
Middle Ear Diseases
Firas Al-Hameed
Thi-Qar Medical School

Acute Otitis Media
• A viral or bacterial infection of the middle ear and mastoid air cell
system that results in mucosal inflammation which is associated with
a middle ear effusion and results in a variable collection of symptoms
and signs.
• It is one of the most common illnesses in childhood, with a peak
incidence in the second 6 months of life
• Recurrent - three or more episodes in 6 months, or four to six
episodes in 12 months

Aetiology
• Viral infection
• The majority of episodes of AOM may be associated with viral infections
• Respiratory syncytial virus (RSV),influenza A virus, parainfluenza viruses,
adenoviruses and rhinovirus.
• Bacterial:
• Haemophilus influenzae, Streptococcus species, Moraxella catarrhalis and
Staphylococcus aureus.
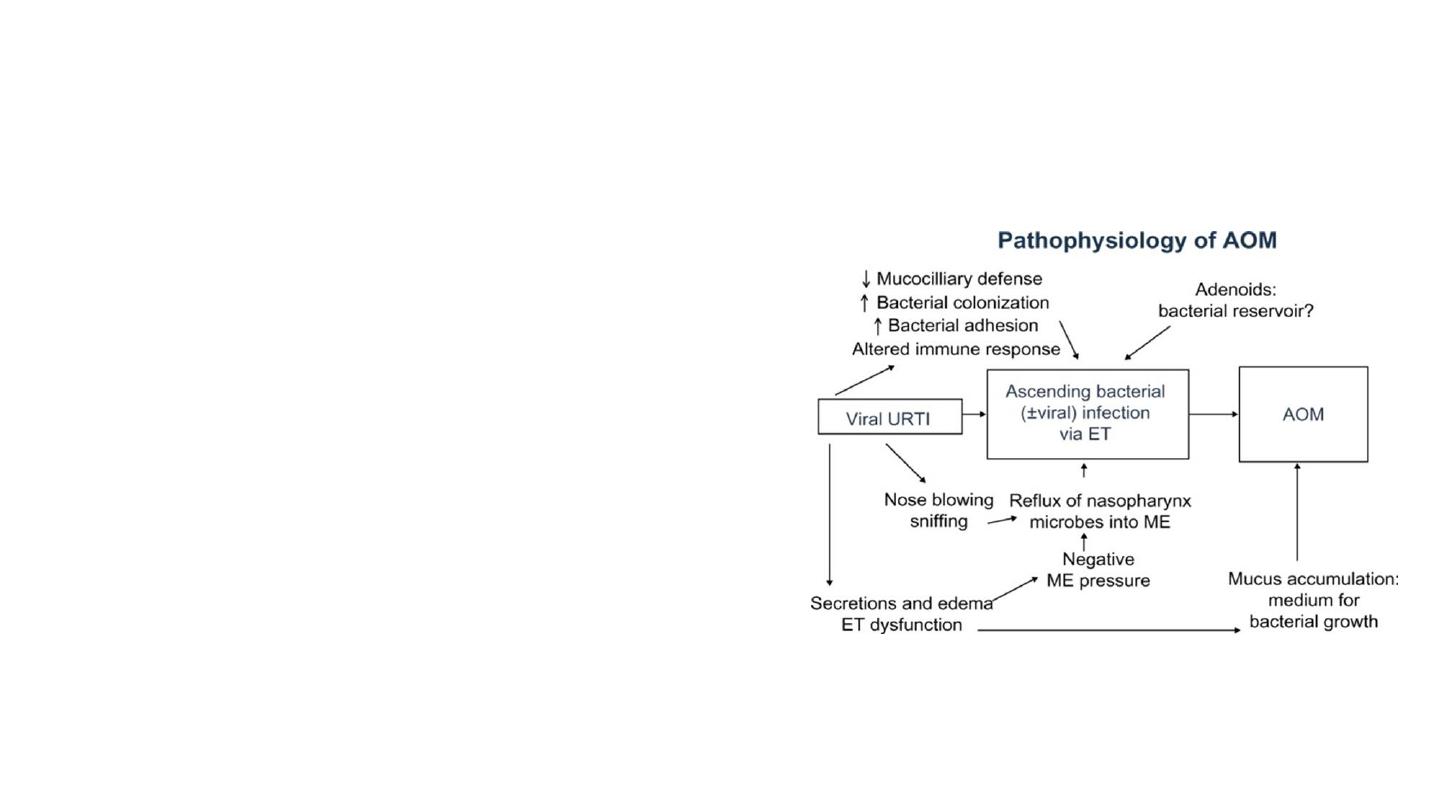
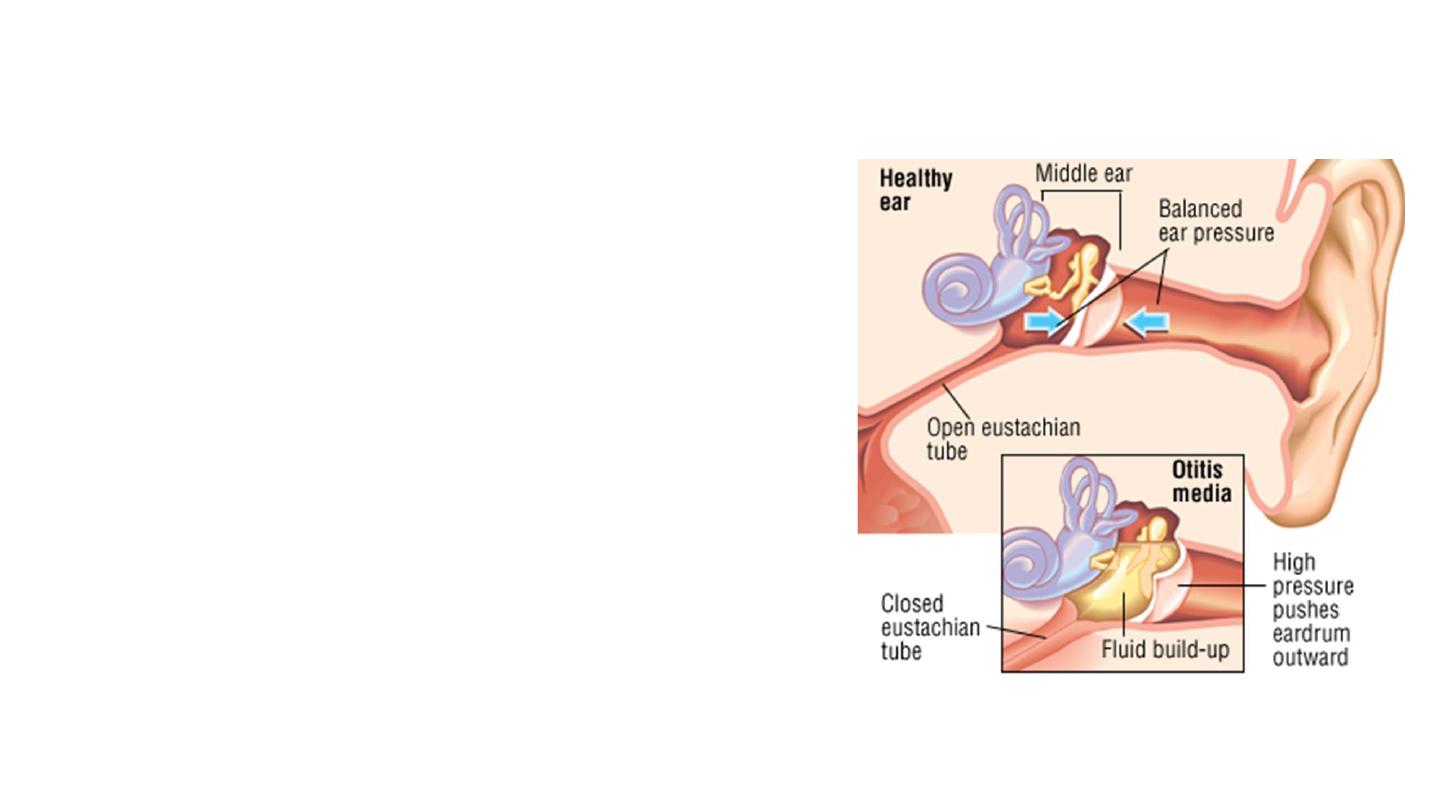
Pathology
• The route of access of pathogens to
the middle ear cleft is variable.
• Direct access may be acquired from
the nasopharynx via the eustachian
tube
• Bloodstream
• From the external auditory canal via a
perforation or ventilation tube

RISK FACTORS FOR ACUTE
OTITIS MEDIA
• Genetic factors
• Racial differences
• low IgG2 subclasses
• Atopy and maternal blood group A
• Environmental factors
• Specific syndromes, particularly those associated with craniofacial
anomalies or skull base abnormalities, e.g Down syndrome
HISTORY AND EXAMINATION
• Symptoms:
• Otalgia
• Hearing loss
• Possible otorrhoea.
