PNEUMONIA
Pneumonia is an inflammation of the lung parenchyma ( the lower portion ofrespiratory tract consisting of the respiratory bronchiole ,alveolar ducts ,alveolar sacs
and alveoli ) are is associated with consolidation of the alveolar space .
TYPES OF PNEUMONIA
1 . Infectious pneumonia .
2 . hydrocarbon pneumonia .
3 . aspiration pneumonia .
4 . radiation pneumonia .
5 . lipoid pneumonia .
( pneumonitis is a general term for lung inflammation that may or may not
be associated with consolidation ) .
INFECTIOUS PNEUMONIA
1- VIRAL PNEUMONIA .
A virus is the most common cause of pneumonia in children and the RSV is the most common virus ,others include para influenza .adenovirus ,influenza virus .
Clinical features :-
The picture start with several days of rhinitis and cough followed by fever and more profound respiratory symptoms such as dyspnea and intercostals retraction .
Diagnosis :-
1 . laboratory finding include predominance of lymphocyte on complete blood picture and diffuse bilateral infiltration on CXR .
2 . Specific diagnosis can be done by rapid test for viral Ag and by culturing nasopharyngeal specimens .
Treatment :-
Usually supportive by antipyretic .
Oxygen and fluid sometime needed .
Specific treatment :-
Ribavirin effective for RSV and influenza in sever pneumonia .
Amantidine for influenza type A .
2 - BACTERIAL PNEUMONIA
The common bacterial cause in children older than three months include pneumococ pneumonia and streptococcus group A flowed by sataph .aureas and H influenza .
Clinical features :-
( 1 ) .The clinical features in older children ( about 6 yrs and older) Is fairly classic present first with mild upper respiratory tract symptoms followed by abrupt onset of fever , tachypnea , chest pain and shacking chills .
Physical examination often reveals lateralization chest signs such as decrease breath sound and crepitation on the affected side .
( 2) . younger children < 6 yrs , may present with non specific manifestation including fever ,malaise ,gastrointestinal complaints , restlessness, apprehension and chills .
Respiratory signs may be minimal and include tachypnea cough grunting respiration .
Signs of pneumonia also may be subtle in young infant with absence of crepitation
and rhonchi .
I n older children th finding on examination may consist of decrease or tubular breath
sound .dullness to percusion and egophony in localized region .
Sometime the clinical pictures of pneumonia differ according to causative M. O .
H influenza ytpe b pneumonia often associated with bacteremia , meningitis and other
sites of infections ( arthritis , pleural effusion ,cellulites ).
Staph. Aureas if present in infant ( 70 % of staph .pneumonia in infant present in first year ) ,associated with acute ill infant with empyema ,pneumatoceles and respiratory failure and the infant may have skin lesions , scalp or previous hospitalization and mother with mastitis .
Lower abdominal pain may be associated with lower lobe pneumonia .
Infant betweenone and three months of ages often have afebrile pneumonia with typically is due to congenital or acquired agent such as Chlamydia trachomatis ,CMV,
Or pneumocystis carinii or RSV .
Pneumonia in immunocompromized patient may be due to P.carinii, gram –ve enteric ,Bacteria ,fungi or CMV .
Patient with cystic fibrosis usually due to pseudomonas aeruginosa .
DIAGNOSIS OF PNEUMONIA
Definitive diagnosis of pneumonia require identification of the causative organism . Sputum for culture ( not easily taken for children ) . Chest x-ray often shows lower consolidation and pleural effusion or pneumopyothorax that complete pneumonia .
WBC is elevated with predominance of neutrophil , if M .pneumonia suspected
Cold agglutinin are present in peripheral blood film .
Blood culture is essential for Ag detection
M .tuberculosis may be diagnosed by tuberculin skin test and analysis of sputum or
gastric aspirates .
Invasive procedures such as bronchoscopy and bronchial –alveolar lavage ,lung aspirate , lung pleural aspirate and lung biopsy done in the unusual clinical picture
Or immune compromised host .
Treatment :-
There is no universally accepted antibiotics regimen for treatment of Presumed bacterial pneumonia . The following general guidelines take in consideration :
1.age .
2.severity of illness .
3.presence of illness in the family .
4. previous hospitalization .
5. lab. Studies must be considered when antibiotics is chosen .
( 1) . Children younger than 6 yrs with mild to moderate illness can be observed at home and given oral antibiotics such as amoxicillin ( 50 mg /kg /day ) or Ampicillin ( 100 mg / kg /day ) or erythromycin 50 mg/kg /day ) .
Children with more severe illness required hospitalization and intra venous Cfotaxime ( 100mg/kg /day) ,ceftriaxone ( 50-75mg /kg/day ) or ceftazidime ( 100mg/kg/day ) after that according to culture .If streptococcus pneumonia susceptible the crystalline penicillin is drug of choice .
