
Allergic conjunctivitis
1- Allergic rhinoconjunctivitis (acute allergic conjunctivitis):
- The most common type of eye allergy.
- It is a hypersensitivity reaction (type I) to a specific airborne antigens.
- Usually there is associating nasal symptoms (so it is called
rhinoconjunctivits) that is thought to be a result of one or more of the
following fact:
a- Direct effect of the allergen on the nasal mucosa and conjunctiva.
b- We have nasolacrimal drainage, so the excessive tears produced are
drained to the nose.
c- As both of them (the conjunctiva and nasal mucosa) are supplied by
pterygopalatine ganglia, so the stimulation of one of them will leads to
stimulation of the other.
- There are two types:
a- Seasonal allergic rhinoconjunctivitis:
- Acute onset of "hay fever" symptoms.
- The most common allergens are pollens.
- Usually occurs during summer.
b- Perennial allergic rhinoconjunctivitis:
- less severe and less prevalent than seasonal allergic rhinoconjunctivitis
(SARC).
- Usual allergens are house-dust mites or animal dander.
- Symptoms occurs throughout the year.
Presentation:
Acute, transient attacks of slightly red, itchy and watery eyes associated with
sneezing and a water nasal discharge.
Signs:
- Mild to moderate lids oedema (as there is inflammation of the palpebral part
of conjunctiva that liberates mediators that cause collection of fluids).
- Periorbital oedema in severe cases.
- Milky or pinkish appearance of conjunctiva as a result of oedema and
injection.
- Mild papillary reaction in the upper tarsal conjunctiva.
Treatment:
Either topical mast cell stabilizer e.g. nedocromil & lodoxamide, or topical
antihistamine e.g. levocabastine & azelastine.
* Only in very rare and severe cases we need topical steroids.
2- Vernal keratoconjunctivitis (spring catarrh):
11
- It is a recurrent, bilateral, external, ocular inflammation affecting children
and young adults.
- More common in male than females.
- Vernal keratoconjunctivitis is an allergic disorder in which IgE and cell-
mediated immune mechanisms play an important role (hypersensitivity
reactions type I & IV).
- Atopic patients often develop asthma and eczema in infancy.
- The onset of vernal keratoconjunctivitis is usually after the age of 5 years (5-
8y) and the condition eventually resolves around puberty, only rarely
persisting beyond the age of 25 years.
- As its name suggests (seasonal basis), the peak incidence of symptoms occur
between April and August but many patients have year-round disease.
- The condition is more common in warm, dry climate and less frequently in
colder climates.
Clinical features:
The main symptoms are:
- Intense ocular itching.
- Lacrimation.
- Photophobia.
- Foreign body sensation.
- Burning.
- Thick mucus discharge.
- Ptosis also occurs (it is a mechanical ptosis as it occurs due to chronic
inflammation and oedema that causes heaviness and increased weight of the
eyelid).
There are three main types (according to anatomical distribution of vernal
disease):
a- Palpebral, b- Limbal and c- mixed.
Signs:
For conjunctivitis:
* For palpebral vernal keratoconjunctivitis, signs in chronological order:
- Conjunctivitis hyperaemia.
- Diffuse papillary hypertrophy mostly on the superior tarsus (tarsal
conjunctiva).
- Enlarged of papillae ends in flat-topped polygonal appearance
(cobblestones).
* For limbal vernal keratoconjunctivitis:
- It is characterized by mucoid nodules that have a
smooth round surface.
22
- Discrete white superficial spots (Trantas dots); which are composed of
collections of inflammatory predominantly eosinophils, are found scattered
around the limbus.
* For mixed vernal keratoconjunctivitis:
- There is papillary reactions and Trantas dots.
For keratitis:
- Punctate keratopathy (epithelial erosions, micro erosions), it is the earliest
finding.
- Macro erosions (result of continued epithelial loss, i.e. small ulcers).
- Plaque (macro erosions coated by layers of mucus which cannot be wetted by
tears and resists epithelization).
- Subepithelial scarring (sign of previous severe corneal involvement), it
occurs due persistent inflammation that prevents healing).
- Pseudogerontoxon, which resembles as arcus senilis. It is seen in the outline
of previously inflamed limbus (occurs if the epithelial scarring and
opacification are in periphery the limbus).
Treatment:
1- Topical steroids: (its use is mandatory)
- As the patients will not heal by any drug, so we use weak steroids as
fluorometholone rather than dexamethasone, betamethasone or prednisolone
as weak ones are of less penetration to cause increase in IOP or to cause
cataract as the strong steroids.
- Short course.
