U N I V E R S I T Y O F M O S U L
C O L L E G E O F
D E N T I S T R Y
2020-2021
Department of
Conservative
Dentistry
5th stage
• Bleaching is lightening of the color of teeth through
application of chemical agent to oxidize organic
pigmentation in teeth.
• As a compare with crowning or veneer bleaching
is efficient, simple, most common, less expensive
and less invasive.
• Problems associated with bleaching are teeth
sensitivity and gingival ulceration, especially when
higher concentrations of bleaching agents is used.
• The desire to have whiter teeth has been documented
since the mid-nineteenth century.
• Bleaching of pulpless teeth was first described by
Truman 1864 . variety of medicaments (chloride,
sodium perborate and hydrogen peroxide were used
with or without heat activation.
• At the end of 19th century, dentists began to bleach
vital teeth.
• In 1989 10% of carbamide peroxide used in a mouth
guard for lightening teeth color.
• In-office professional whitening become the most
popular system for whitening the teeth.
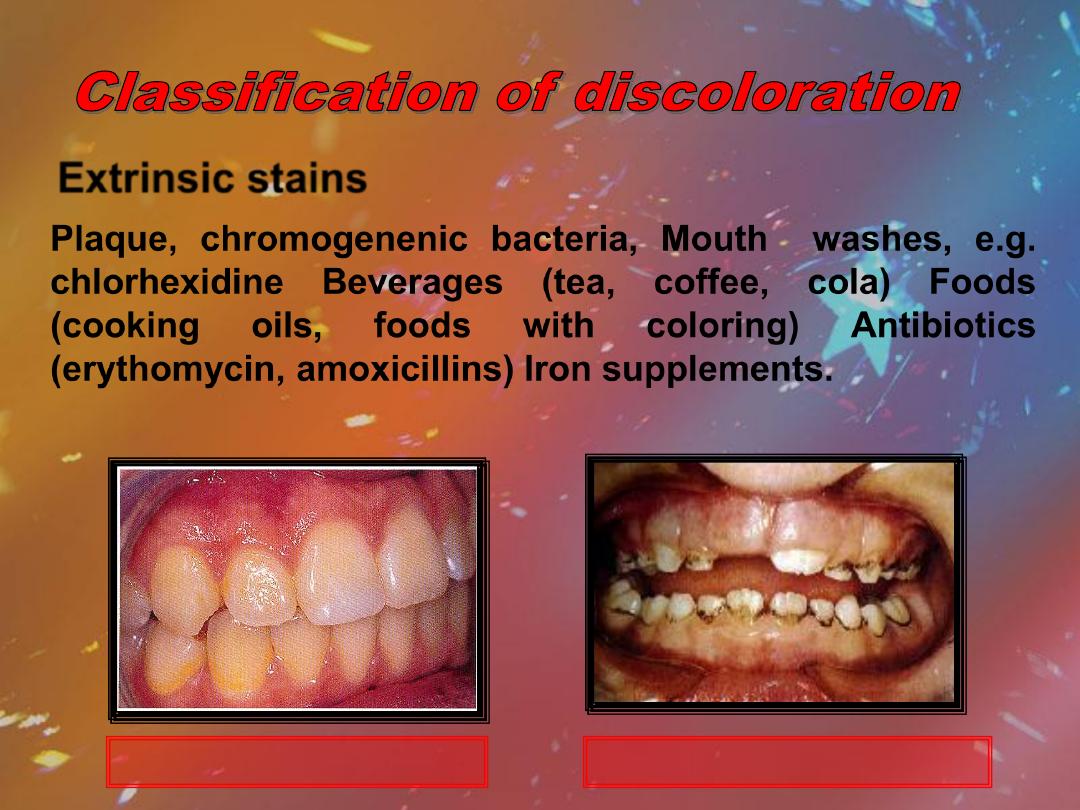
Extrinsic stains
Plaque, chromogenenic bacteria, Mouth washes, e.g.
chlorhexidine Beverages (tea, coffee, cola) Foods
(cooking
oils,
foods
with
coloring)
Antibiotics
(erythomycin, amoxicillins) Iron supplements.
Yellow stain from plaque
Chlorhexidine induced stain

Extrinsic stains
Coffee staining
Patient with respiratory tract infection
and use antibiotics
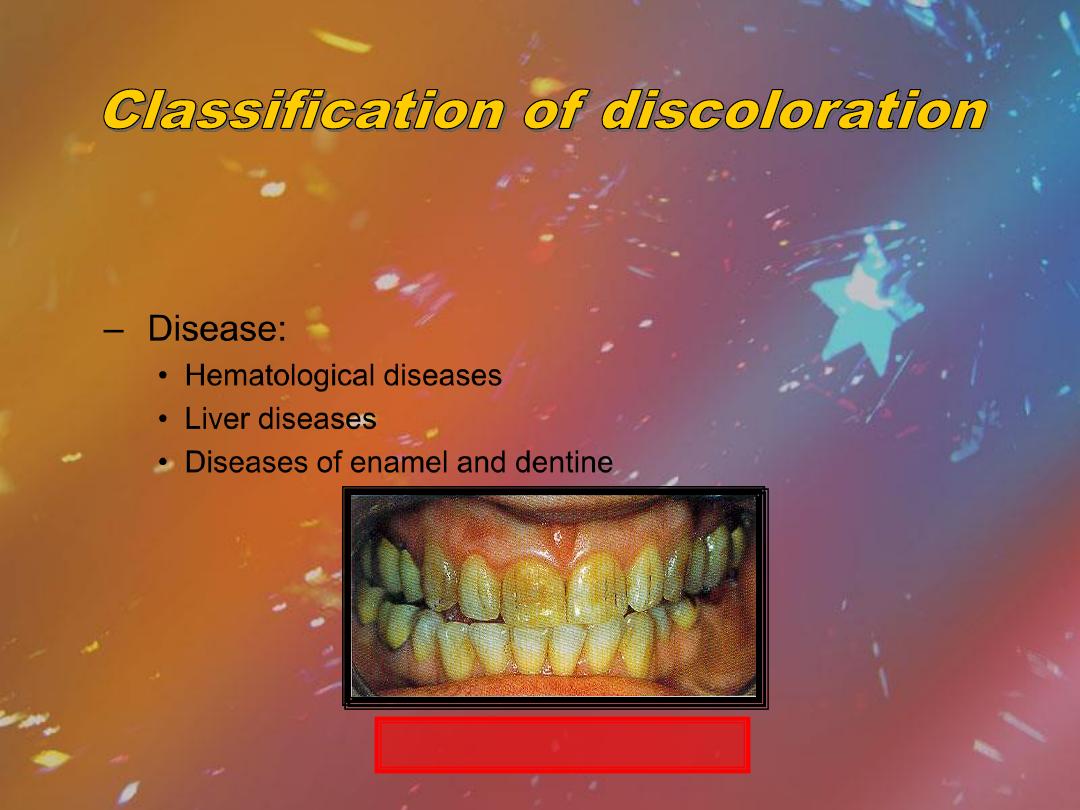
– Disease:
• Hematological diseases
• Liver diseases
• Diseases of enamel and dentine
•Intrinsic stains
•
Pre-eruptive
Amelogenesis imperfecta

•Intrinsic stains
•
Pre-eruptive
–Medication:
•Tetraycline stains
•Fluorosis stains
Tetracycline staining
Fluorosis
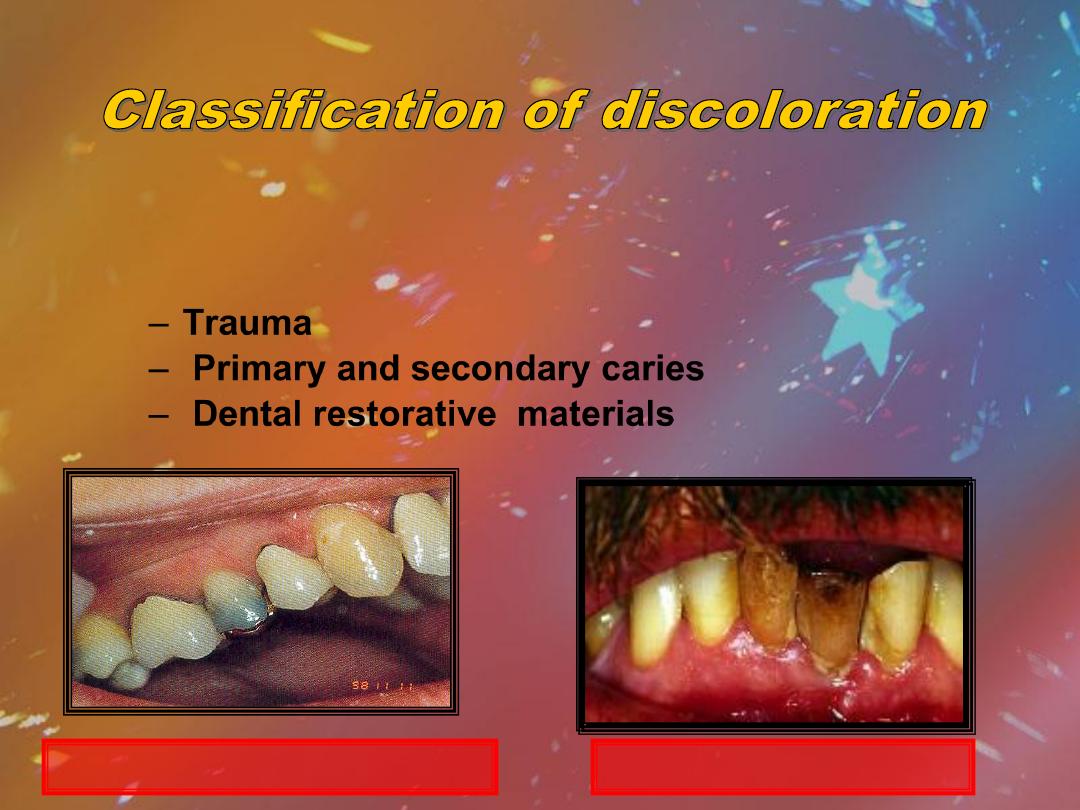
– Trauma
– Primary and secondary caries
– Dental restorative materials
•Intrinsic stains
•
Post-eruptive