( 2) . children more than 6 yrs with mild to moderate illness can be observed at home and given oral penicillin or if Mycoplasma pneumonia is likely (macrolides ) can be used such as erythromycin or new generation ( azithromycin and clarythromycin )
In severe cases hospitalization and I V third generation cephalosporin .
Other supportive treatment :
1 .severe dyspnea or cyanosis is indication for oxygen .
2 . antipyretic may be needed .
3. adequate intake of fluid must be ensured .
4. good nursing and the infant position in the cot should be changed frequently and
his head should be raised above his feet .
5 . blood gas analysis in severe ill case should be done .
6 . ventilatory support may be needed in seriously ill child .
7 . Chest physical therapy may be need to clear the secretion and encuorge cough .
Indication of hospitalization in pneumonia
1. failure to response to oral antibiotics .
2. inability to take oral antibiotics because of vomiting or poor compliance .
3. lobar consolidation in more than one lobe .
4. immune suppression .
5. moderate to severe respiratory distress .
6. empyema .
7. abscess or pneumatocele .
8. underling cardiopulmonary diseases.
BRONCHIOLITIS
A common disease of lower respiratory tract of infant results from inflammatory obstruction of small airways .
Respiratory syncytial virus ( RSV ) is the causative agent in more than 50% of cases .others may caused by para-influenza , mycoplasma or adenovirus or measles .
There is no firm evidence that bacteria can cause bronchiolitis .
Bronchiolitis occur most commonly in male infant between 3-6 months ,who have not been breast –fed and who is living in crowded condition and have smoker mother .
The source of viral illness is usually a family member with respiratory illness.
Pathophysiology
Acute bronchiolitis is characterized by bronchiolar obstruction due to edema and accumulation of mucus and cellular debris and by invasion of the smaller bronchial by virus ,and because the radius of airway is smaller during expiration the resultant ball valve respiratory obstruction leads to early air
Trapping and over inflation .
Atelactasis may occur when the obstruction becomes complete and trapped air is Absorbed .
The pathologic process impairs the normal exchange of gasses in the lung.
Ventilation – perfusion mismatched result in early hypoxemia .
CLINICAL MANEFISTATION
T he infant first has a mild upper respiratory tract infection with serous nasal discharge and sneezing , these symptoms usually lasts few days and may be accompanied by diminished appetite and fever of 38 c .
The gradual development of respiratory distress characterized by wheezy cough , dyspnea and irritability .
In mild cases symptoms disappear in 3 days .
In more severe cases may develop within several hours .
On examination :- the patient in distress ( subcostal ,inter costal recession ) . Palpable liver and spleen due to over inflated lung ,wide spread Fine crepitation may be heard .
The expiratory phase of breathing is prolonged and wheezing are Audible .
Chest x-ray finding :-
1 . hyper inflation of the lung and increased antero –posterior diameter .
2 . scattered area of consolidation .
3 . sometimes increased translucency of the lungs
DIFFERNTIAL DIAGNOSIS OF BRONCHIOLITIS :
1 . Bronchial asthma that accompanied by repeated episodes with family history and respond well to bronchodilator .
2 . foreign body usually the history of aspiration and localized sings on Examination.
3 . Bacterial bronchopneumonia that associated with generalized obstructive pulmonary over inflation
4 . heart failure , usually with cardiac murmur .
Admission criteria :
( 1) .any risk factors ( age < 3 months , previous severe bronchiolitis , premature
Apnea , chronic lung disease, congenital heart diseases , Immunodeficiency , multiple congenital abnormalities , Severe neurological diseases ,social concerns ).
( 2) . moderate or severe bronchiolitis .
PROGNOSIS :-
The first three days usually most critical ,after that the improvement occur rapidly and the death may due to :
1. apneic attach .
2. respiratory failure .
3. severe dehydration .
4. associated some cardiac or immunity problems .
A significant proportion of infant have hyper reactive airways during later Childhood .
TREATMENT OF BRONCHIOLITIS
1. Hospitalization of infant with respiratory distress .
2. cool place and humidified oxygen to relieve hypoxemia and reduce water
loss from tachypnea .
3. avoidance of sedation to irritable infant.
4. sitting the infant in 40 degree angle and the head and chest slightly elevated
to extend the neck .
5 . intra venous fluid to replace the loss .
6. ribavirin , antiviral given by aerosol for immune deficient patients or with cardiac diseases .
7 . antibiotics to treat or prevent bacterial invasion .
8 . steroid may be used but sometime may be harmful .
9 . bronchodilators are frequently used .
10 . those patients with impending respiratory failure requiring ventilatory help .
11 . as prevention RSV immune globulin may be given to risky cases .
Discharge if all of the following are confirmed :
1- feeding well . 2- no cyanosis in air . 3- apyrexial . 4- R.R rate < 50 /min.
5- parents are confident .
6. advice parents :-
( a).small frequent feeds .
( b). explain peak symptoms are on day 4-5 .
( c) . open access for 48 hrs to return if they have concerns .