• These may follow a preceding upper respiratory tract
infection.
• Fever
• Irritability, poor feeding, vomiting, ear pulling and
clumsiness
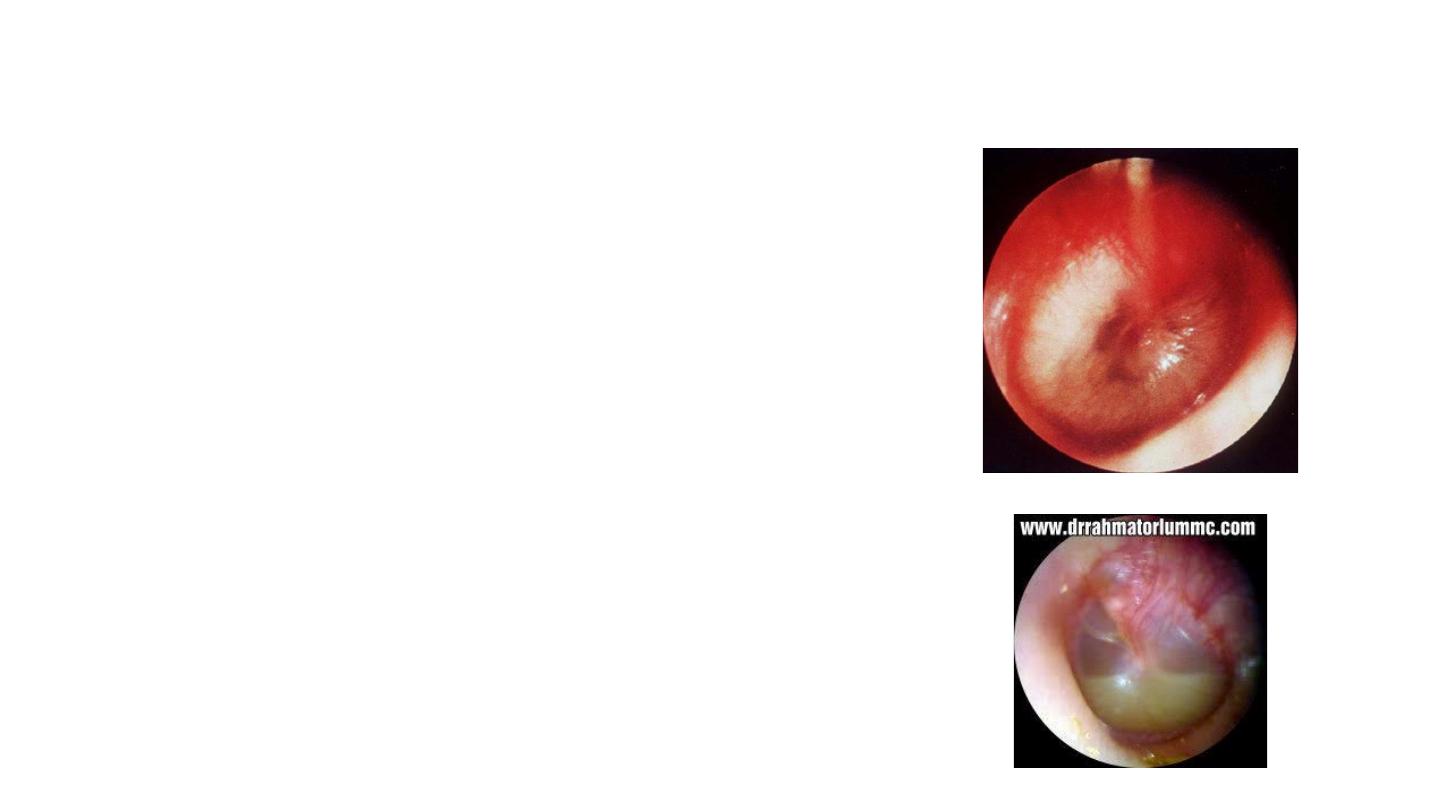
• Otoscopy:
• TM typically appears injected and bulging.
• Yellow TM due to mucopus.