Trauma to the centrals
Premolar has an amalgam core

•Intrinsic stains
•
Post-eruptive
–Ageing
– Smoking
– Chemicals
Tobacco discoloration

•Intrinsic stains
•
Post-eruptive
–Minocycline ( semi synthetic second-generation
tetracycline derivative)
– Functional and Para functional changes
Attrition
General Indications of
Bleaching
1. Generalized staining.
2. Ageing.
3. Extrinsic stain - Smoking and dietary stains
(tea/coffee).
4. Fluorosis.
5. Tetracycline staining (in combination with
restorative techniques).
6. Traumatic pulpal changes.
7. Discoloration of anterior teeth after RCT.
Contraindications of
Bleaching
1. Patients with high/unrealistic expectations.
2. Pregnancy/Breastfeeding.
3. Sensitivity/cracks/exposed dentine.
4. Existing crowns / large restorations.
5. Elderly patients with visible recession
.
6. Peroxide allergy.
7. Generalized dental caries.
8. Decay and active periapical pathology (must be
resolved first).
Bleaching is a complex chemical process works by
oxidation. Bleaching slowly transforms organic substance
into chemical intermediates that are lighter in color.
In oxidation-reduction reaction oxidizing agent (H2O2)
has free radicals with unpaired electrons, oxidizing agent
gives up unpaired electrons and becomes reduced; the
reducing agent (bleached substance) accepts the electrons
and becomes oxidized.
•
Oxidizing agent (H2O2) diffuses through the organic matrix of
the enamel and dentin because of its low molecular weight.
•
The free radicals attack organic molecules to achieve stability;
this releases other radicals which intern can react with other
unsaturated bonds.
•
bleaching opens highly pigmented carbon-ring compounds and
converts them to chains that are lighter in color. Bleaching
process continues to the extent that all the original pigment is
rendered essentially colorless, beyond that continuation of the
bleaching process is not beneficial.
