Thi Qar University College of Medicine Internal Medicine Department
GIT LECTURES 2017Dr. FAEZ KHALAF, SUBSPACIALITY GIT
MBChB,FIBMS-CABMS(MED),MD-FACP(US),FIBMS(GIT&HEP)
IRRITABLE BOWEL SYNDROME
• Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by abdominal pain or discomfort and altered bowel habits in the absence of detectable structural abnormalities.• Approximately 20% of the general population fulfil diagnostic criteria for IBS but only 10% of these consult their doctors because of gastrointestinal symptoms ..
• Female predominant
Pathophysiology
Behavioural and psychosocial factors
Physiological factors
Luminal factors
Most patients seen in general practice do not have psychological
problems but about 50% of patients referred to hospital have a psychiatric illness, such asanxiety, depression, somatisation and neurosis, Panic attacks are also common.
Acute psychological stress and overt psychiatric disease are known to
• alter visceral perception
• and gastrointestinal motility.
Behavioural and psychosocial factors
Physiological factors
(5-HT) disorder, as evidenced by relatively excessiverelease of 5-HT in diarrhoea-predominant IBS (D-IBS)
and relative deficiency with constipation-predominant
IBS (C-IBS).
There is some evidence that IBS may represent a state of low-grade gut inflammation or immune activation, not detectable by tests, with raised numbers of mucosal mast cells, patients respond positively to mast cell stabilisers, such as ketotifen, which supports a pathogenic role of mast cells in at least some patients.
Immune activation may be associated with altered CNS processing of visceral pain signals. This is more common in women and in D-IBS, and may be triggered by a prior episode of gastroenteritis with Salmonella or Campylobacter species.
Luminal factors
bacterial contents (the gut microbiota) have been reported. Small intestinal bacterial overgrowth (SIBO) This ‘gut dysbiosis’ may explain the response to probiotics or the non-absorbable antibiotic rifaximin that has been reported in trials.
Dietary factors are chemical food intolerances (not allergy) to poorly absorbed, short-chain carbohydrates (lactose, fructose and sorbitol, among others), collectively known as FODMAPs (fermentable oligo-, di- and monosaccharides, and polyols). Their fermentation in the colon leads to bloating, pain, wind and altered bowel habit. Noncoeliac gluten sensitivity (negative coeliac serology and normal duodenal biopsies) seems to be present in some IBS patients,
while others may be intolerant of chemicals such as salicylates or benzoates, found in certain foods.
Etiology
The pathogenesis of IBS is poorly understood• psychosocial factors
anxiety
depression
somatisation and neurosis
• altered gastrointestinal motility
no consistent evidence of abnormal motility
• altered visceral sensation
a consequence of altered central nervous system processing of visceral sensation.
• luminal factors
• following an episode of gastroenteritis
• intolerant of specific dietary components, particularly lactose and wheat
• gut microflora
Clinical features
• Colicky abdominal pain• Altered bowel habit
• Abdominal distension
• Rectal mucus
• Feeling of incomplete defecation
•
Abdominal Pain
• Abdominal pain episodic and crampy(lower)
• may be mild enough to be ignored or it may interfere with daily activities.
• Pain is often exacerbated by eating or emotional stress and improved by passage of flatus or stools
• Sleep deprivation is also unusual
Altered Bowel Habits
• The most common pattern is constipation alternating with diarrhea, usually with one of these symptoms predominating.
• Stools are usually hard with narrowed caliber
• Diarrhea resulting from IBS usually consists of small volumes of loose stools
• Nocturnal diarrhea does not occur
• Diarrhea may be aggravated by emotional stress or eating.
