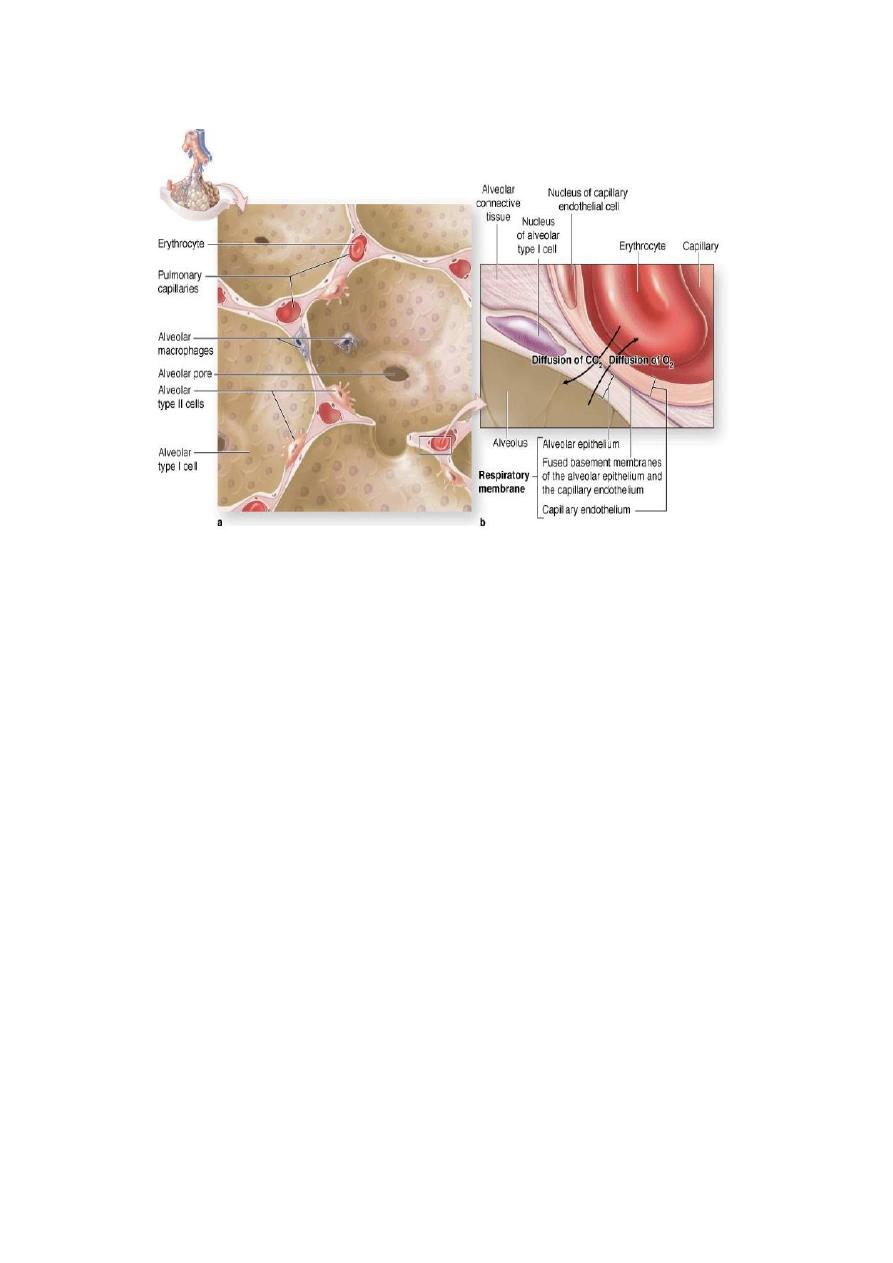
The barrier between air and blood is made up of the epithelial cells and their basement
membrane; by endothelial cells and their basement membrane; and by intervening
connective tissue. At many places the two basement membranes fuse greatly reducing the
thickness of the barrier.