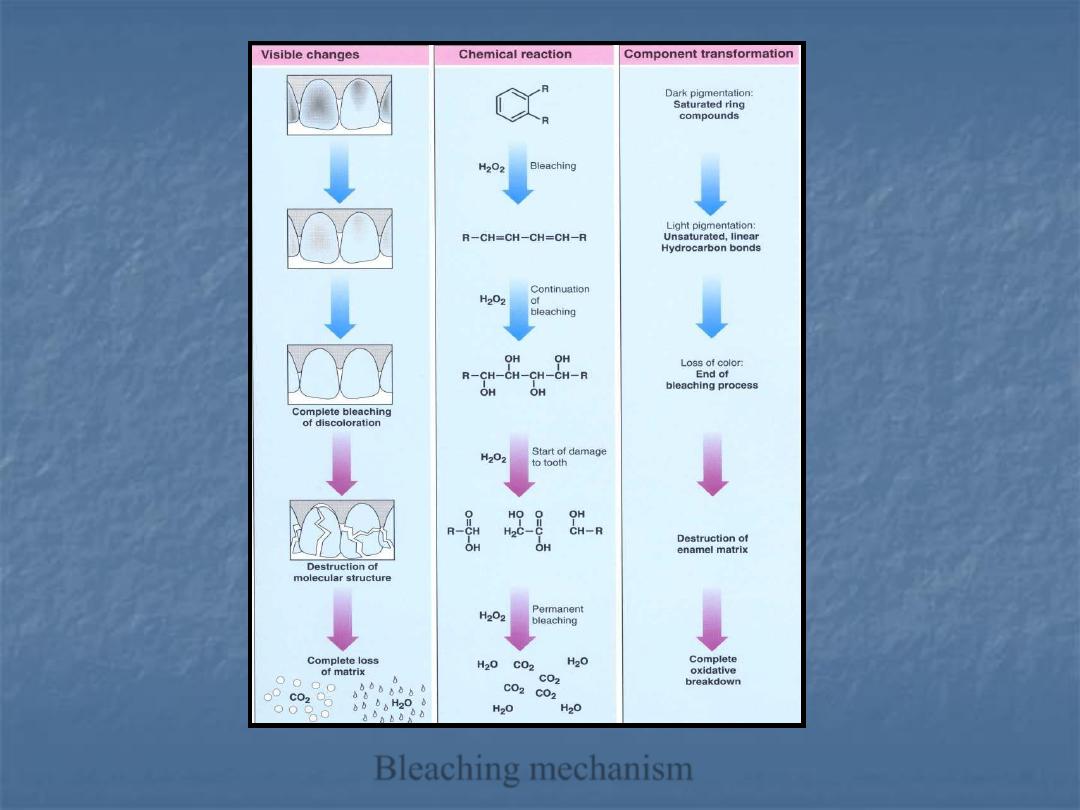
Bleaching mechanism
1- Bleaching Agent :
For example Hydrogen Peroxide , Carbamide Peroxide , Sodium
Perborate , Sodium Percarbonate
The ideal criteria of bleaching agent are:
a- Easy to apply
b- Non acidic
c- Lighten teeth successfully and efficiently
d- Minimum amount of bleaching agent to get desired result
f- Not irritate oral tissues
g- Not cause damage to the teeth
h- Well controlled by the dentist
2- Thickening agent-Carbopol.
3- Urea Stabilize hydrogen peroxide,elevate pH and enhance other
desirable qualities as anticariogenic effects and saliva
stimulation.
4- Vehicle –glycerine enhance viscosity of preparation and eases
manipulation.
5- Surfactant (surface wetting agent).
6- Preservatives (citroxain) give greater durability and stability.
7- Flavorings (Melon, banana flavors).

– 1. Type of Bleach.
– 2. Concentration and Time.
– 3. Mode of Application.
– 4. pH Value.
– 5. Type of Stain.
– 6-Patient's Age.
– 7. Surface Cleanliness.
– 8. Sealed Environment.
– 9. Heat and Light Activation.
1. In-office bleaching: this includes
A- dentist-administered bleaching (Power
bleaching).
B- dentist-supervised bleaching (Waiting room
bleaching).
2. Home bleaching.
3. Over-the-counter bleaching.
4. Walking bleaching (internal bleaching).
1- In-Office Bleaching
The first bleaching of teeth to change color was
an in-office procedure. Both vital and non vital
teeth can be bleached by this technique.
A-Dentist-Administered Bleaching (Power
Bleaching).
B-Dentist-Supervised Bleaching (Waiting Room
Bleaching).
A-Dentist-Administered Bleaching (Power
Bleaching)
In this procedure high concentration of tooth
whitening agents (25
–40% hydrogen peroxide) is
used. Whitening gel is applied to the teeth and the
peroxide will be activated (or not) by light for
around one hour in the dental office. Different types
of lights can be used such as halogen curing
lights, Plasma arc lamp, Lasers. Light exposure
activate bleaching gel by specific catalyst or by
heat .

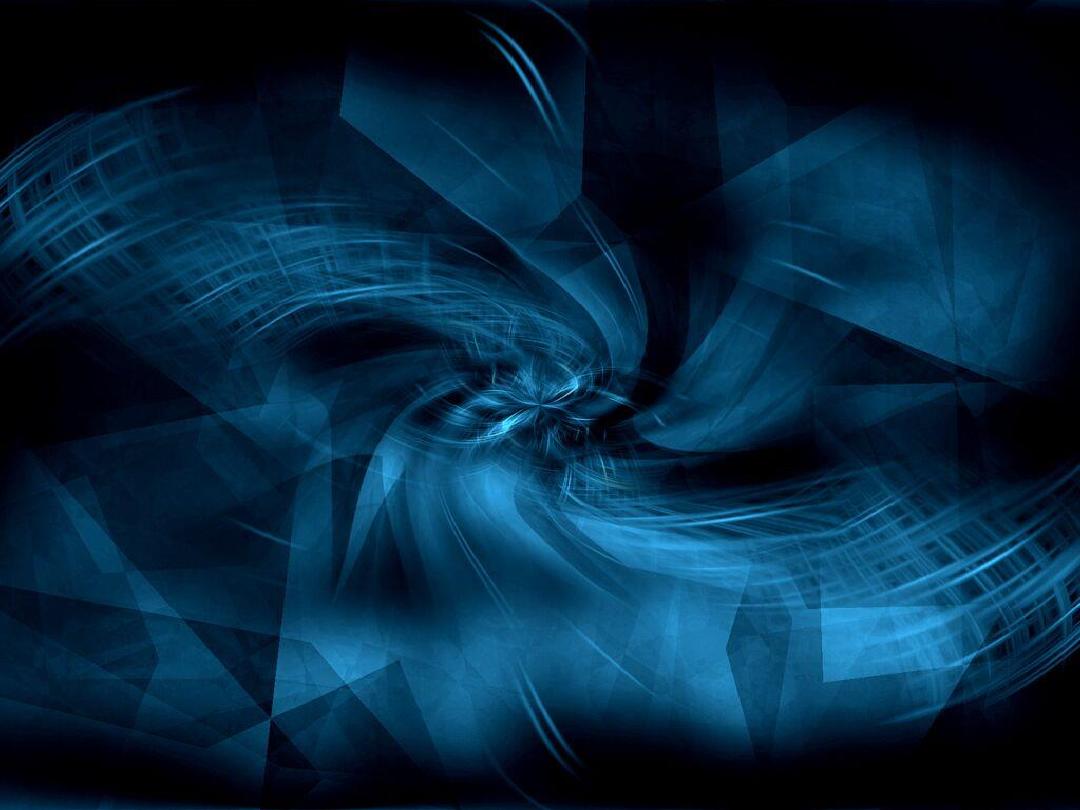
Prophylaxis of the
tooth.