• Stool may be accompanied by passage of large amounts of mucus
Gas and Flatulence
abdominal distentionincreased belching
flatulence,
Most IBS patients have impaired transit and tolerance of intestinal gas loads
The diagnosis
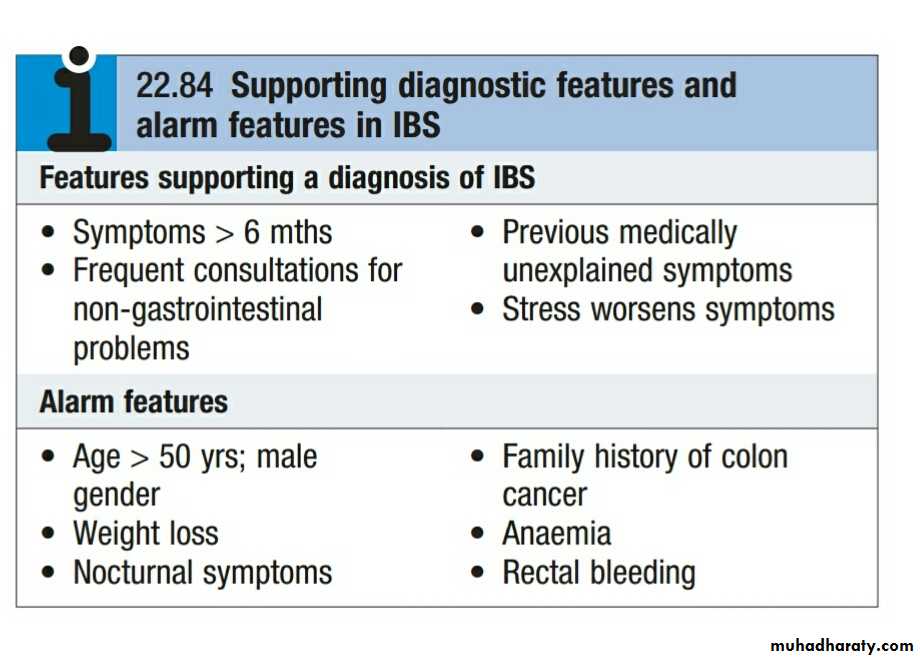
is clinical with excluding secondary disease if neededFeatures supporting a diagnosis of IBS
• Symptoms > 6 months without progressive deterioration,
• absence of other systemic symptoms such as fever and weight loss
• small-volume stool without any evidence of blood.
• Frequent consultations for non-GI problems
• Previous medically unexplained symptoms
• Stress worsens symptoms
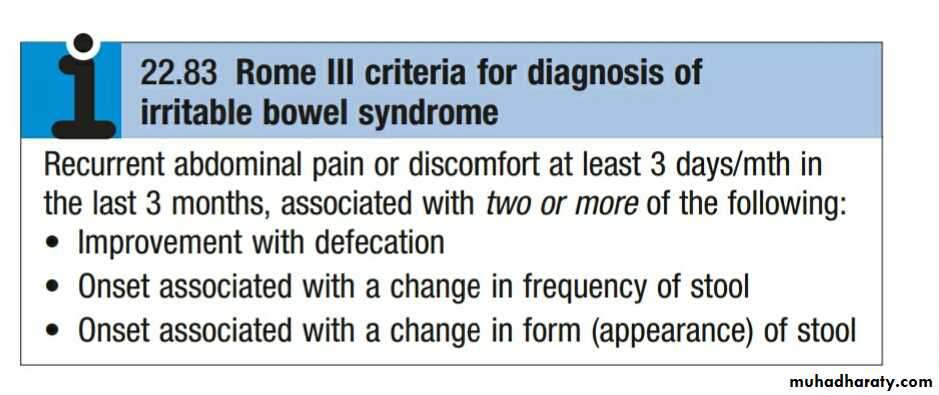
Diagnostic Criteria (Rome)
Recurrent abdominal pain or discomfort at least 3 days per month in the last 3 months associated with two or more of the following:
• 1. Improvement with defecation
• 2. Onset associated with a change in frequency of stool
• 3. Onset associated with a change in form appearance) of stool
Investigation
minimal for typical symptomif we need:
• Full blood count
• GSE
• lower GI endoscopy
(sigmoidoscopy, Colonoscopy)
alarm features.