- Potent steroid, long course causes increase in intraocular pressure and
cataract, so the patient get blind due to use of topical steroids, especially seen
in those jumping from one doctor to another as no one can cure them.
2- Mast cell stabilizers:
nedocromil 0.1% drops *2 daily
or lodoxomide 0.1% drops *4 daily.
or sodium cromoglycate 2% *4 daily
They are not effective as steroids in controlling acute exacerbation (as their
actions starts when all mediators released are used, so their action delays for
few days).
3- Acetylcyseine 5% drops *4 daily, as treatment of early plaque formation
(mucolytic).
4- Topical cyclosporin A: used in steroids resistant cases.
5- Debridement: of early mucus plaques
6- Supratarsal injection of steroids: it is very effective in patients with severe
disease unresponsive to conventional therapy.
Conjunctivitis in mucocutaneous diseases
33
(Autoimmune conjunctivitis)
1- Cicatricial pemphigoid:
- It is a rare, idiopathic, chronic, progressive, autoimmune, mucocutaneous
disorder that primarily affects elderly patients, and it affects females more than
males.
- About 90% of patients have lesions of the oral mucosa but skin lesions are
less common.
Presentation:
- Subacute onset of non-specific symptoms such as:
Irritation, burning and tearing, so the diagnosis may be easily overlooked
(missed).
Signs: in chronological order:
a- Papillary conjunctivitis plus diffuse conjunctival hyperaemia.
b- Subconjunctival bullae that ends with ulceration and pseudomembranes.
c- Later changes: chronic inflammation, subepithelial fibrosis and conjunctival
shrinkage.
complications:
a- Dry eye: due to:
- Fibrous occlusion of ductules of the lacrimal and accessory lacrimal glands.
- Destruction of the goblet cells.
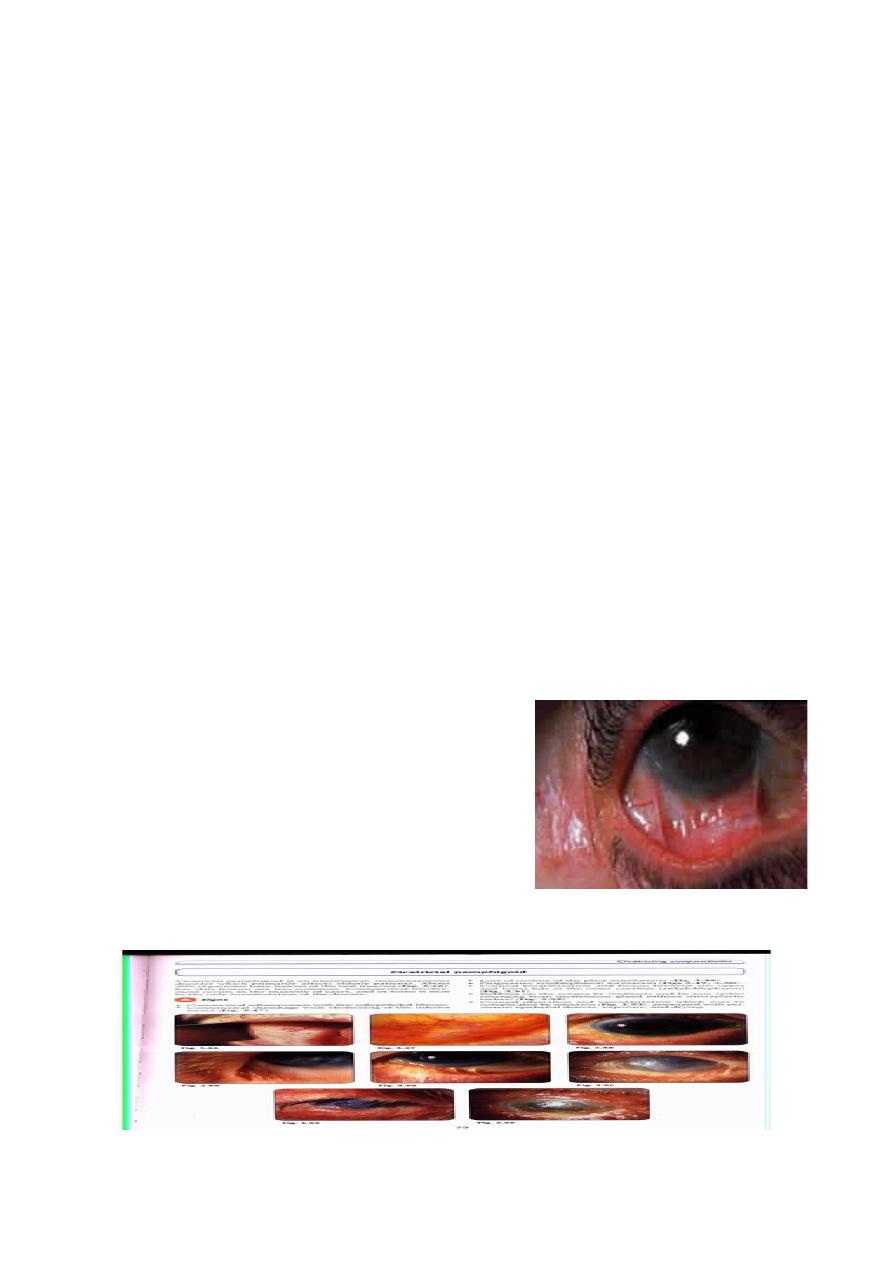
b- Symblepharon: Adhesions between bulbar
and palpebral conjunctivae.