( d) . seek help if worsening and feeding difficulties .
BRONCHIOLITIS OBLITERANCE
Un common form of chronic bronchiolitis in which there is endobronchiolar granulation tissues and peribronchiolar fibrosis , this most commonly caused by adenovirus and less commonly bt measles ,influenza ,pertusis And M . pneumonia .
Most like acute bronchiolitis ,but the course progress often after a period of
improvement with increasing respiratory distress with poor respond to bronchodilator
Treatment :
No specific treatment just supportive with trial with steroid and Bronchodilator .
LUNG ABSCESS .
Lung abscess is a suppurative process resulting in destruction of pulmonary parynchyma and formation of cavity containing purulent material .
Causes :
1 .aspiration of infected material when the local defense mechanismare overwhelmed by surgery or virulent microorganism .
In recumbent position the posterior segments of upper lobes most affected .
In erect position the basilar segments of the lower lobes most affected .
2. pneumonia caused by aerobic pyogenic M.O. like staph.
3 . bronchial obstruction by tumor or foreign body .
4 . metastatic lung abscess secondary to bacteremia or due to septic thrombophlebitis .
5.rare may caused by amebea .
Clinical manifestation :-
Fever , malaise , anorexia ,weight loss , cough often associated With hemoptysis and producing copious amount of foul smelling or purulent sputum .
There may be respiratory distress , spiking fever , chest pain and marked leukocytosis
Diagnosis :-
Chest x-ray shows cavity with or without fluid level surrounded by alveolar infiltration .
Sputum culture reveal mixture of anarobic bacteria .
C.T. scan and u/s used for diagnosis of lung abscess and sometime guiding for aspiration
Treatment of lung abscess :
Treatment should be follow the culture ,but in case of an
aerobic by gram stain , treatment with clindamycin or piperacillin for 4-6 wks and
wait the culture .
Alternative treatment allergic to penicillin is chloramphinicol or metronidazole .
Many consider clidamycin the agent of choice .
Antibiotics should be given intravenous for at least 2-3 wks .
Bronchoscopy is indicated only to identify and remove foreign body .
Chest tube drainage is necessary if empyema present .
Surgical drainage almost never indicated unless :
1 . recurrent hemoptysis .
2 . necrosis .
Asthma
Definition : - asthma is a lung disease characterized by :
1 . Airway obstruction ( or airway narrowing ) that is reversible ( but not completely
So in some patients ) either with treatment or sometime spontaneously
2 . Airway inflammation .
3 . Airway hyper-responsiveness to variety of stimuli .
Incidence :-
Asthma is the most common chronic lung disease of children .
As many as 10 -15 % of boys and 7 – 10 % girls may have asthma at sometime during childhood
1. before puberty twice as many boys are affected , but at puberty the incidence is equal .
2 .asthma is more severe in young children because they are more prone to viral infection and because the smaller airway size increase airway resistance .
3 . data on the inheritance of asthma are most compatible with polygenic or multifactorial .
a child with one affected parent has about 25% risk of having asthma, the risk increases to about 50 % if both parents are asthmatic .
4 . A genetic predisposition combined with environmental factors may explain most cases of
childhood asthma .
Epidemiology :-
Asthma may have its onset at any age . 30 % of patients are symptomatic by one year .
80 – 90 % of asthmatic children have their first symptoms before 4-5 yrs of age ,
Most severely affected children have an onset of wheezing during the first year of life and family history of asthma and other allergic disease, these children may have growth retardation unrelated to steroid therapy .
The prognosis for young asthmatic is generally good .
About 50% of all asthmatic children are virtually free of symptom within 10 -20 yrs , but recurrence are common in children .
In children who have mild asthma with onset between 2 yrs and puberty , The remission rate is about 50% and only 5% experience severe asthma .
In contrast ,resolution is rare in children with severe asthma characterized By chronic steroid user with frequent hospitalization about 95 % become Asthmatic adult .
Risk factors for occurrence of asthma include :-
( poverty , black race , birth weight less than 2.5 kg , maternal smoking . Small home size , large family size , intense allergic exposure at infancy )
ETIOLOGY :-
Asthma is a complex disorder involving autonomic , immunogenic , Infectious , endocrine and psychological factors .
Vagal sensory ending in airway epithelium causing contraction of smooth muscles .
Immunological factors as extrinsic ( allergic asthma ) have increase IgE level .
Intrinsic asthma no increasing IgE level and negative skin test .
Viral agent are the most important infection triggers .
Endocrine effect on asthma may be worsen in relation to pregnancy and menses .
Thyrotoxicosis increase the severity of asthma .
Psychological factors affection are related more closely to poor control of asthma Than to the severity of asthma .
Summary of asthma triggers in children :
1 . respiratory infections .
2 . irritant ( cigarette , air pollution .
3 . exercise .
4 . allergic ( inhaled or ingested )
5 . change in the weather .
6 . emotional stress ( cry . laugh ) .
7 . medication like aspirin .