The gingiva is isolated with
a rubber dam.
Protective eyewear is mandatory for
patient, dentist and dental assistant.
gingiva is protected with a
continuous coating.
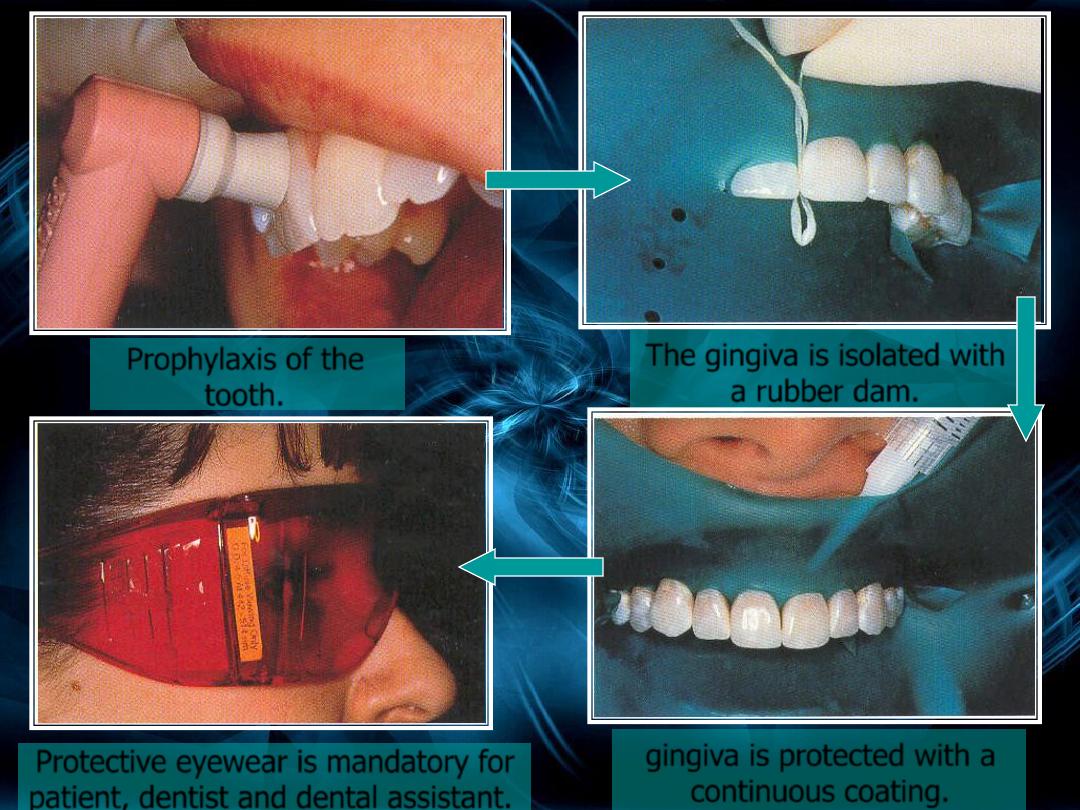
The gel is mixed in a
good consistency.
Application of the gel.
Light source used to accelerate
the oxidation process.
Removal of the spent
bleaching material
Manufacturer instruction should be observed
particularly appropriate timing that the material
remain
on
the teeth. After that bleaching material is
removed from the teeth and teeth are washed. the
bleach is reapplied for further 10 min., the process
is repeated for 45 min. to 1 hour.
After that teeth are polished with diamond polishing
paste, dam and mucosal protective is removed and the
mouth is rinsed finally the shade of the teeth is now
assessed .
B-Dentist-Supervised Bleaching (Waiting
Room Bleaching)
It is recommended for patients with TMJ problems or for
patients who do not want use tray at home. In this
technique bleaching tray containing high concentration of
carbamide peroxide (35-40%) placed in the patient's
mouth for 30 minutes to two hours in the dental office.
Advantages of In-Office Bleaching
Technique
1. Greater potential for immediate results that may
enhance patient satisfaction and motivation.
2. Dentist control.
3. Avoidance of soft tissue exposure and material
ingestion.
4. Reduced total treatment time.
5. Less pain inducing application.
Disadvantages of In-Office Bleaching
Technique
1. High cost.
2. Unpredictable result.
3. Unknown duration of treatment.
4. Potential for soft tissue damage to patient and
provider.