• TM perforation
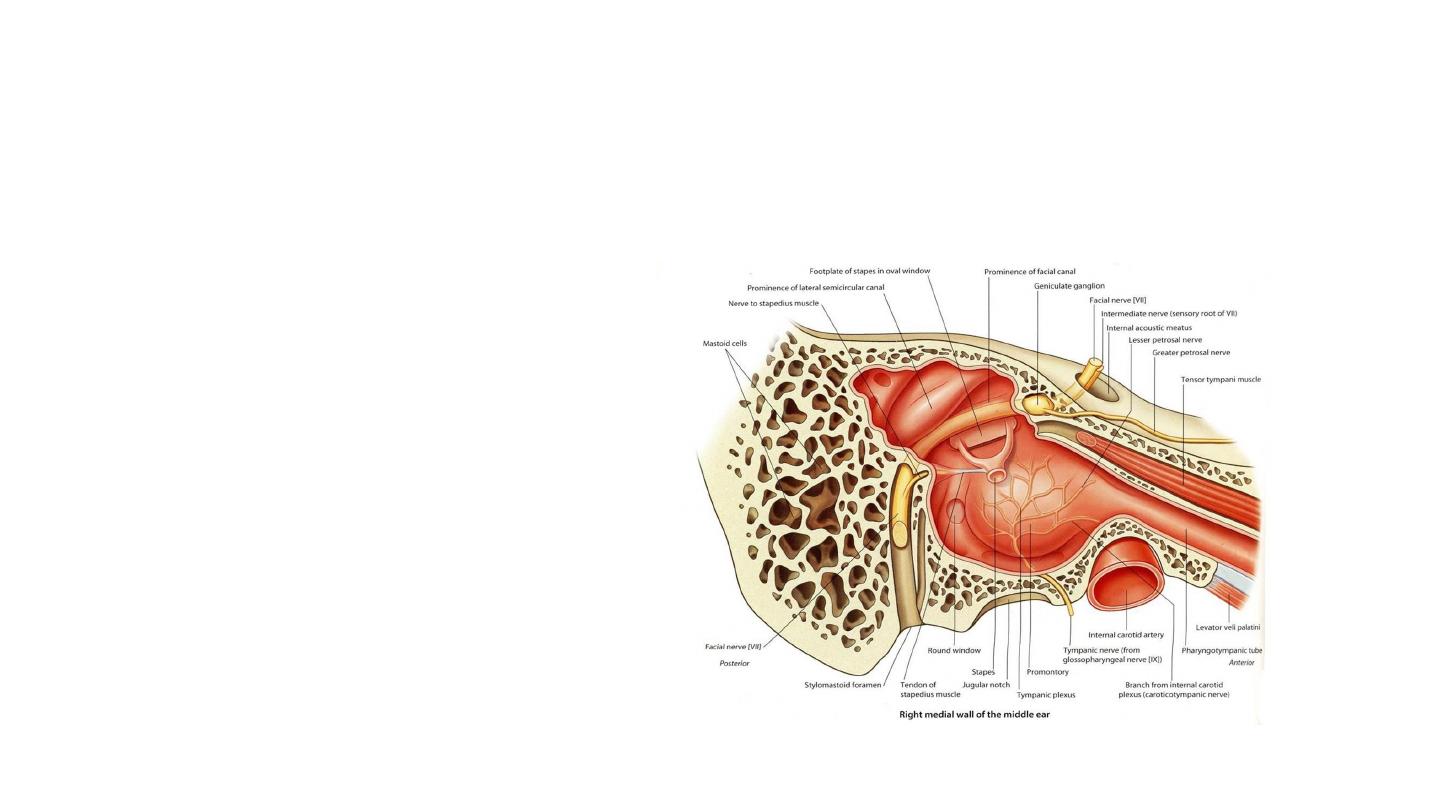
• Intratemporal
• Perforation of the tympanic membrane
• Acute coalescent mastoiditis
• Facial nerve palsy
• Acute labyrinthitis
• Petrositis
• Development of chronic otitis media
• Intracranial
• Meningitis
• Encephalitis
• Brain abscess
• Otitis hydrocephalus
• Subarachnoid abscess
• Subdural abscess
• Sigmoid sinus thrombosis
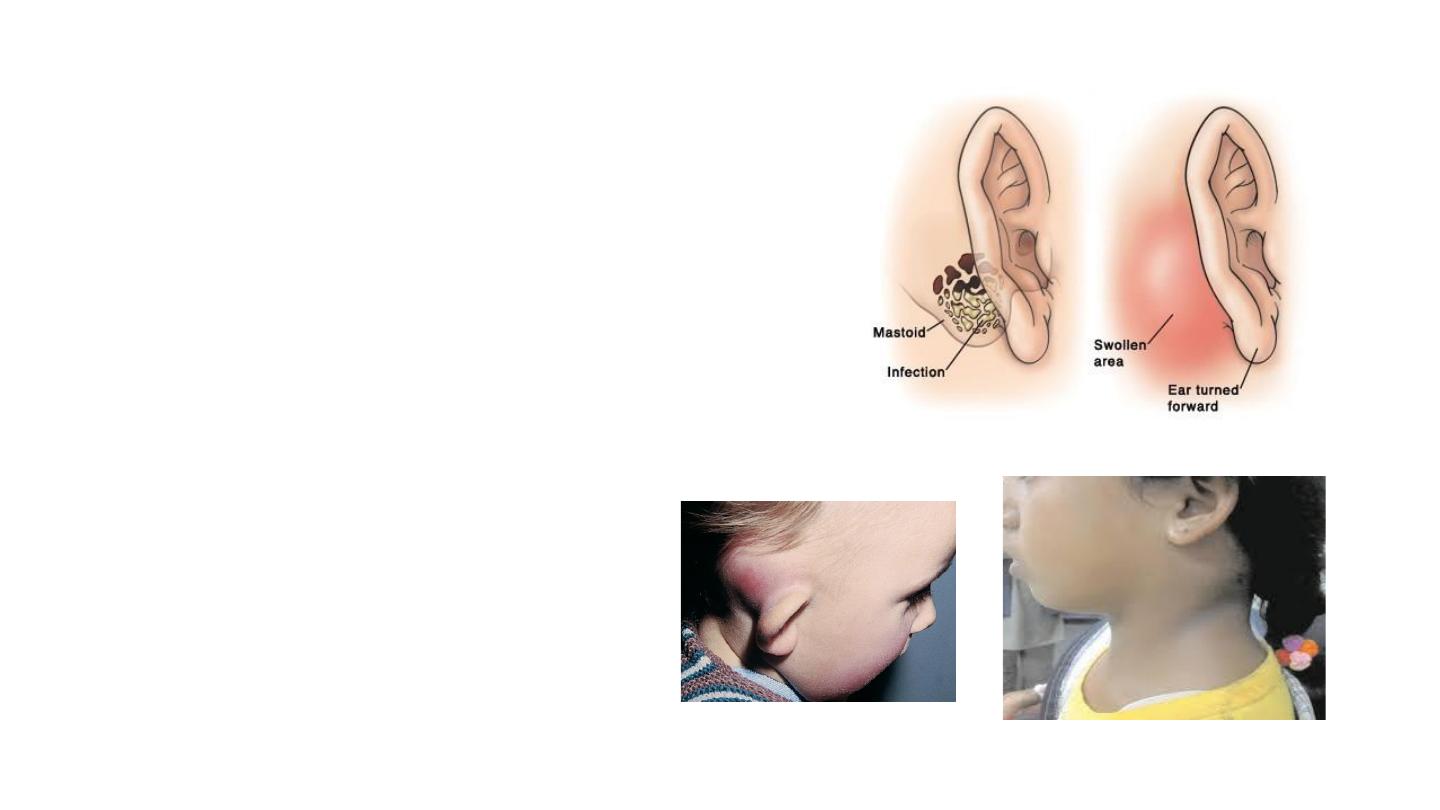
Acute Mastoiditis
• Otalgia, otorrhoea.
• Hearing Loss
• Swelling behind ear
• Malaise.
Examination:
• Pyrexia
• Post auricular swelling
• Pinna-down & forwards
• Full postauricular crease

INVESTIGATIONS
• High-resolution CT scan of the
temporal bones (and neck, if
required) with contrast
• In severe cases or complicated cases
• Suspected complications
• Not responding to antibiotic therapy
• In severe or complicated cases, blood
tests including full blood count,
inflammatory markers (such as CRP)
and blood cultures are indicated.

Treatment
1.
Explanation and advice. This is a condition that is usually self-limiting.
2.
Simple supportive treatment for the inevitable accompanying symptoms including fluids and
simple analgesia such as ibuprofen (anti-inflammatory) and paracetamol (antipyretic).
3.
Antibiotics: 7- to 14-day course of amoxycillin
4.
Spontaneously ruptured tympanic membrane: patients should be encouraged to keep their
ears dry. The majority of such perforations will heal spontaneously within 3 months.
5.
Management of complications: myringotomy+/- grommet insertion, drainage of abscess+/-
mastoid surgery.

Chronic otitis media
• Defined as chronic inflammation of the middle ear cleft including
mucosa, tympanic membrane and ossicles.