The endothelial cells lining the alveolar capillaries are remarkable for their extreme
thinness. With the EM they are seen to have numerous projections extending into the
capillary lumen, these projections greatly increase the surface of the cell membrane that is
exposed to blood and is, therefore, available for exchange of gases. At many places the
basement membrane of the endothelium fuses with that of the alveolar epithelium greatly
reducing the thickness of the barrier between blood and air in alveoli.
Pneumocytes
EM studies have shown that the cells forming the lining epithelium of alveoli
(pneumocytes) are of various types .
‰
‰
1-
The most numerous cells are the squamous cells already referred to. They are called
type I alveolar epithelial cells
. Except in the region of the nucleus, these cells are
reduced to a very thin layer. The edges of adjoining cells overlap and are united by
tight junctions (preventing leakage of blood from capillaries into the alveolar lumen).
They form the lining of 90% of the alveolar surface.
‰
‰
2-
Scattered in the epithelial lining there are rounded secretory cells bearing microvilli
on their free surfaces. These are designated type II alveolar epithelial cells , their
cytoplasm contains secretory granules that appear to be made up of several layers .
These cells are believed to produce a secretion that forms a film over the alveolar
epithelium. This film or pulmonary surfactant reduces surface tension and prevents
collapse of the alveolus during expiration, type II cells may multiply to replace
damaged type I cells.
3-
Type III alveolar cells, or brush cells, of doubtful function, have also been described.
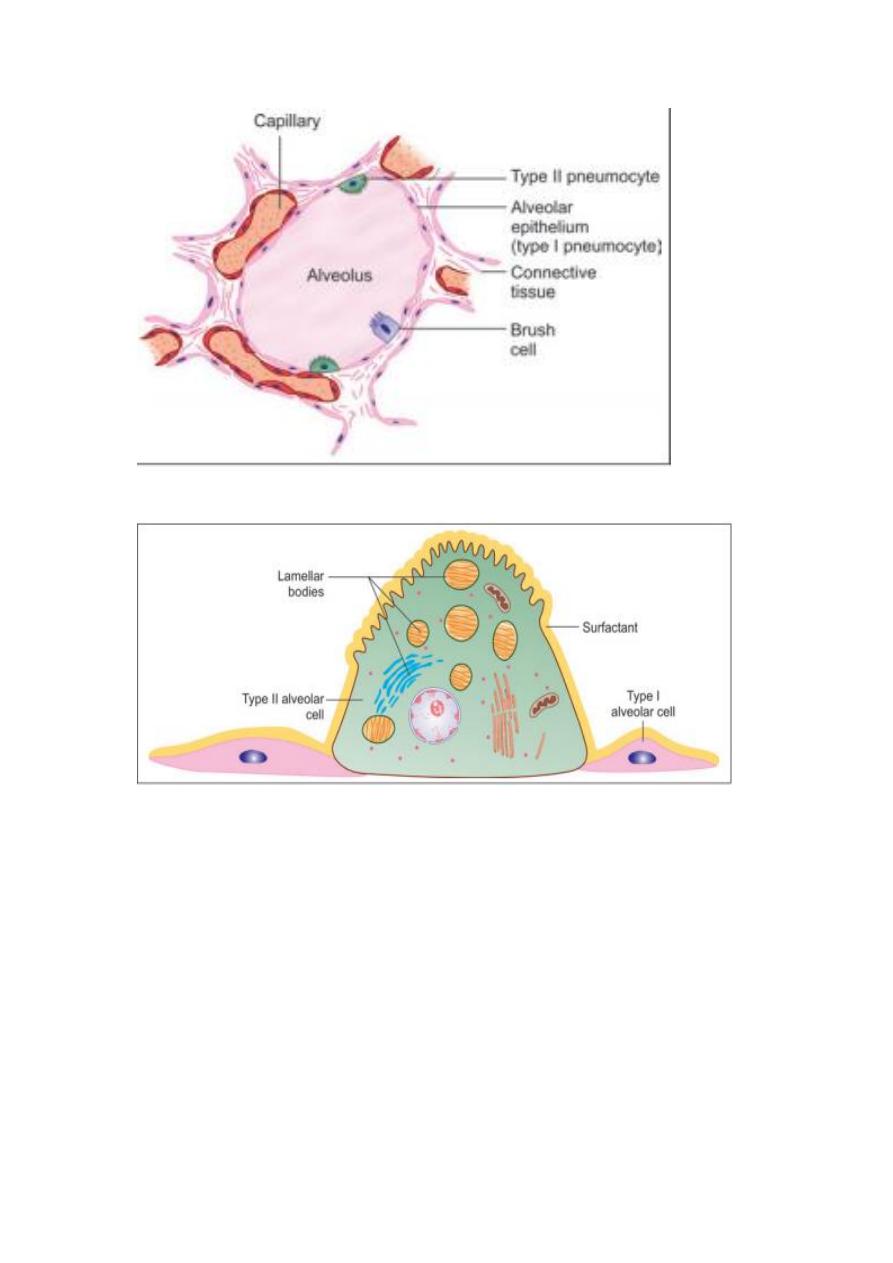
Connective Tissue
The connective tissue in the wall of the alveolus contains collagen fibers and
numerous elastic fibers continuous with those of bronchioles. Fibroblasts, histiocytes,
mast cells, lymphocytes and plasma cells may be present. Pericytes are present in
relation to capillaries.
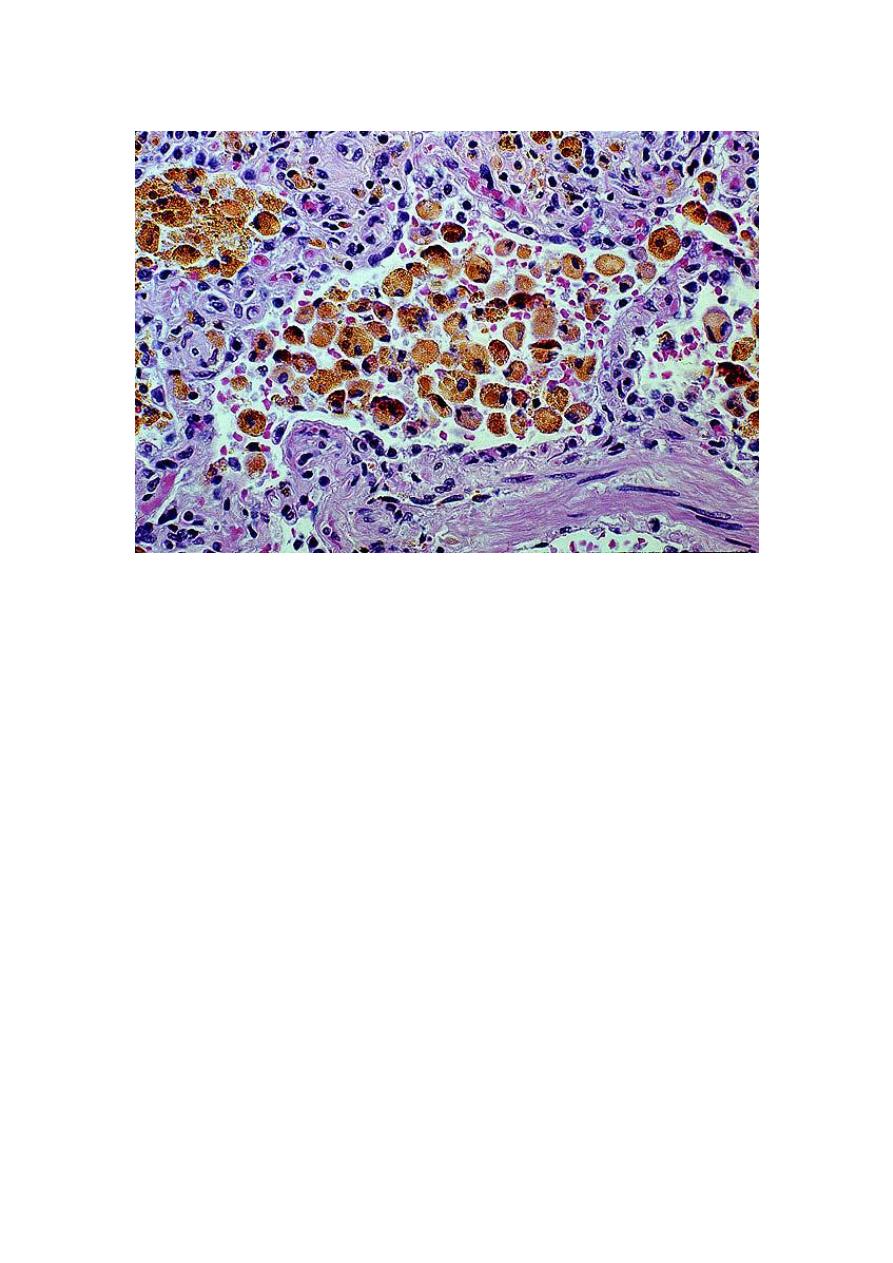
Some macrophages enter the connective tissue from blood and pass through the
alveolar epithelium to reach its luminal surface. Dust particles phagocytosed by them
are seen in their cytoplasm. They are therefore called dust cells. These dust cells are
expelled to the outside through the respiratory passages. In congestive heart failure (in
