Clinical immunology L-3
Inflammation&THE INFLAMMATORY RESPONSE
Inflammation is the response of living tissue to damage.
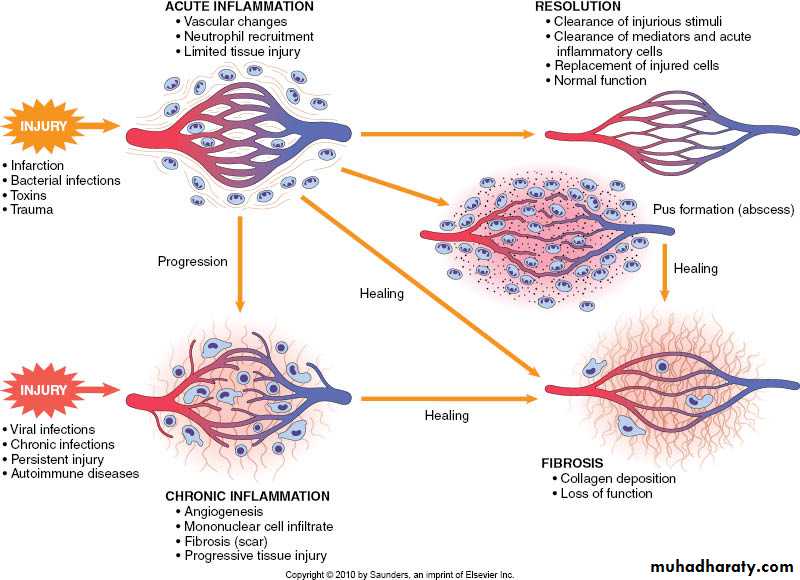
Types of inflammation:-Acute inflammation
-chronic inflammation
The cause of acute inflammation may be due to physical damage, chemical substances, micro-organisms or other agents.
Acute inflammation is short-lasting, lasting only a few days. If it is longer lasting however, then it is referred to as chronic inflammation. Various examples of acute inflammation such as sore throat, reactions in the skin to a scratch or a burn or insect bite, and acute hepatitis.
The Inflammatory Response3 Steps:
• 1. Tissue damage = release of chemical signals~
• Mast cells release chemicals known as Histamine & Prostaglandins that trigger inflammation• 2. Vessels dilation increases permeability of capillaries~
• Increased blood flow; leukocytes leak out to infected area
• Delivery of clotting factors & antimicrobial proteins
• 3. Phagocytosis of pathogens~
• WBC’s engulf microbes or damaged tissue
• Fever: leukocyte-released chemicals increase body temperature
The inflammatory response consist of changes in blood flow, increased permeability of blood vessels and escape of cells from the blood into the tissues. The changes are essentially the same whatever the cause and wherever the site.
• Immediate, early response
• Vasodilation• Vascular permeability
• Emigration of leukocytes into tissues
• Reactions of leukocytes in inflammation
• Recognition of microbes and dead tissues
• Removal of the offending agents
• Macrophage activation
• Leukocyte-mediated tissue injury
CLINICAL FEATURES OF ACUTE INFLAMMATION
1-skin--flushing, fever, sweating, swelling2-CNS--headache, confusion, anorexia
3-respiratory--
Increased respiratory rate, hypoxia4-heart--
Tachycardia, hypotension, flow murmur
5-endocrine—
Release of catecholamine, glucocorticoid hormones& insulin from pancreas.
6-LNs- enlarged lymph nodes, lymphocytosis
7-Bone marrow-
Increased production of neutrophils and macrophages.Cardinal signs of acute inflammation
• Celsus described the local reaction of injury in terms that have come to be known as the cardinal signs of inflammation.• These signs are:
• rubor (redness)
• tumor (swelling)
• calor (heat)
• dolor (pain)
• functio laesa, or loss of function (In the second century AD, the Greek physician Galen added this fifth cardinal sign)
Briefly, the steps involved in the acute inflammatory response are:
Small blood vessels adjacent to the area of tissue damage initially become dilated with increased blood flow, then flow along them slows down.Endothelial cells swell and partially retract so that they no longer form a completely intact internal lining.
.
• 3.The vessels become leaky, permitting the passage of water, salts, and some small proteins from the plasma into the damaged area (exudation). One of the main proteins to leak out is the small soluble molecule, fibrinogen.