c- Ankyloblepharon: Adhesions between upper
and lower eyelids at the outer canthi.
d-
Keratopathy: (sight-threatening) caused by:
Symblepharon formation demonstrated by
drawing lower lid down and having the
patient look up.
â
Progressive symblepharon formation
Ankyloblepharon
44

- Cicatricial entropion.
- Metaplastic lashes (the lashes emerge from the orifices of meibomian
glands).
- Lagophthalmos (partial or total inability to close the lids).
- Dry eyes.
e- End stage disease:
- Total keratinization of the cornea.
- Obliteration of fornices.
- Corneal neovascularization.
- Corneal ulceration.
- Secondary bacterial infection.
Treatment of cicatricial pemphigoid:
a- Topical therapy:
- Steroids in acute stage.
- Artificial tears.
- Antibiotics (protection from bacterial infection).
b- Systemic therapy:
- Steroids are used in acute manifestation.
- Long term therapy, we use dapsone and cytotoxic agents (azathioprine,
cyclophosphamide) to suppress conjunctival inflammation.
c- Silicon contact lenses:
- To protect cornea from trichiasis and drying.
- Holding tear film.
d- Surgery: (Not done in acute stage, as it may accelerate incidence of
infections)
- Correction of entropion.
- Punctual occlusion if not already occluded, to prevent tear drainage by
nasolacrimal duct.
- Tarsorrhaphy (suturing of both lids) or injection of botulinum toxin into
levator muscle.
2- Stevens-Johnson syndrome:
(compare between this item and the previous
one)
It is an acute, self-limiting, severe, mucocutaneous vesiculobullous disease,
which primarily occurs in young healthy individuals, and males are affected
more often than females.
Precipitating factors: are hypersensitivity reactions to:
a- Drugs.
b- Infectious e.g. Mycoplasma pneumoniae, Herpes simplex virus.
A cause is found in only 50% of cases.
Basic lesion:
55
It is an acute vasculitis, which affects the skin in 100% and the conjunctiva in
90%.
Presentation:
Fever, malaise, sore throat, cough and arthralgia.
Ocular signs:
a- The eyelids are swollen and crusted.
b- conjunctivitis of different grades varies in severity as follows:
i- Transient mild papillary conjunctivitis.
ii- Severe membranous or pseudomembranous conjunctiva.
iii- Shedding of the membranes is followed by the development of focal
fibrotic patches (replacement by fibrous tissue).
Complications:
a- Symblepharon.
b- Metaplastic lashes: which have fine and arise from the openings of damaged
meibomian glands.
c- Epiphora: caused by lacrimal drainage obstruction and normal tear
production, but if there is normal lacrimal drainage but excessive production
then it is lacrimation.
d- Dry eye: due to obstruction of lacrimal ductules.
e- Keratopathy: secondary to:
i- Cicatricial entropion.
ii- Metaplastic lashes.
iii- Dry eyes.
Treatment:
a- Topical steroids may control vasculitis .
b- Scleral contact lens to prevent symblepharon.
c- Other measures:
i- Tropical retinoic acid for keratinization.
ii- Artificial tear.
iii- Punctate occlusion.
iv- Surgery to correct permanent deformities.