which pulmonary capillaries become overloaded with blood) these macrophages
phagocytose erythrocytes that escape from capillaries. The cells, therefore, acquire a
brick red color and are then called heart failure cells. Macrophages also remove
excessive surfactant, and secrete several enzymes.
Connective Tissue Basis of the Lung
The greater part of the surface of the lung is covered by a serous membrane, the
visceral pleura. This membrane consists of a layer of flattened mesothelial cells,
supported on a layer of connective tissue.
Deep to the pleura there is a layer of subserous connective tissue. This connective
tissue extends into the lung substance along bronchi and their accompanying blood
vessels, and divides the lung into lobules. Each lobule has a lobular bronchiole and its
ramifications, blood vessels, lymphatics and nerves.
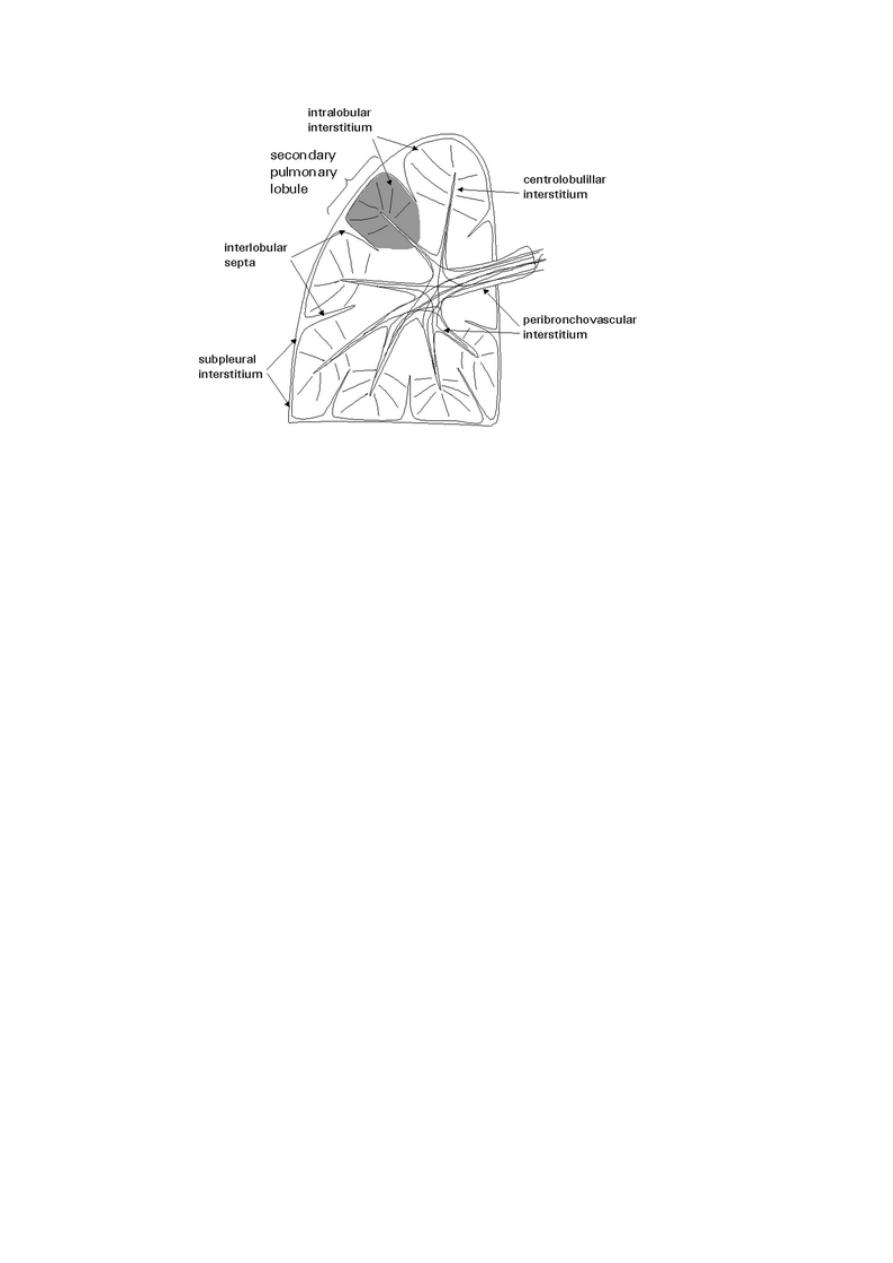
The epithelial lining of air passages is supported by a basal lamina deep to which
there is the connective tissue of the lamina propria. Both in the basal lamina and in the
lamina propria there are numerous elastic fibers. These fibers run along the length of
respiratory passages and ultimately become continuous with elastic fibers present in
the walls of air sacs. This elastic tissue plays a very important role by providing the
physical basis for elastic recoil of lung tissue. This recoil is an important factor in
expelling air from the lungs during expiration. Elastic fibers passing between lung
parenchyma and pleura prevent collapse of alveoli and small bronchi during
expiration.
Blood Supply of Lungs
The lungs receive deoxygenated blood from the right ventricle of the heart through
pulmonary arteries. Within the lung the arteries end in an extensive capillary network
in the walls of alveoli. Blood oxygenated here is returned to the left atrium of the
heart through pulmonary veins.
Oxygenated blood required for nutrition of the lung itself reaches the lungs through
bronchial arteries. They are distributed to the walls of bronchi as far as the respiratory
bronchioles. Blood reaching the lung through these arteries is returned to the heart
partly through bronchial veins, and partly through the pulmonary veins. Plexuses of
lymph vessels are present just deep to the pleura and in the walls of bronchi.