5. Rubber dam discomfort.
6. Teeth sensitivity.
7. Nausea from swallowing but rare.
8. Extra office time.
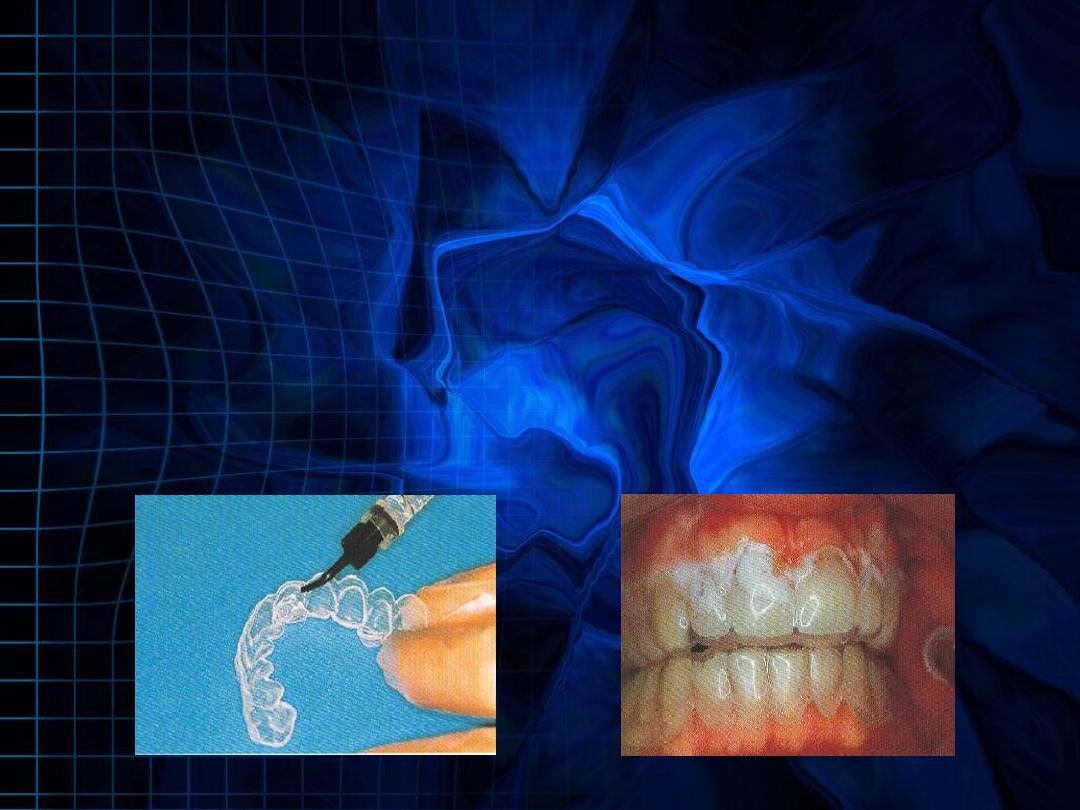
2-Home Bleaching (Night Guard Vital
Bleaching Dentist-Prescribed Bleaching)
Technique involves the use of custom-fitted mouth
guard that contains low concentration of whitening
agent (10
–20% carbamide peroxide). There are two
regimes for application of whitening agents: sleeping
with prosthesis loaded with material or wearing
loaded prosthesis during day. Night wear uses one
application while day wear uses 1-2 applications of
1-2 hours duration. Treatment time is generally 2-6
weeks.
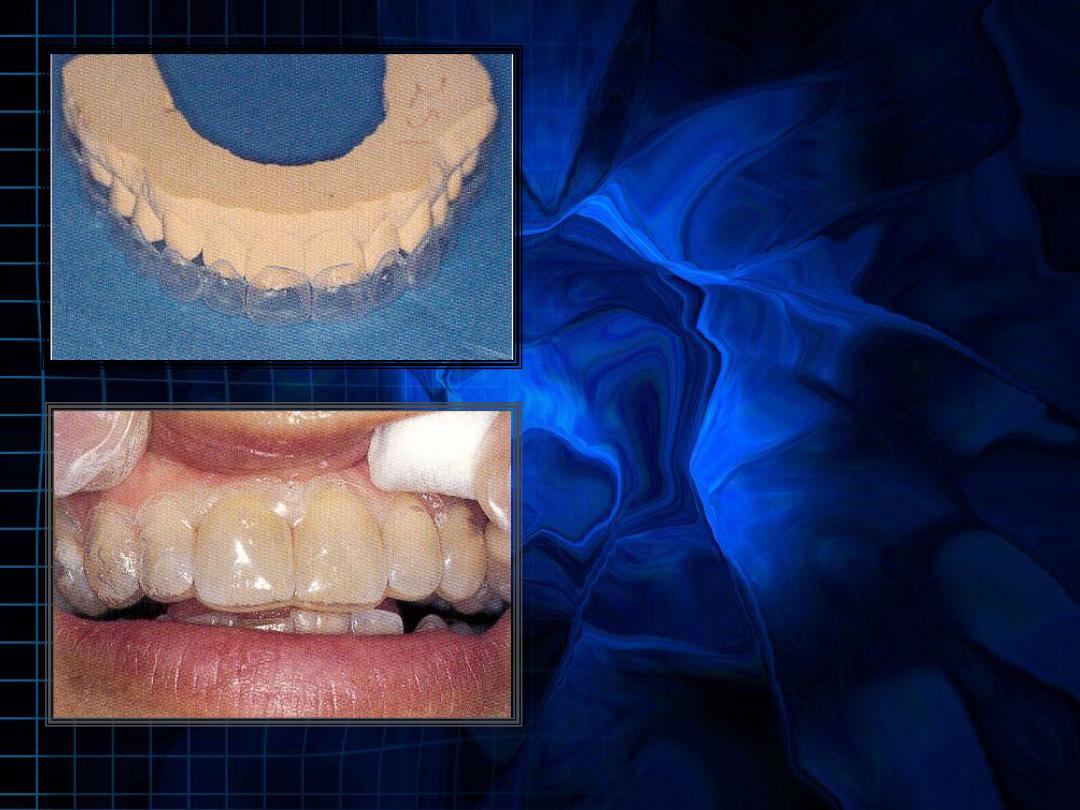
Custom-fitted mouth
guard
Mouth guard loaded
with bleaching material
Advantages of Home Bleaching
Technique
1. Ease of application.
2. Reduced chair time and cost.
3. High success rate.
4. Safety of materials used.
Disadvantages of Home Bleaching
Technique
1. Teeth sensitivity.
2. Gingival or stomach irritation.
3. It is a long time procedure.
4. Discomfort from wearing the trays.
5. It requires patient compliance.
6. Unpleasant taste.
7. Uneven tooth bleaching.
3-Over-The-Counter Bleaching
Manufacturers develop many Over the counter
bleaching products like Toothpastes, mouth
rinses, gums and strips.