8 . gasroesophageal reflux .
ASTHMA PATHOPHYSIOLOGY :
The pathology of asthma include bronchoconstriction , bronchial smooth muscle
hypertrophy , mucous gland hypertrophy , mucosal edema , infiltration of
inflammatory cells ( eosinopil , neutrophil , basophil , macrophage ) .
Obstruction is most severe during expiration because the intrathoracic airway become
smaller during expiration .
Overinflation cause decrease compliance and then increase work of breathing .Airway obstruction may lead to atelactasis and then ventilation – perfusion mismatch
Further narrowing of airway may lead to pheumothorax .
Hypoxia may damage alveolar cells and then decrease surfactant which normally
stabilized alveoli , thus this process may aggravate the tendency toward atelactasis .
CLINICAL FEATURES
The acute episodes are most often caused by exposure to irritant such as cold air or exposure to allergins .
Because airway patency decrease at night many children have acute asthma at night .
Cough is non productive early in the course of attack accompanied by wheezing ,
Tachypnea , dyspnea , prolonged expiration and use of accessory muscles of
Respiration .
Hyperinflation of the chest , tachycardia and pulsus paradoxus may be present in
severe asthma .
Cough may present without wheezing or wheezing may be present without cough .
Asthma may present only with chronic night cough only .
When the patient is in extreme respiratory distress the cardinal signs ,wheezing may
be strikingly absent only after bronchodilator treatment gives partial relief of the
airway .
Abdominal pain is common due to contraction of abdominal muscles and diaphragm ,
Vomiting is common .
DIFFERENTIAL DIAGNOSIS :
1 . Respiratory ( infection , foreign body aspiration , tracheomalacia , cystic fibrosis ,
Bronchiectasis , alpha 1 – anti trypsin deficiency ) .
2 . cardiac ( congenital heart disease with failure , vascular ring ) .
3 . G.I.T ( gastro- esophageal reflux , H type fistula ) .
4 . Miscellaneous ( immune deficiency , psychogenic cough ) .
LABORATORY STUDIES IN ASTHMA
1 . Complete blood count , generally normal but esonophelia suggest atopy .