• It can be subdivided into non-suppurative and suppurative
• Chronic non-suppurative otitis media (otitis media with effusion)
(glue ear).
• Chronic suppurative otitis media (CSOM)

Otitis media with effusion (OME)
• Presence of fluid or an effusion in the middle ear space caused by
inflammation of the middle ear cleft mucosa
• Symptoms of infection are absent
• No tympanic membrane perforation or otorrhoea.
• The peak incidence is between 2 and 5 years of age with up to 80
per cent of children having had at least one episode by the age of
10
• Mostly encountered in the paediatric population, can occur in
adults.
Aetiology
• Classic Theory
• OME arises from Eustachian tube (ET)
dysfunction
• Inflammation Theory
• This theory suggests that the middle
ear mucosa becomes inflamed from
bacteria already present in the middle
ear or possibly from reflux of saliva
containing URTI viruses or bacteria into
the ET.

• Risk factors:
• Recurrent URTIs
• Parental smoking
• Allergy
• Reduced overall nasopharyngeal dimensions. The adenoids are recognised as
important contributors to OME
• Syndromic risk factors include cleft palate and trisomy 21
Symptoms:
• Conductive hearing loss
• Learning difficulties
• Behavioural problems and speech delay
• Recurrent infections and otalgia are
uncommon
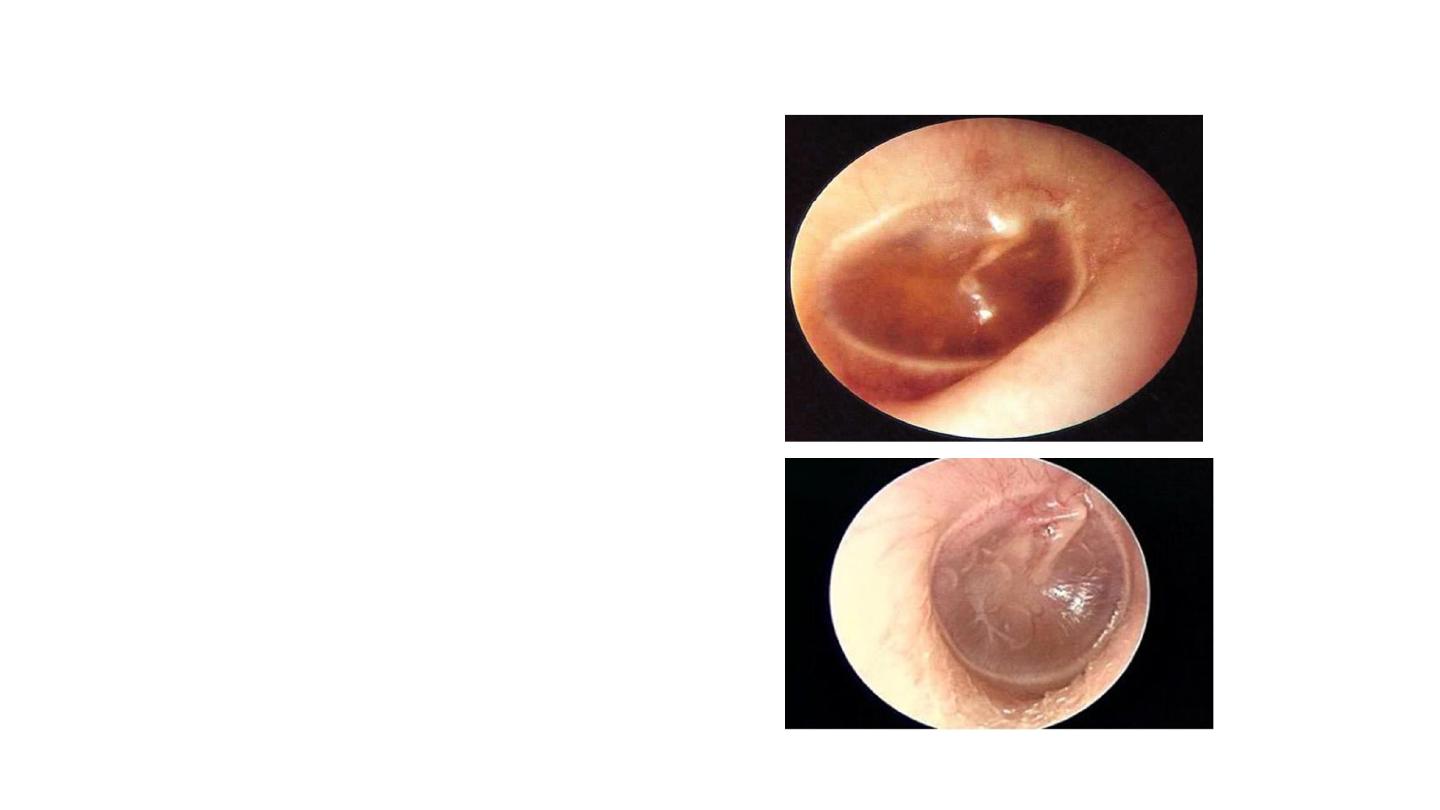
Examination
may or may not reveal a
middle ear effusion.