These products are composed of a low
concentration of whitening agent (3
–6% hydrogen
peroxide). They are self-applied to the teeth and
should be applied twice per day for up to 2 weeks
A- Advantages of Over the Counter
Bleaching
1. Inexpensive.
2. Convenient.
3. Easy to use.
4. Represent fastest growing segment of market.
bleaching strips
Disadvantages of Over the Counter
Bleaching
1. Needs patient compliance. Patients may not
use product properly or long enough
2. Over use may lead to erosion, dissolution of
enamel and sensitivity.
3. Lack of diagnosis. Patients may misdiagnose
the cause of discoloration

4-Walking Bleaching (Internal or Intracoronal Bleaching)
It is commonly carried out on discolored anterior teeth
that have been endodontically treated.
Sodium perborate (SP) which mixed with distilled
water in ratio of 2:1 and placed into pulp chamber
was best agent for intracoronal bleaching. In case of
severe discoloration, 3% H
2
O
2
can be applied in place
of water.
Use of 30% H2O2 is not appropriate because of
possible risks of cervical resorption.
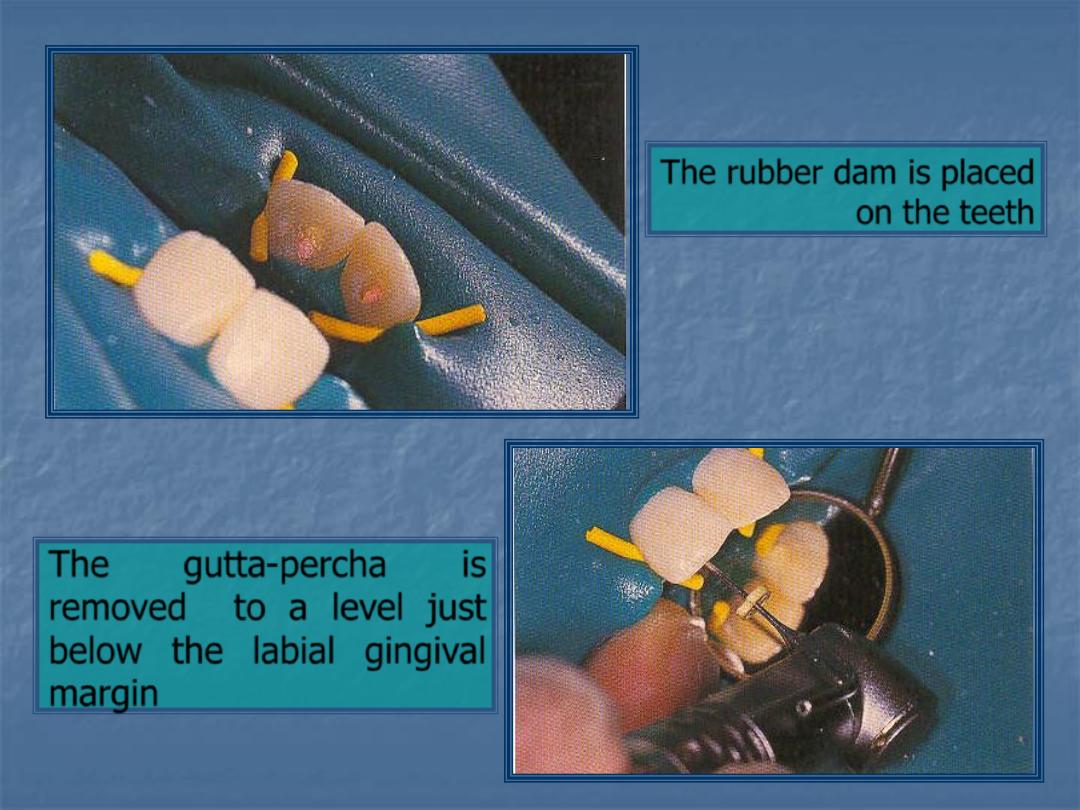
The rubber dam is placed
on the teeth
The
gutta-percha
is
removed to a level just
below the labial gingival
margin
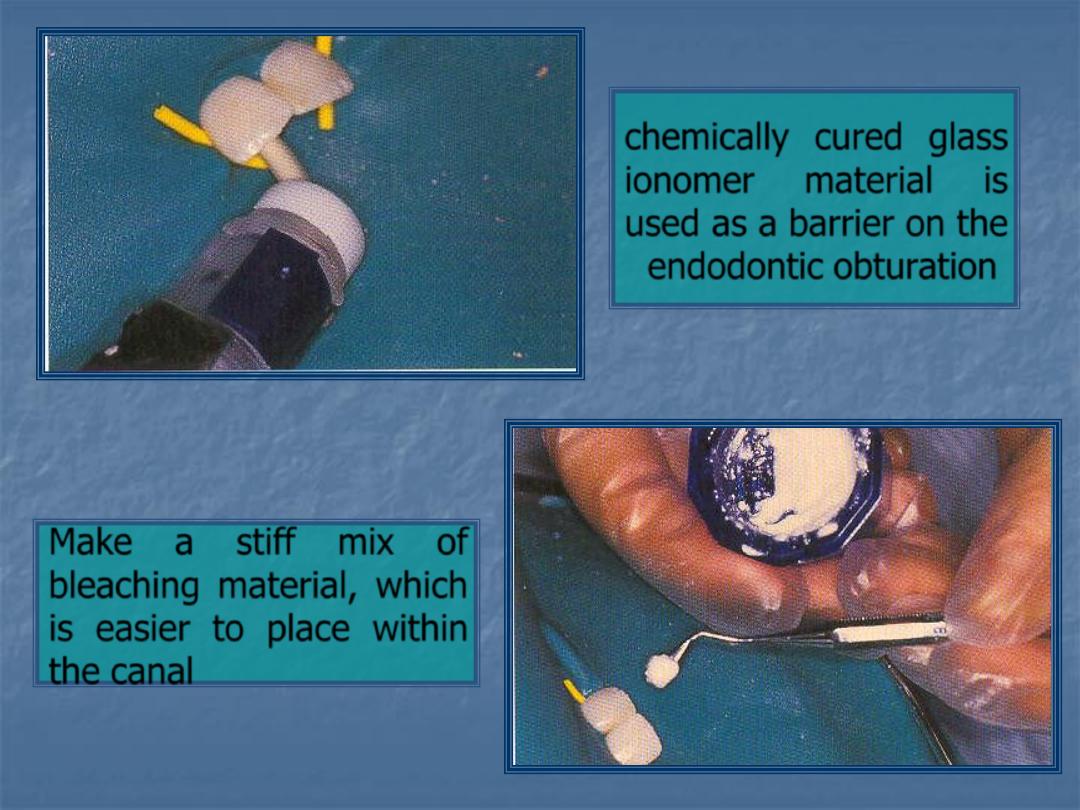
chemically cured glass
ionomer material is
used as a barrier on the
endodontic obturation
Make a stiff mix of
bleaching material, which
is easier to place within
the canal

• Apply a thick, well-sealed temporary
filling to ensure a good seal.