Diarrhoea-predominant
Alarm features
• Age > 50 years; male gender• Weight loss
• Nocturnal symptoms
• Family history of colon cancer
• Anaemia
• Rectal bleeding
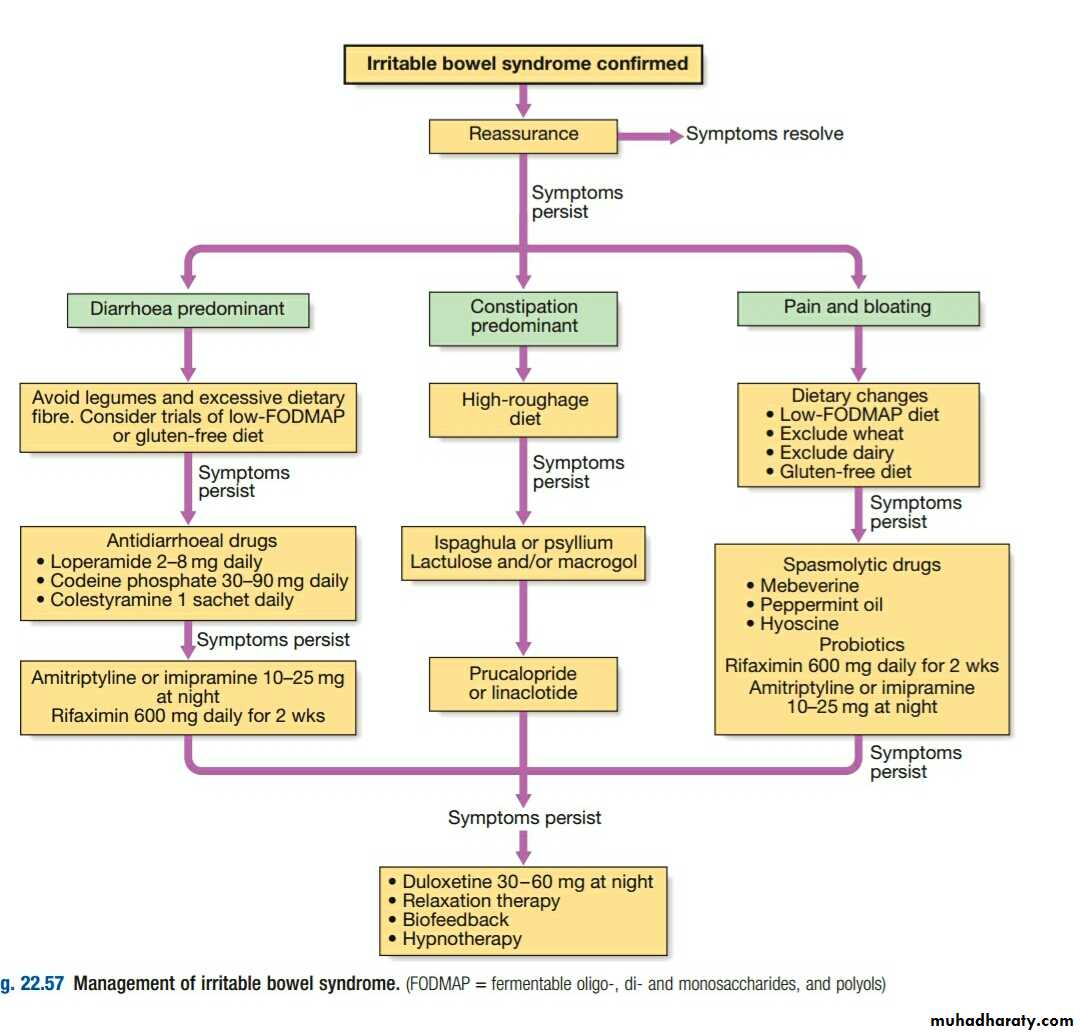
Management
• Diagnosis• Reassure the patient and
• Dietary alteration
wheat-free diet
lactose exclusion
• Treatment of the predominant symptoms
• Therapy with tricyclic antidepressant