• The tympanic membrane
• Colour: can look dull red, blue, grey or an
amber yellow colour.
• It can bulge forward or be retracted. Attic
and posterior retraction pockets may occur
• Air bubbles or a fluid level can occasionally
be seen.
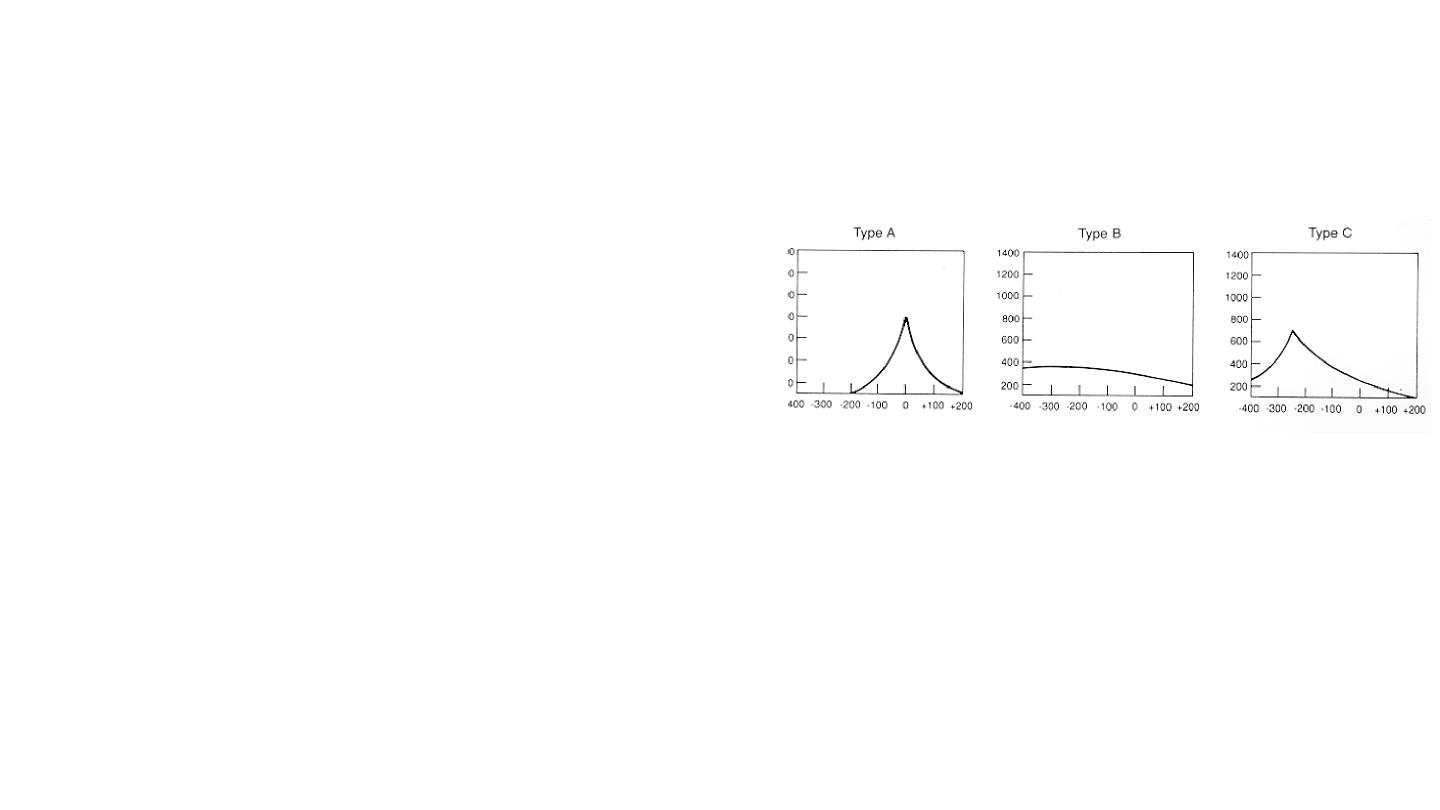
Investigation
• An audiogram appropriate to age
• Will show a conductive hearing loss.