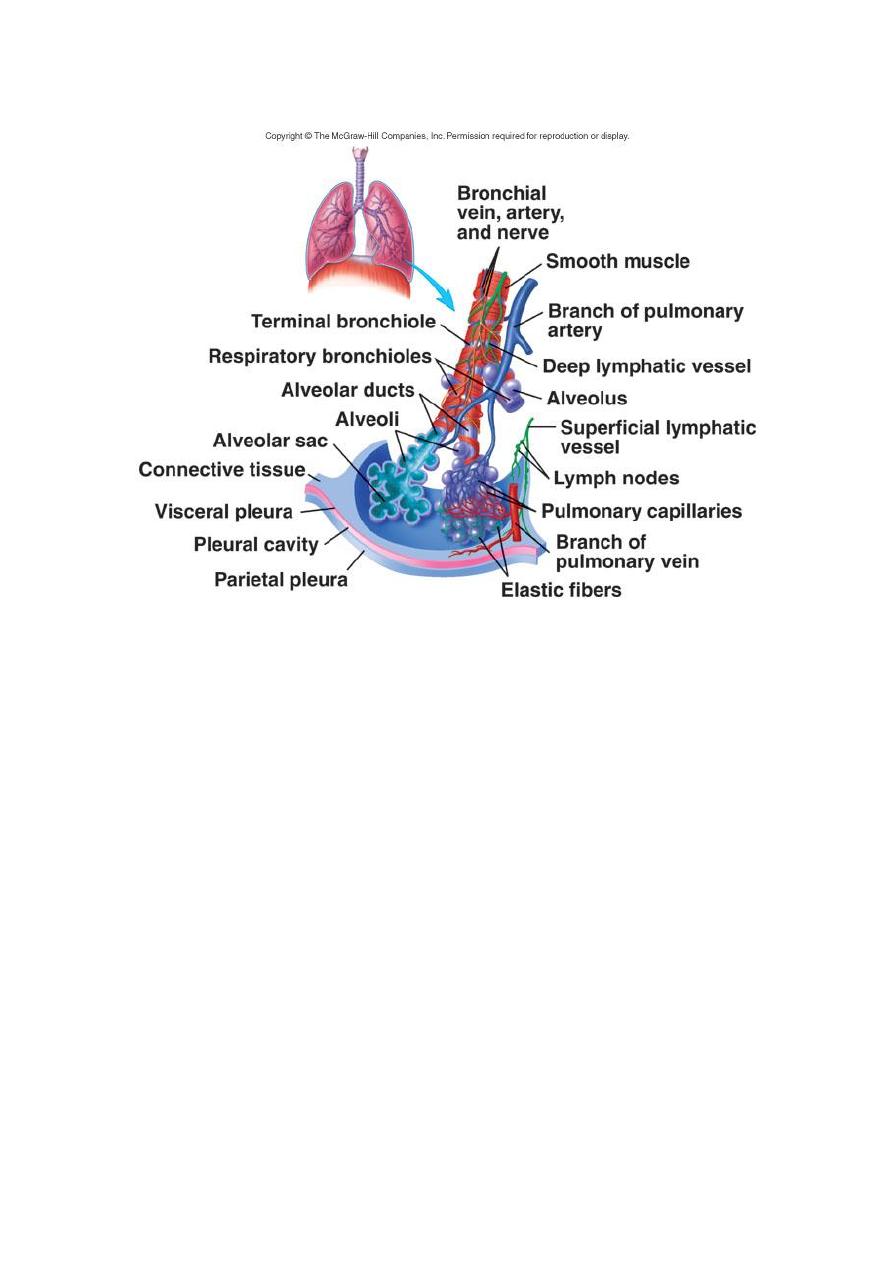
Nerve Supply of Lungs
The lungs receive autonomic nerves, both sympathetic and parasympathetic, and
including both afferent and efferent fibers. Efferent fibers supply the bronchial
musculature. Vagal stimulation produces bronchoconstriction. Efferent fibers also
innervate bronchial glands. Afferent fibers are distributed to the walls of bronchi and
of alveoli. Afferent impulses from the lungs play an important role in control of
respiration through respiratory reflexes.
