Antimicrobial chemotherapy
chemotherapy as a science began in the first decade of the 20th century with understanding of the principles of selective toxicity, the specific chemical relationships between microbial pathogens and drugs, the development of drug resistance, and the role of combined therapy.Range of action of antibiotics
Antibiotics fall into 3 main categories :-a – action mainly against G+ve organisms like : penicillin , erythromycin & lincomycin .
b – action mainly against G-ve organisms like : polymyxin & nalidixic acid .
c – action against both G+ve & G-ve organisms ( broad spectrum activity ) like : ampicillin & ciprofloxacin .
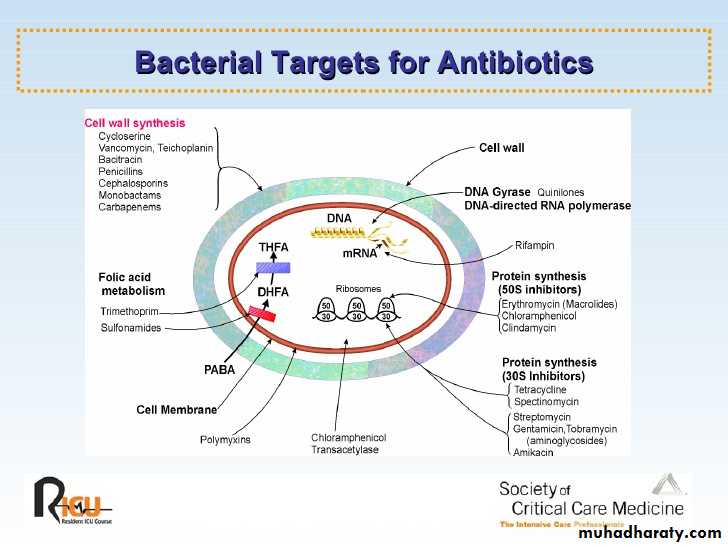
Mechanisms of action of chemotherapeutic agents
1 – Inhibition of cell wall synthesis :-
such as ß-lactams that include penicillins & cephalosporins interfere with cell wall synthesis and cause bacteriolysis .
2 – Inhibition of cytoplasmic membrane function :-
for example polymyxins.
3 – Inhibition of protein synthesis :-
such as : tetracyclines , erythromycin and aminoglycosides e.g. tobramycin & gentamycin .
4 – Inhibition of nucleic acid synthesis :-
Such as : quinolone , refampicin , novobiocin & sulfonamide . .
5 – Competitive inhibition :-
In which the drugs compete with an essential metabolite for the same enzyme e.g. Such as sulfonamide resemble to p – aminobenzoic acid ( PABA ) is an essential metabolite for DNA synthesis .
Mechanisms of resistance to antimicrobial agents
1 – The organism produced enzymes that destroy the drug e.g. production of ß – lactamases that destroy penicillin by penicillin resistant staphylococci & acetyltransferase which produced by gram negative bacilli destroy chloramphenecol .
2 – The organism change its permeability to the drug by modification of protein in the outer cell membranes , thus impairing its active transport into the cell e.g. resistance to polymyxins .
3 – The organism develop an altered receptor site for the drug e.g. resistance to aminoglycosides is associated with alteration of a specific protein in the 30s subunit of the bacterial ribosome that serve as a binding site in susceptible organisms .
4 – The organism develop an altered metabolic pathway that by passes the reaction inhibited by the drug e.g. sulfonamide-resistant bacteria acquire the ability to use performed folic acid with no need for extracellular PABA
Origin of resistance to antimicrobial agents
A – Non genetic drug resistance :- this include1 – Metabolic inactivity :- Most antimicrobial agents act effectively only on replicating cells , non multiplying organisms are phenotypically resistant to drugs such as M. tuberculosis which survive for years in tissues & their resistance is due to metabolic inactivity but if they start multiply after suppression of cellular immunity of the patient , they become susceptible to the drugs .
2 – Loss of target structure :- Protoplast or L-forms of bacteria are penicillin resistant because they lost their cell wall which is a structural target site of the drug .
3 – Bacteria may infect the host in the sites where antimicrobial are exclude or not active e.g. amino glycosides such as gentamycin are not effect in treating of enteric fever because of the Salmonellae are intracellular & aminoglycosides do not inter to the cells
B – Genetic drug resistance :- this include
1 – Plasmid mediated resistance :- Plasmid is an extra chromosomal genetic elements associated with bacterial resistance to antibiotics , plasmids frequently carry many genes that code for the production of enzymes that inactivate or destroy the antibiotics e.g. ß- lactamases which destroys the ß- lactam ring in penicillin & cephalosporin , plasmids may result in epidemic resistance among bacteria by moving from one to the other by conjugation.2 - Transposon-mediated resistance :- Many transposons carry genes that code for drug resistance , as they move between plasmids & chromosomes they can transfer this property to bacteria . the process called transposition .
3 – Chromosomal drug resisstance :- This develop as a result of spontaneous mutation in a genes that controls susceptibility to an antimicrobial agents
Complications of antibacterial chemotherapy
1 – Development of drug resistance
2 – Drug toxicity
3- super-infections
4 – Hypersensitivity