Conjunctival Degenerations
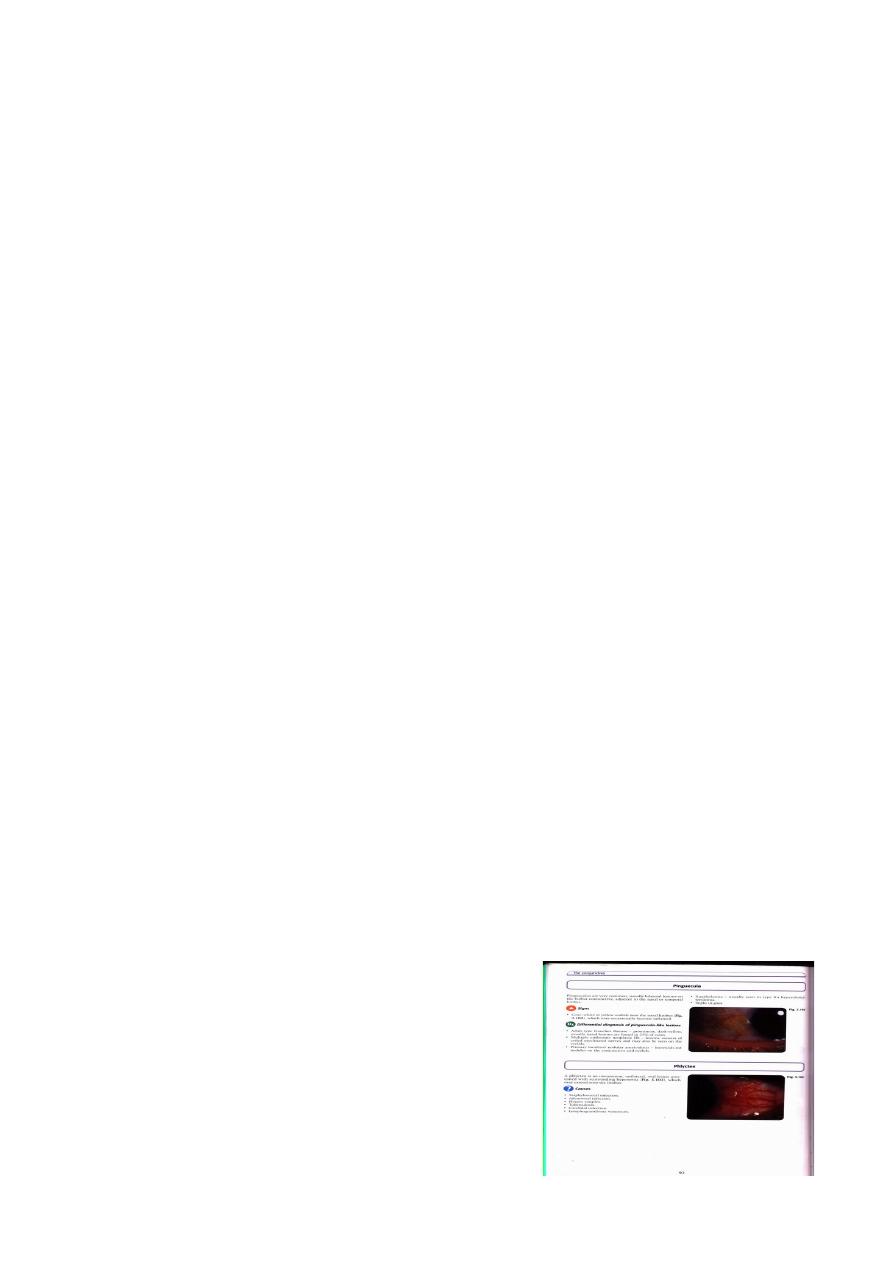
1- Pinguecula:
It is an extremely common lesion which
consists of a yellow-white deposit on the bulbar
conjunctiva adjacent to the nasal or temporal
aspect of the limbus and it is usually
asymptomatic.
Histology:
}
For treatment of dry
eye
66
Degeneration of the collagen fibers of the conjunctival stroma, thinning of the
overlying epithelium and occasionally calcification.
Some pinguecula may enlarge very slowly but surgical excision is seldom
required.
2- Concretions:
- They are small yellow-white deposits.
- Commonly present in the palpebral conjunctiva of the elderly.
- Also in patients with chronic meibomian gland disease.
- Usually asymptomatic, but occasionally causes foreign body sensation when
erode through the epithelium.
Treatment: They can be easily removed with a needle.
3- Pterygium:
- It is a triangular sheet of conjunctival
fibrovascular tissue invades the cornea.
- Occurs in patients who have been living in hot
climates.
- May represent a response to chronic dryness
and exposure to the sun.
Signs:
a- Small, grey, corneal opacities near the nasal limbus.
b- Then, the conjunctiva overgrows these opacities
and progressively invades onto the cornea in a
triangular fashion.
c- A deposit of iron (Stocker line) may be present in
the corneal epithelium anterior to the advancing
head of the pterygium.
* Usually asymptomatic.
Treatment:
Surgical excision: needed only in these cases:
i- If it is threatening the visual axis.
ii- For cosmetic reason.
iii- Severe irritation.
77