2 . sputum whitish with esonophilia and purulent sputum suggest infection .
3 . chest x-ray normal between episodes
Hyperinflation , atelactasis , pneumomediastinum or presence of pneumothorax .
May be present .
4 . pulmonary function test .
5 . serum IgE
6 . Allergy skin test .
7 . arterial blood gas analysis .
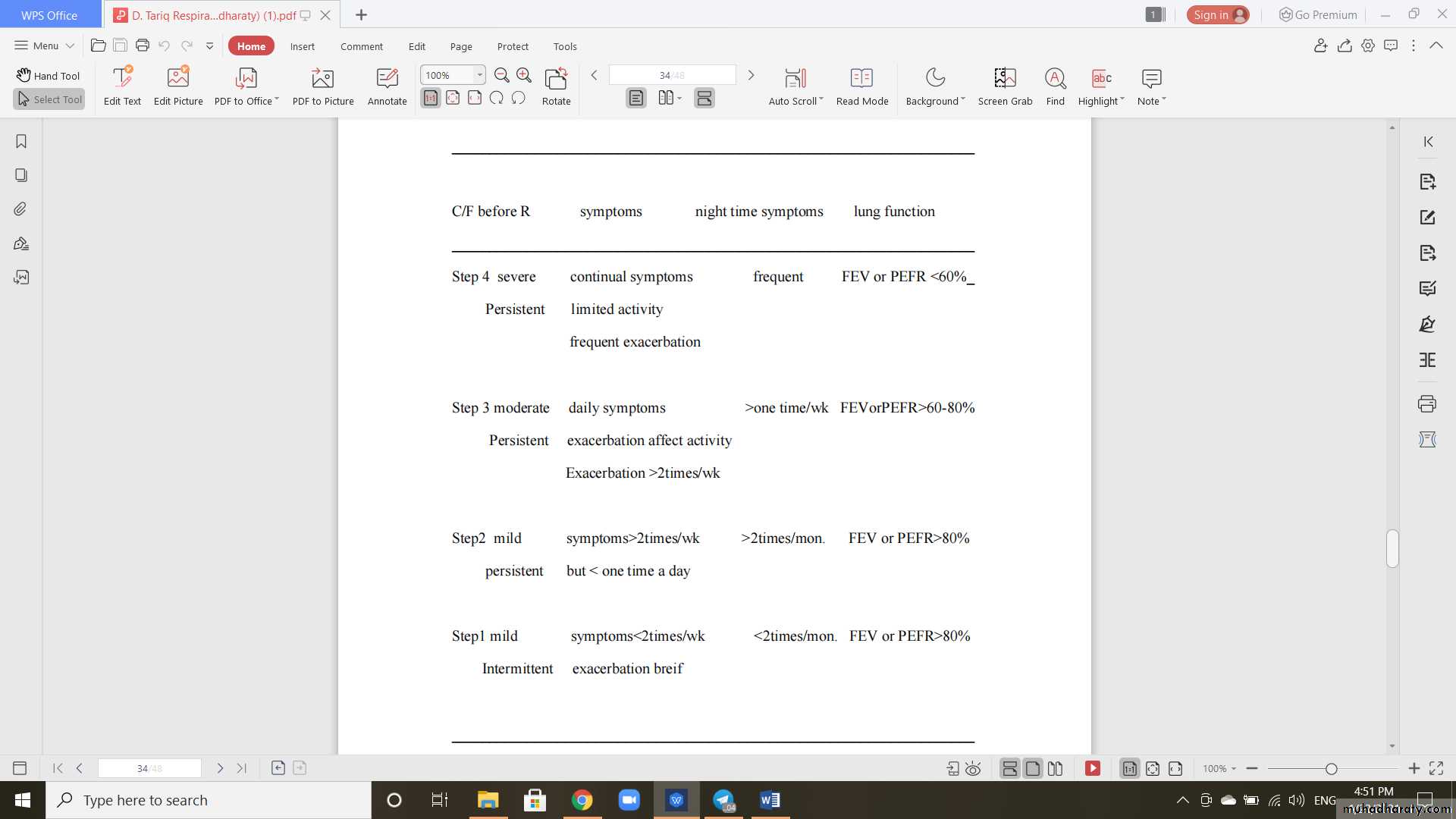
CLASSIFICATION OF ASTHMA SEVERITY IN GENERAL
_____________________________________________________________________
_____________________________________________________________________
FEV =Forced expiratory volume in 1st secondPEFR = Peaked expiratory flow rate
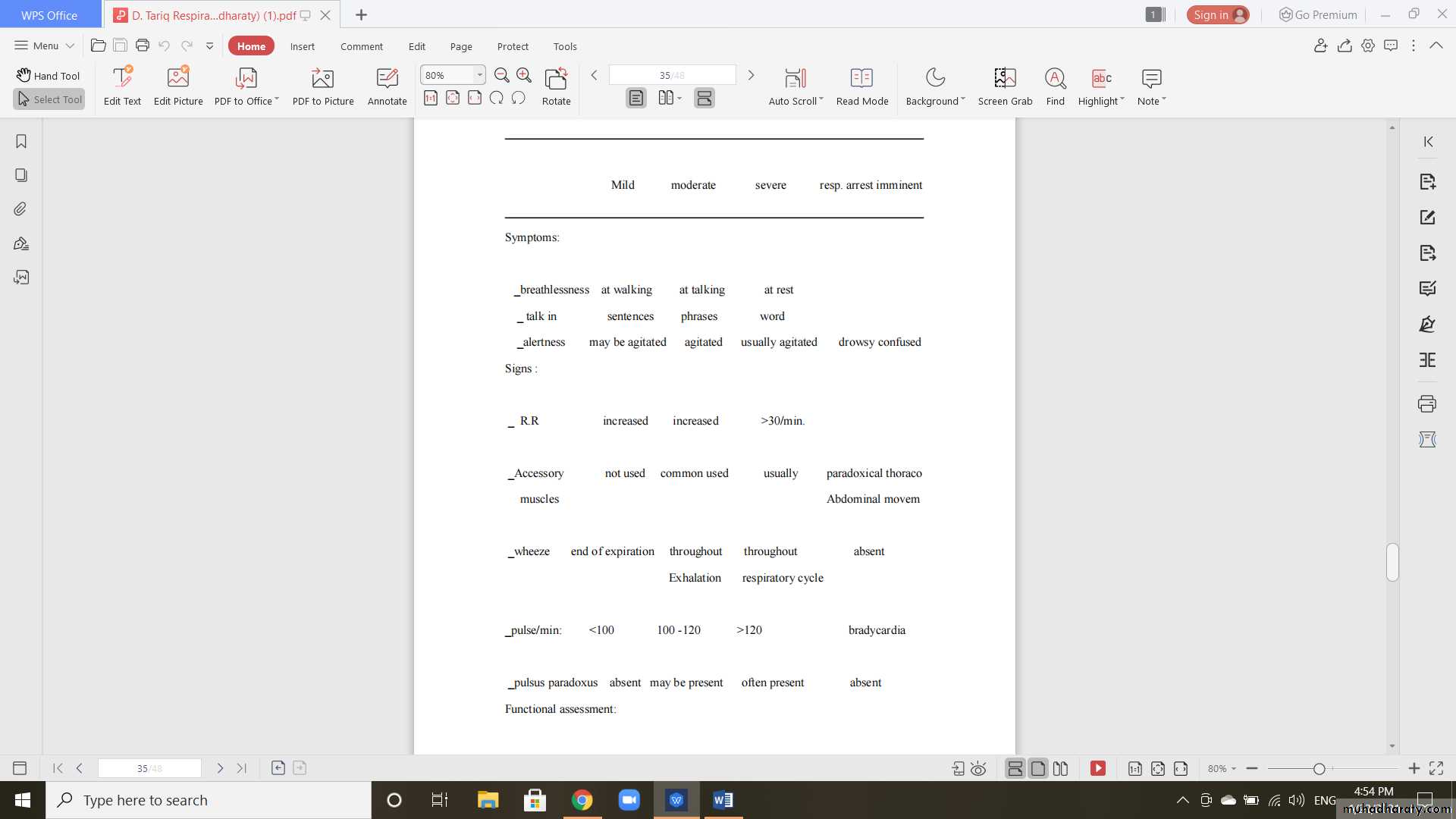
_SaO2 CLASSIFICATION OF SEVERITY OF ACUTE ASTHMA EXACERBATION
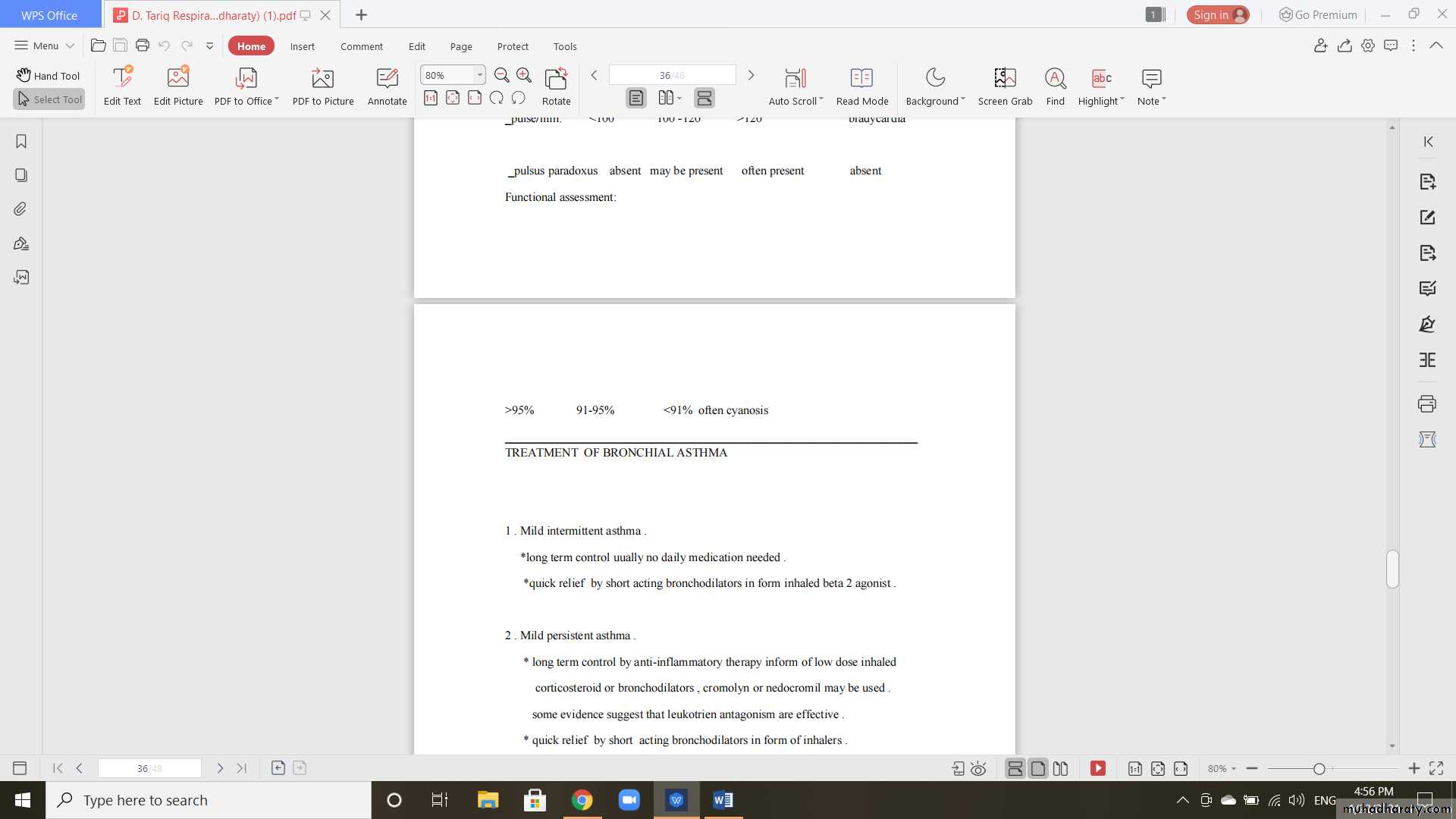
_____________________________________________________________________TREATMENT OF BRONCHIAL ASTHMA
1 . Mild intermittent asthma .*long term control uually no daily medication needed .
*quick relief by short acting bronchodilators in form inhaled beta 2 agonist .