4.Circulating polymorphs neutrophil initially adhere to the swollen endothelial cells (margination), then actively migrate through the vessel basement membrane (emigration), passing into the area of tissue damage
5.Later, small numbers of blood monocytes (macrophages) migrate in a similar way, as do Iymphocytes.
Resolution of inflammatory response is crucial for normal healing.
This involves active down-modulation of inflammatory stimuli &repair of the damage to nearby local tissues.Extravasated neutrophils undergo apoptosis& phagocytosed by macrophages together with microorganism.
Macrophages also synthesizes collagenase &elastase which breakdown local connective tissue & aid in the removal of debris.
Macrophages derived cytokines &platetate derived growth factors attract fibroblasts &promote the synthesis of new collagen, while angiogenic factors stimulate new vessel formation.
Sepsis and septic shock
Septic shock is the clinical manifestation of overwhelming inflammation.Failure of normal inhibitory mechanisms results in excessive production of pro-inflammatory cytokines by macrophages.
This result in hypotension, hypovolemia,
hypoperfusion& tissue edema.Uncontrolled neutrophil activation causes the release of proteases and oxygen free radicals within blood vessels.
Direct activation of the coagulation pathway combines with endothelial cell disruption to form clots within the damaged vessels.
This is what we call disseminated intravascular coagulation(DIC) which considered a medical emergency.
The clinical consequences include cardiovascular collapse, acute respiratory distress syndrome, multiorgan failure and often death.
most frequently results from infection with Gram-negative bacteria because
Lipopolysaccharide is particularly effective at activating the inflammatory cascade.Failure to remove an inflammatory stimulus results in chronic inflammation.
In other word, chronic inflammation can be defined as inflammation which continues past 1 month
Marked by
• -a loss of function
• - Fibroblast activity continues forming granuloma
Persisting microorganisms stimulate the ongoing accumulation of neutrophils, macrophages& activated T-lymphocytes.
If this is associated with local deposition of fibrous connective tissues, a granuloma may form.
This is a characteristic of infections such as tuberculosis and leprosy, in which the M.O. is protected by a cell wall which shields it from killing, inspite of phagocytosis.
In most cases, the development of active immune response is beneficial to the host& result in either clearance or control of infection with minimal local damage.
However ,vigorous or prolonged immune response may cause significant tissue damage. These are known as hypersensitivity reactions & may involve either antibody or cell-mediated responses.
INVESTIGATIONS
Leukocytosis is common. Platetate count may be increased. Chronic inflammation is commonly associated with normochromic normocytic anemia.C-Reactive Protein ( CRP ) is the most widely used clinical measure of acute inflammation, but levels of fibrinogen, ferritin &complement component may also be increased as part of the acute phase response, while albumin levels are reduced.
CRP is an acute phase reactant which opsonizes invading pathogens. Levels of CRP increase within 6-houres of an inflammatory stimulus & may rise up to 1000 folds.
Plasma half life of CRP is 19 hours, so levels fall in just few days once the stimulus is removed.
In contrast to CRP, the
ESR is an indirect measure of the acute phase response. It measures the rate of fall of erythrocytes through plasma, causing aggregation of red cells.Abnormal red cell morphology can make rouleoux formation impossible.
For these reasons, inappropriately low ESR occurs in spherocytosis, sickle cell anemia& microcytic anemia.IMAGING TECHNIQUES
A chest-x ray and abdominal CT-scan may identify the source of unknown infection or malignancy.Abdominal or pelvic ultrasound may identify hepatic lesions, abdominal nodes and local abdominal or pelvic abscesses.
An MRI scan is more appropriate for the diagnoses of soft tissue or bone/joint infections.
Echocardiography is used to look for vegetation & assess valve function in suspected bacterial endocarditis. White cell scans are rarely indicated, but may be useful in identification of the site of pyogenic infections.
An isotope scan may identify the evidence of malignancy or bone infection.
Familial Mediterranean Fever(FMF)This is the most common of the familial periodic fevers, predominantly affecting Mediterranean people, including Arabs, Turks, Sephardic Jews and Armenians.
It results from mutation of the pyrine gene, which is thought to regulate neutrophils-mediated inflammation.
FMF is characterized by painful attacks of fever associated with peritonitis , pleuritis and arthritis. It lasts from a few hours to four days.
During acute episodes CRP levels are markedly increased.
The majority of individuals have their first attack before the age of 20. The major complication of FMF is AA amyloidosis.
Colchicine significantly reduces the number of febrile episodes in 90% of patients, but does not stop an established attack.