• Recall the patient approximately 2
weeks later and if necessary repeat the
procedure several times.
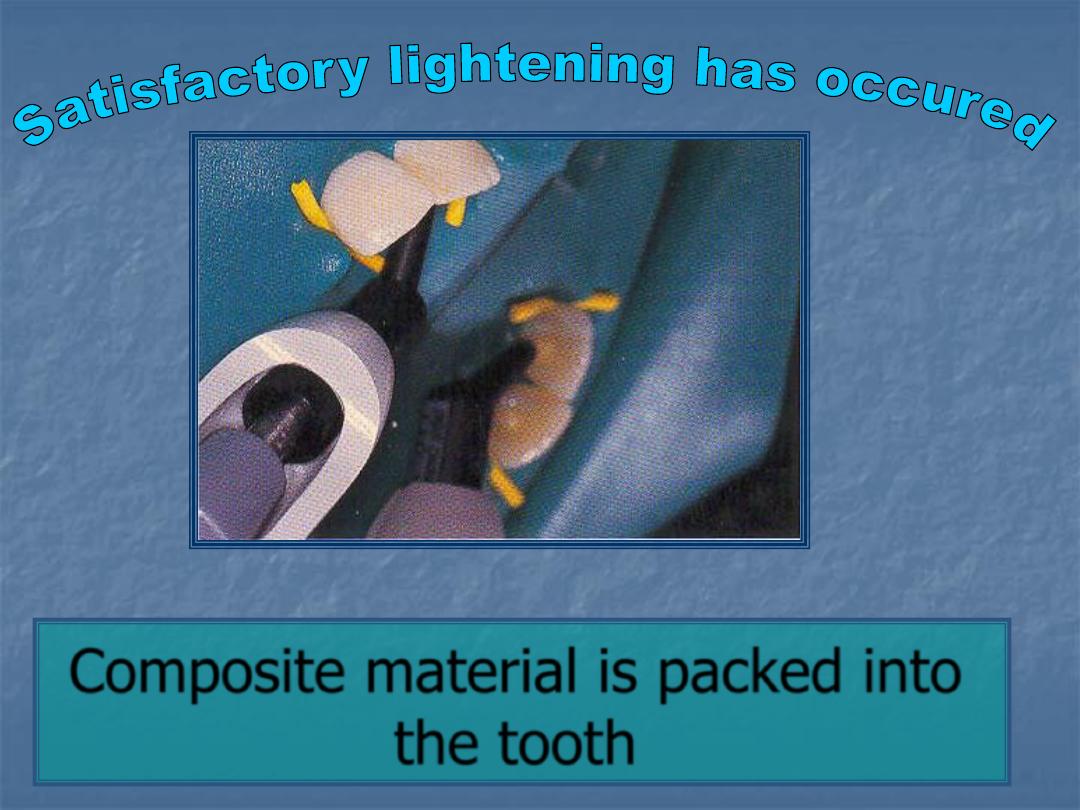
Composite material is packed into
the tooth
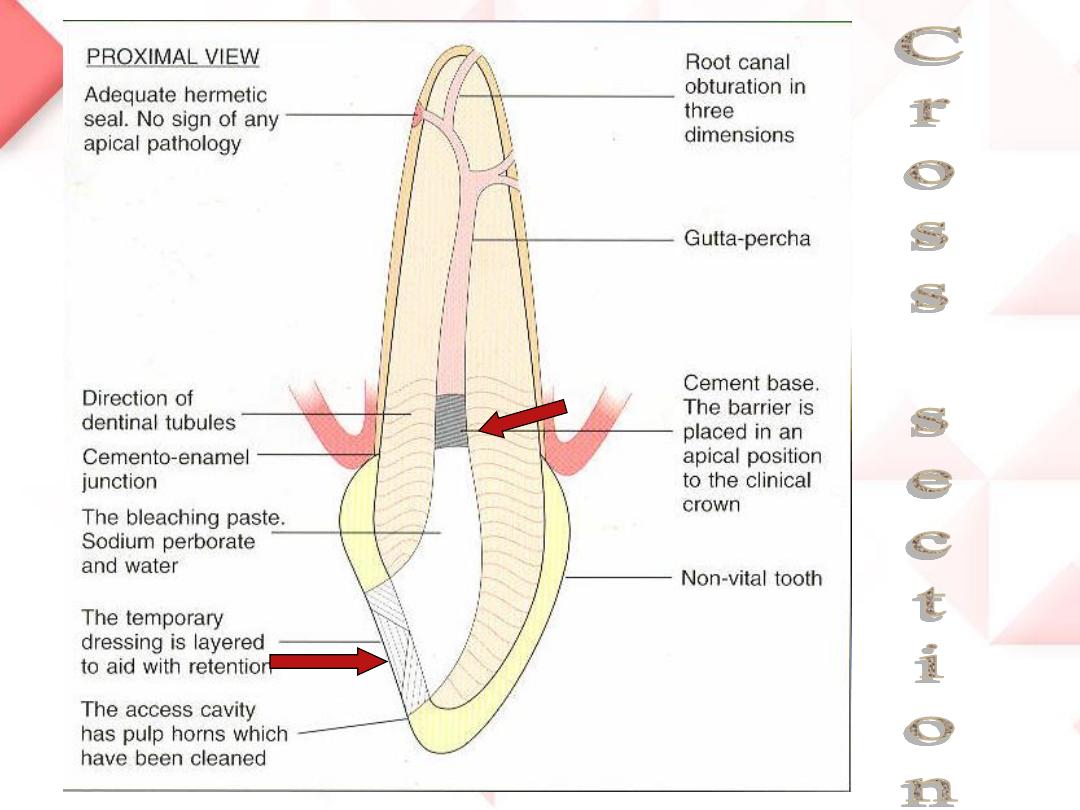
Cross section
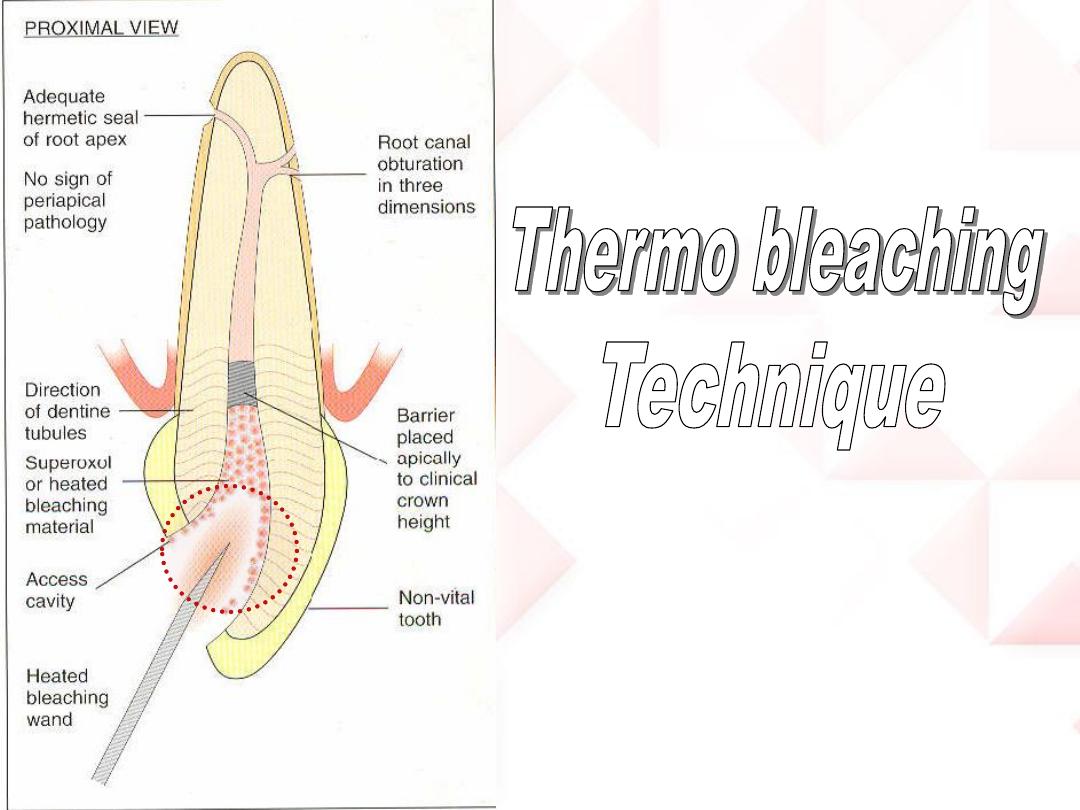

•30-35 H
2
O
2
solution in small cotton pellet place in
pulp chamber
•Apply heat device or light source temperature 50-
60 C. bleaching should be limited to separate 5 min.
period rather than long continues period
•Remove heat or light source and allow teeth to
cool. then wash with warm water.
•Dry tooth and place bleach past (SP mixed with
distilled water)
in the pulp chamber.
•Recall the patient approximately 2 weeks later.
A- Advantages of Intracoronal Bleaching
Technique
1. More conservative than other esthetic treatment
like crown or veneer.
2. Effective and efficient.
3. Safe and popular.
4. Evaluation color over the time.
5. Reduced chair time.
Disadvantages of Intracoronal Bleaching
Technique
1. Tooth fracture due to extensive removal of intra
coronal dentin also bleaching with H
2
O
2
reduce
micro-hardness of dentin and enamel.
2. Careful examination is necessary, since
method requires healthy periodontal tissues
and properly obturated root canal to prevent
bleaching agent from reaching periapical
tissues.
3. Swelling of papilla or percussion sensitivity of
bleached teeth can be observed.
4. External cervical resorption or even internal
resorption can be observed.

•
Gingiva
•Minor gingival irritation and/or ulceration.
•Gingival soreness.
•
Oral mucosa
•Sore throat.
•Unpleasant taste.
•Burning palate.
•
Gastrointestinal
•Gastrointestinal Irritation.
