Diabetic hypoglycemia
Dr .Adel Gassab MohammedMD. CABMS. MSc of Specialized Endocrine and Diabetes, Specialist Endocrinologist,
College of medicine
ORCID iD: https://orcid.org/0000-0001-9084-1038.
Email: adelgassab@utq.edu.iq
Overview
Hypoglycemia: is a clinical syndrome with diverse causes in which low plasma glucose concentrations lead to symptoms and signs, and there is resolution of the symptoms/signs when the plasma glucose concentration is raised .Diabetic hypoglycemia occurs when someone with diabetes doesn't have enough sugar (glucose) in his or her blood. Glucose is the main source of fuel for the body and brain, so you can't function well if you don't have enough.
Low blood sugar (hypoglycemia) is defined as a blood sugar level below 70 milligrams per deciliter (mg/dL), or 3.9 millimoles per liter (mmol/L).
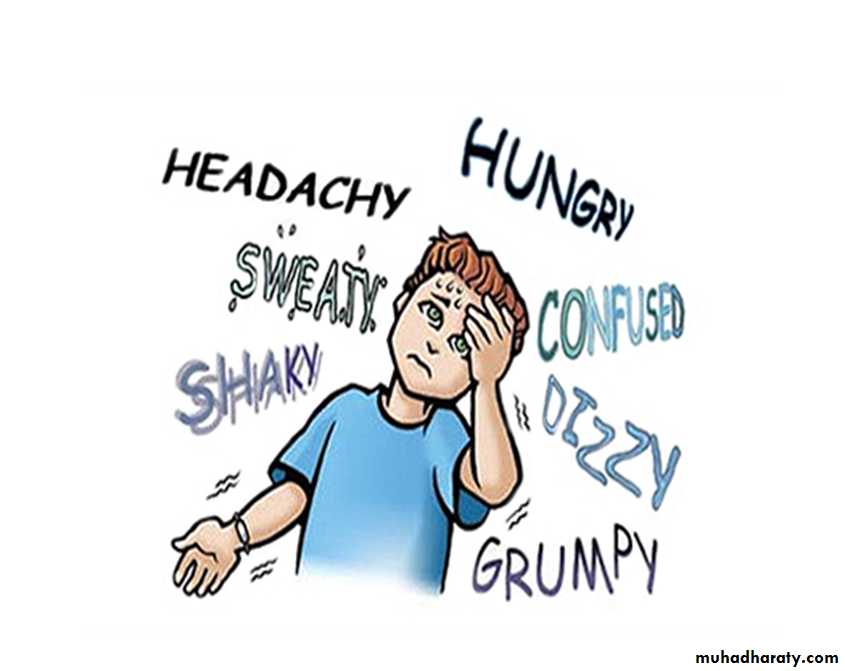
Symptoms
Early warning signs and symptomsInitial signs and symptoms of diabetic hypoglycemia include:
Shakiness
DizzinessSweating
Hunger
Fast heartbeat
Inability to concentrate
Confusion
Irritability or moodiness
Anxiety or nervousness
Headache
Nighttime signs and symptoms
Damp sheets or nightclothes due to perspirationNightmares
Tiredness, irritability or confusion upon waking
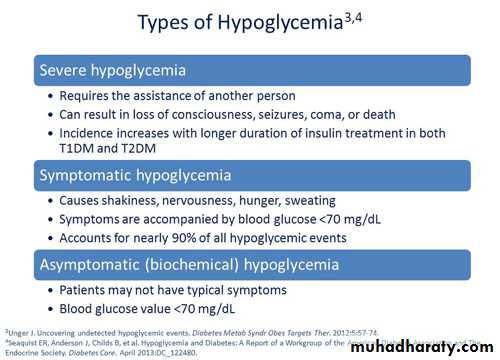
Severe signs and symptoms
Clumsiness or jerky movementsInability to eat or drink
Muscle weakness
Difficulty speaking or slurred speech
Blurry or double vision
Drowsiness
Confusion
Convulsions or seizures
Unconsciousness
Death, rarely
Causes
Common causes of diabetic hypoglycemia include:
Taking too much insulin or diabetes medication
Not eating enoughPostponing or skipping a meal or snack
Increasing exercise or physical activity without eating more or adjusting your medications
Drinking alcohol
RESPONSE TO HYPOGLYCEMIA IN DIABETES
The protective response to hypoglycemia is impaired inmany diabetic patients . The first defense, the ability to suppress
insulin release, cannot occur in patients with absolute beta-cell
failure ( those with type 1 diabetes and long-standing type 2
diabetes). Therefore, inhibition of hepatic glucose production
continues.
Thus, the main defense against hypoglycemia is increased
release of counter regulatory hormones (glucagon and
epinephrine), which raise plasma glucose concentrations by
stimulating glucose production and by antagonizing the insulin induced increase in glucose utilization.