2 . Mild persistent asthma .
* long term control by anti-inflammatory therapy inform of low dose inhaled corticosteroid or bronchodilators , cromolyn or nedocromil may be used . some evidence suggest that leukotrien antagonism are effective .
* quick relief by short acting bronchodilators in form of inhalers .
3 . Moderate persistent asthma .
* long term control by daily anti –inflammatory treatment inform of inhaled corticosteroid and long acting bronchodilators .
*quick relief by short acting bronchodilators .
4 . Severe persistent asthma .
* long term control daily anti-inflammatory therapy inform of inhaled corticosteroid ( high dose )and long acting bronchodilators , anti-leukotien or theophyline .
* quick relief by short acting bronchodilators .
Treatment of severe asthma ( status asthmaticus )
1 . Admission and continuous oxygen to keep saturation more than 90 % .
2 . Aerosilized albuterol ( salbutamol ) in a dose 0.15 mg /kg may be repeated hourly
3 . Methyl prednisolone 1-2 mg/kg intravenously 6 hourly or Hydrocortisone 10 mg /kg
4 . Aminophyline administral either loading dose 5 mg /kg followed by continuous infusion or bolus therapy 1mg /kg 6 hourly ( slow infusion ) .
Beside that laboratory work should include blood gas analysis and electrolytes .
Chest x-ray is advisable if there are localized abnormalities on auscultation or
failure response to the treatment .
Fluid therapy may be needed due to loss that result from ( hyper ventilation , poor
oral intake , diuretic effect of theophyline ) .
Mechanical ventilation may be needed if medical therapy failed .
DRUGS USED IN ASTHMA
1 .Bronchodilators :-
A . B2-adrenergic agonist include albuterol ( sabutamol ) , terbutaline , epinephrine and isoproterenol .
for example albuterol ( o.1-0.15 mg/kg / dose ) 3 times daily orally .
aerosol ( 0.o1-0.03 ml/kg ) diluted with 2 ml of normal
saline up to 4 times daily .
side effects tachycardia , tremor .
B . Xanthine ( theophyline and its derivatives ) are effective bronchodilators but have significant side effect like irritability , hyperactivity , hematemesis and seizure this can be minimized by beginning with small dose and increase slowly and available as rapid release and slow release .
C . Anticholinergic such as ipratropium bromide as atropine derivative ,
have slower onset of action and provide less maximal bronchodilation .
2 . Corticosteroid :-
They have significant side effect when used orally for long period
Oral preparation are extremely effective , however low dose therapy Usually 3-5 days .
Low dose ( alternative day ) steroid therapy can be used effectively
for patient whose asthma can not be controlled with inhaled steroid
because o high effective and can be used safely for chronic asthma .
Mode of action of steroid :
1 . suppression of mediators .
2 . enhance response to agents that increase cyclic AMP .
3 . Enhance response to B2 agonist .
3 . Cromolyn :- Is a mast cell stabilizers that inhibit pulmonary histamine release .
It given to prevent ( not treat ) asthma .
4 . nedocromil :- Is effective in long term asthma ( 4 mg by inhalation ) but has no clear
cut advantage over cromolyn .
5 . Leukotriene inhibitors :- These agent improve pulmonary function by afford protection
against bronchospasim induced by exercise cold air and allergens.
Zafirlukast and Zileutin given above 12 yrs .
Montelukast can be given in children above 2 yrs .
6 . Ketotifen :- Antihistamine with mass cell stabilizers used for prevention .
7 . Methotrexate :-
Remain as experimental therapy for patient with severe steroid
dependent asthma .
8 . Future therapy :-
Monoclonal Anti IgE antibodies are undergoing clinical trial in
patients with allergen induced asthma
EDUCATION ABOUT ASTHMA
1 . Patients should be aware about the triggering factors to be avoided .
2 . patients and parents should know how to use medication .
3 . parents should understand that asthma is chronic disorder with acute exacerbation .
4 . emphasize the importance of compliance and adherence to treatment .
5 . avoid unnecessary restriction in the life style of the child or family .
INHERITED LUNG DISEASES
CYSTIC FIBROSIS :-
The most common lethal inherited disease of whitish that defined as a disease of the exocrine gland that cause viscoid secretion ,the GIT , and pulmonary system are most commonly and most severely affected .
Pathogenesis :-
Cystic fibrosis is inherited as autosomal recessive gene that located on
chromosome no. 7 .
The defect in cystic fibrosis is thought to be blocked or closed chloride channel in the
cell membrane of epithelial cells . this blockage traps chloride ions inside the cell and
draws ions and water into the cell . this process results in dehydration of the mucous
secretion .
Clinical features :-
1 . respiratory insufficiency , occurs eventually in more than 95 % of all patients and caused by abnormal mucous gland secretion in the airway producing airway obstruction and secondary infection , cough , dyspnea , bronchiectasis , pneumothorax and finely corpulmonale is a late complication .