PLEURAL MEMBRANES
The lung’s outer surface and the internal wall of the thoracic cavity are covered
by a serous membrane called the pleura . The membrane attached to lung tissue is
called the visceral pleura and the membrane lining the thoracic walls is the parietal
pleura. The two layers are continuous at the hilum and are both composed of simple
squamous mesothelial cells on a thin connective tissue layer containing collagen and
elastic fibers. The elastic fibers of the visceral pleura are continuous with those of the
pulmonary parenchyma. The narrow pleural cavity between the parietal and visceral
layers is entirely lined with mesothelial cells that normally produce a thin film of
serous fluid that acts as a lubricant, facilitating the smooth sliding of one surface over
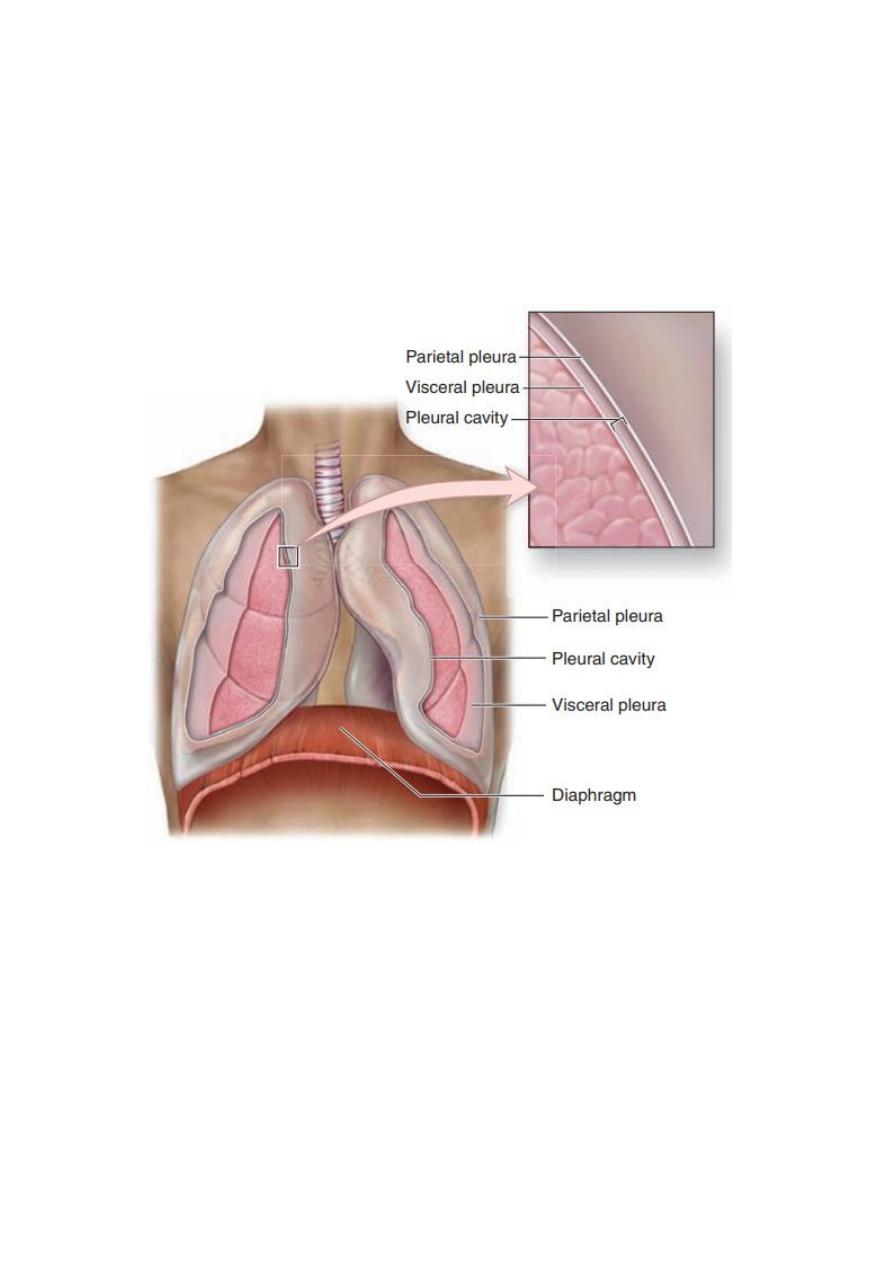
the other during respiratory movements. In certain pathologic states, the pleural cavity
may contain liquid or air. Like the walls of the peritoneal and pericardial cavities, the
serosa of the pleural cavity is water-permeable and fluid exuded from blood plasma
commonly accumulates (as a pleural effusion) in this cavity during inflammation and
other abnormal conditions.