• 5-HT4 agonists
Psychological interventions
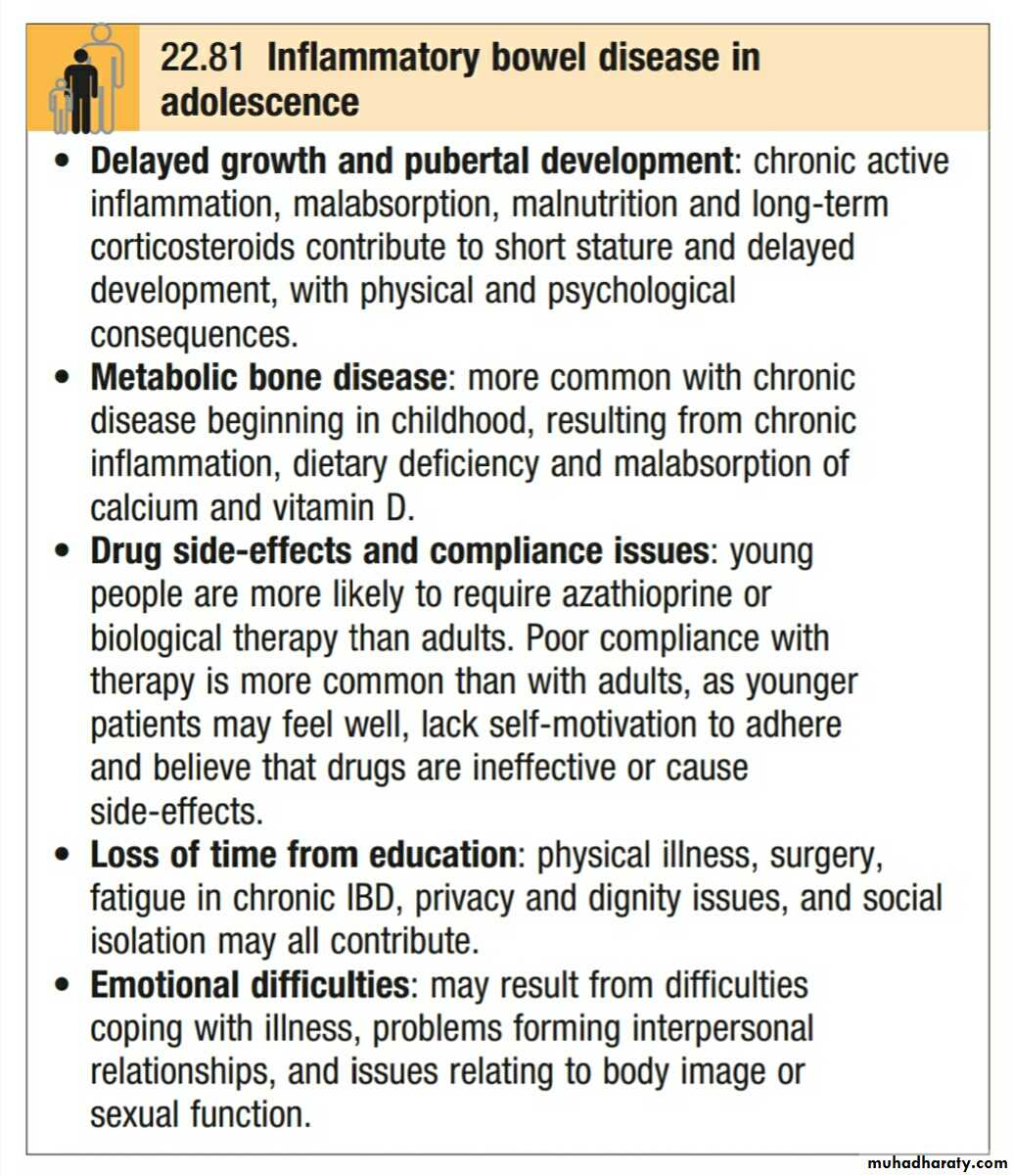
IBD in special circumstances
Childhood: Chronic ill health in childhood or adolescent IBD may result in• Growth failure.
• Metabolic bone disease
• Delayed puberty.
• Loss of schooling and social contact,
• As well as frequent hospitalization, can have important psychosocial consequences.