1. GIT , chronic diarrhea and malabsorption .
2. electrolytes in sweats ( sodium and chloride is high ) .
3. reproductive defect including sterile male and reduce fertility in females .
4. hepatic manifestation , that ends with portal hypertension .5. pancreatic with diabetic mellitus .
6. skeletal abnormalities with arthritis and joint pain .
7. nasal including chronic sinusitis with nasal polyps .
Diagnostic criteria of cystic fibrosis :-
1 . positive sweat test by skin test > 6 MEq /L .
2 . typical pulmonary manifestation .
3 . typical GIT manifestation ( meconium ileus , chronic diarrhea , rectal prolapse ,
billiary cirrhosis ) .
4 . positive family history .
Therapy :-
1 . treatment of pulmonary problems .
2 . chest physiotherapy ( postural drainage , active cycle of breathing ) .
3 . antibiotics given orally , I.v or aerosol especially for staph. And pseudomonas infection ( aminoglycosides , cephalosporin can be used ) .
4 . bronchodilators and steroid .
5 . pancreatic enzymes replacement .
6 . vitamins supplement , high calorie and protein diet .
7 . treatment of complication accordingly .
8 . lung transplant .
DISEASES OF PLEURA
PLEURAL EFFUSION :--
Accumulation of fluid in the pleural space whenever the local hydrostatic forces pushing fluid out of the vascular space exceed osmotic forces pulling fluid back into the vascular space .
Etiology :-
1 . congestive heart failure .
2 . hypoprotienemia .
3 . obstruction of lymphatic drainage .
4 . malignancy .
5 . collagen vascular disease .
6 . infection of pleura is due to strepto cocus , pneumonaie , H . influenza or T .B .
Clinical features :-
In general clinical features of primary disease is the presenting symptoms , but the patient may complain from pain , dyspnea , and sings of respiratory insufficiency resulting from compression of the underling lung tissues .
Physical finding include :-
Dullness to percussion , decrease breath sounds , mediastinal shift and decrease tactile fremitus .
Diagnosis :-
Is confirmed by chest x-ray . postero- anterior shows uniform opacity with a curved upper border , when air is also present the fluid line is horizontal . decubitus views may be helpful to distinguish fluid collection from other densities in the thorax .
diagnostic thoracocetesis may be necessary to establish the cause of the effusion and
to exclude infection .
Most patients with effusion should undergo diagnostic thoracocentesis unless the:-
1 . underling causes for the effusion are clearly evident .
2 . the patient does not have significant respiratory distress .
3 . infection not suspected .
Comparison between transudates and exudates pleural effusion :
Transudate exudates
--------------- ------------
1 . low specific gravity < 1.015 high specific gravity
2 . low protein ( < 2.5 g/ dl high protein > 3g / dl
3 . decrease lactic dehydrogenase increase lactic deh.
4 . low cell count high cell count
5 . high PH low PH
6 . normal glucose low glucose
Treatment : -
Treatment directed to the underlying condition that cause the effusion and at relief of mechanical consequences of the fluid collection .Small effusion especially if they are trnsudate usually require no treatment .
Large effusion may require drainage with chest tube especially if the fluid is
purulent ( empyema ) .
If the underlying condition is treated successfully the prognosis for patient with pleural effusion including empyema is excellent .
PNEUMOTHORAX:-
Is the accumulation of air in the pleural space that may result from external trauma or from leakage of air from the lung or air way ,it may occur spontaneously .Predisposing condition include :-1 . mechanical ventilation .
2 . asthma .
3 . disorder of collagen .
4 . cystic fibrosis .
5 . infection especially staph. Pneumonia , T.B.
6 . Iatrogenic ( tracheostomy , thorachocentesis ) .
Symptoms of pneumothorax :-
Chest pain , dyspnea , and cyanosis . If the air leak accumulate with mediastinum , subcutaneous emphysema may become apparent .
Physical finding :-
Decreased breath sounds , tympanic percussion note , sings of mediastinal shift and subcutaneous crepitance .
Few or no physical sings of pneumothorax may be present if the amount of air collection is small , but symptoms may progress rapidly if the air in the pleural space is under pressure ( tension pneumothorax ) with death resulting if the tension not relieved .
DIAGNOSIS :-
The radiography usually confirms the diagnosis ,although in the infant there may be difficulty in distinguishing pneumothorax from a large diaphragmatic hernia or giant emphysematous bulla , drink of gastrografin usually resolve the difficulty .
TREATMENT OF PNEUMOTHORAX :-
The treatment depend on the amount of air collectedand the nature of the underling cause ,
Small pneumothorax often do not need treatment and resolve spontaneously .
Large pneumothrax and tension peumothorax require immediate drainage of air .
In emergency situation a simple needle aspiration may sufficient , but placement of
chest tube may be require for resolution .
Sclerosing the pleural surfaces to obliterate the pleural space may benefit patient with
recurrent pneumothoraces .