• Minor upsets in the stomach or intestines.
Effects of the bleaching process

•
Resin Polymerization and Bonding
Strength
Oxygen inhibits resin polymerization; consequently, residual H2O2 in
tooth structure after bleaching adversely affects the bonding strength of
resin composites to enamel and dentin. Therefore, waiting for at least 7
days after bleaching, prior to restoring the tooth with resin composites,
has been recommended.
Effects of the bleaching process
•
Teeth
•Bleaching occurs in an uneven manner.
•White spots or banding within the tooth may be noticeable.
•Pain and sensitivity of the teeth
•External Root Resorption
Tooth sensitivity is common side-effect of external
teeth bleaching. Teeth sensitivity normally persists
for up to 4 days but longer duration up to 39 days
has been reported
The sensitivity is due to the bleaching agent's
ability to easily penetrate through enamel, dentin
and even the pulp within minutes due to its acidic
properties, prolonged contact time and presence
of greater amounts of carbopol in bleaching
solutions
.
Teeth Sensitivity Following Bleaching
Management of Teeth Sensitivity
Passive approach include reductions in time or
frequency of application.
Active approach involves use of fluoride, Oxalates
agents or Potassium salts. mechanism of action
of Fluoride is occlusion of dentinal tubules or an
increase in enamel hardness.
Management of Teeth Sensitivity
Oxalate-containing products may interact with
dentine producing precipitates of calcium and
phosphate occlude dentinal tubules.
Potassium salts interfere with transmission of
pain stimulus at level of A-delta fibers around
odontoblast so block nerve conduction.