• Impedance audiometry
(tympanometry)
• Will show a flat tympanogram (type B)
• Significant negative pressure peak,
indicating reduced middle ear pressure
Normal
Flat
Negative
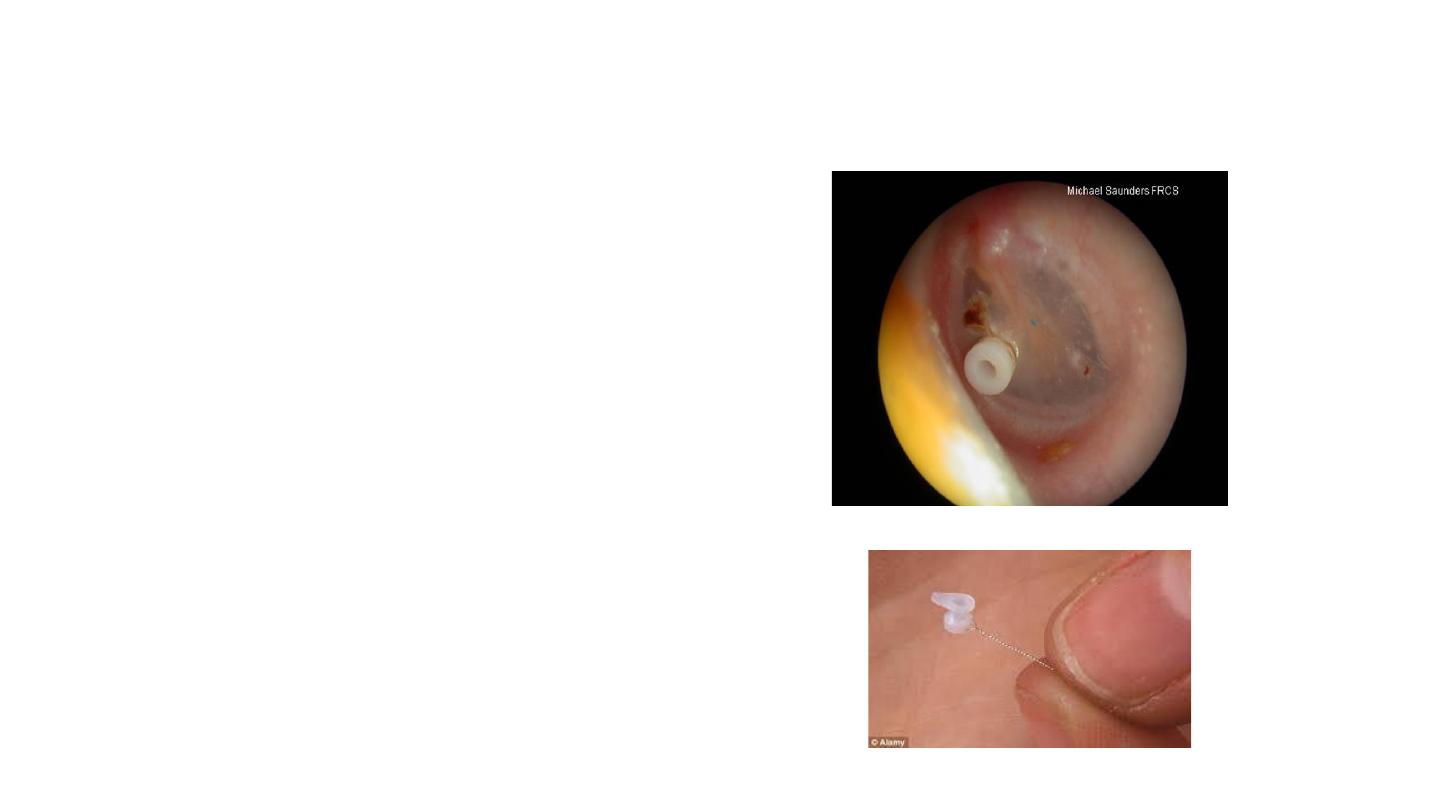
Treatment
• Watchful waiting: first line. Resolve
spontaneously in 3 months
• Myringotomy, suction clearance and
insertion of a ventilating tube
(grommet) +/- adenoidectomy
• Hearing aids are a useful alternative
where surgery is not preferred, or
relatively contraindicated