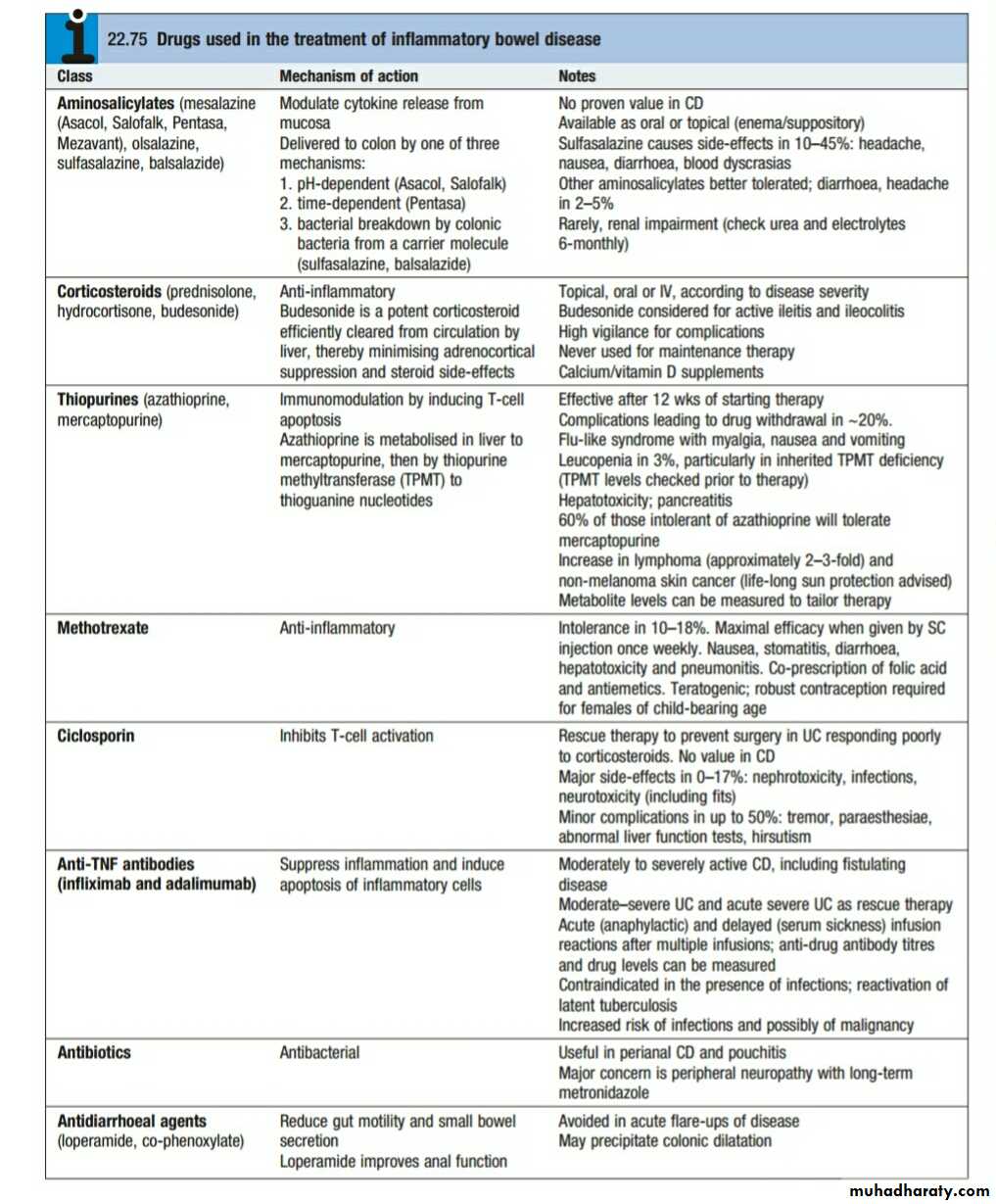
Treatment is similar to that described for adults and may require corticosteroids, immunosuppressive drugs, biological agents and surgery.
Monitoring of height, weight and sexual development is crucial.
Metabolic bone disease
Patients with IBD are prone to developing osteoporosis due to effects of• Chronic inflammation.
• Corticosteroids.
• Weight loss.
• Malnutrition and malabsorption.
Osteomalacia can also occur in Crohn’s disease that is complicated by malabsorption, but is less common than osteoporosis. The risk of osteoporosis increases with age and with the dose and duration of corticosteroid therapy.
Microscopic colitis
which comprises two related conditions, lymphocytic colitis and collagenous colitis, has no known cause. The presentation is with watery diarrhoea. The Colonoscopic appearances are normal but histological examination of biopsies shows a range of abnormalities. It is therefore recommended that biopsies of the right and left colon plus terminal ileum should be undertaken in all patients undergoing colonoscopy for diarrhoea. Collagenous colitis is characterised by the presence of a sub mucosal band of collagen, often with a chronic inflammatory infiltrate. The disease is more common in women and may be associated with rheumatoid arthritis, diabetes, coeliac disease and some drug therapies, such as NSAIDs or PPIs.Treatment with budesonide is usually effective but the condition will recur in some patients on discontinuation of therapy.