Risk factors
Some people have a greater risk of diabetic hypoglycemia, including:People using insulin
People taking certain oral diabetes drugs (sulfonylureas)
Young children and older adults
Those with impaired liver or kidney function
People who've had diabetes for a longer time
People who don't feel low blood sugar symptoms (hypoglycemia unawareness)
Those taking multiple medications
Anyone with a disability that prevents a quick response to falling blood sugar levels
People who drink alcohol
Complications
If the patient ignore the symptoms of hypoglycemia too long, may lose consciousness. That's because the brain needs glucose to function. Recognize the signs and symptoms of hypoglycemia early, because if untreated, hypoglycemia can lead to:Seizures
Loss of consciousnessDeath
Take early symptoms seriously. Diabetic hypoglycemia can increase the risk of serious — even deadly — accidents.
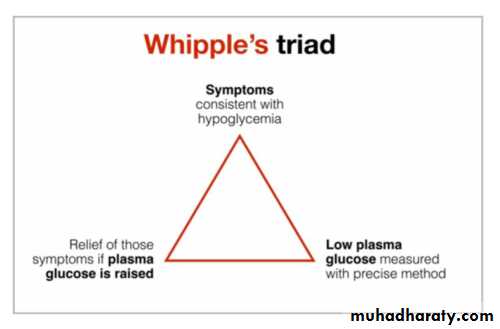
Diagnosis
If the have signs or symptoms of low blood sugar, check the blood sugar levels with a blood glucose meter — a small device that measures and displays the blood sugar level. hypoglycemia when the blood sugar level drops below 70 mg/dL (3.9 mmol/L).The diagnosis of hypoglycemia is not based on an absolute blood
glucose level; it requires fulfillment of the Whipple triad:I ) Signs and symptoms consistent with hypoglycemia
2) Associated low glucose level
3) Relief of symptoms with supplemental glucose
Laboratory tests
1) CBC2) Glucose
3) Insulin
4) C-peptide
5) Beta-hydroxybutyrate(Suppressed beta-hydroxybutyrate (< 1 µmol/L) in conjunction with low levels of free fatty acids (< 1 µmol/L) during hypoglycemia may indicate hyperinsulinism.)
6) Proinsulin
7) Antibodies for insulin and its receptors
8) Sulfonylurea and meglitinide screen
9) Electrolytes, BUN/Cr, UA
10) liver function tests, cortisol and thyroid levels , growth
hormone level
11) Other tests: ECHO, ECG, CXR , CT and MRI
Treatment Protocol
Initially
• Glucose 10-20 g is given by mouth, either in liquid
form or as granulated sugar (2 teaspoons) or sugar
lumps.
• GlucoGel® - formerly known as Hypostop® Gel -
may be used.
• Repeat capillary blood glucose after 10-15 minutes; if
the patient is still hypoglycemic then the above can
be repeated (probably up to 1-3 times).
1. Mild to moderate hypoglycemia should be
treated by oral ingestion of 15 g carbohydrate;glucose or sucrose crystals/ solutions are
preferable to orange juice and glucose gels.
Patients should retest blood sugar in 15 minutes
and retreat with another 15 g of carbohydrates if
BG remains <70mg/dl
2. Severe hypoglycemia in a conscious person
should be treated by oral ingestion of 20 g of
carbohydrate, preferable as glucose tablets or
equivalent.
Blood sugar should be retested in 15 minutes,
and then retreated with a further 15 g of glucose
if BG remains <70 mg/dl.
3. Severe hypoglycemia in an unconscious individual:
– No IV access: 1 mg of glucagon should beadministered subcutaneously or intramuscularly.
– Hypoglycemic effects (specially due to drugs) may
persist for 12-24 hours and ongoing glucose
infusion or other therapies such as octreotide may
be required
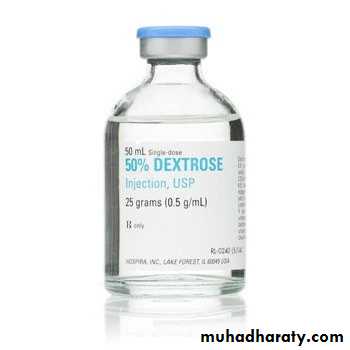
With IV access: 10-25 g (20-50 cc of D50W) of
glucose should be given intravenously over 1-3minutes.
• Retest in 15 minutes to ensure the BG >70mg/dl and
retreat with a further 15 g of carbohydrate if needed.
• Once conscious, eat usual snack or meal due at that
time of day or a snack with 15 g carbohydrate plus
protein.
Prolonged Hypoglycemic Coma:
Use IV mannitol and dexamethasone with constantglucose monitoring and IV glucose to keep serum
level at 70-80mg/dl until either consciousness has
been restored or permanent brain damage is
diagnosed.
Once the patient is more alert, carbohydrate
should be given, e.g. toast, or a normal meal. Forinpatients, an infusion of 10% glucose may be
administered if required.
A complication of diabetes in which the patient is unaware of a deep drop in blood sugar because it fails to trigger the secretion of epinephrine which generates the characteristic symptoms of hypoglycemia (such as palpitations, sweating, anxiety)
occurs more frequently in those who: Frequently have low blood sugar episodes.
The good news is, hypoglycemia unawareness is reversible simply by avoidance of hypoglycemia for 7–21 days (setting target blood glucose levels higher)