• Lec : 9
Mucogingival Surgery• UNIVERSITY OF MOSUL
• COLLEGE OF DENTISTRY
• By:
• Dr.Ghayath Aljawady
• B.D.S, M.Sc., Ph.D in periodontics
• 2020-2021
• Department of:
• Oral and Maxillofacial surgery / Periodontics unit
• Department of:
The term Mucogingival surgery was initially introduced in the literature by Friedman to describe surgical procedures for the correction of relationships between the gingiva and the oral mucous membrane, with special reference to three problem areas: attached gingiva, shallow vestibules, and a frenum interfering with the marginal gingiva.
The 1996 World Workshop in Clinical Periodontics renamed Mucogingival surgery as periodontal plastic surgery, a term originally proposed by Miller in 1993 and broadened to include the following areas:
Periodontal-prosthetic corrections.
Crown lengthening.
Ridge augmentation.
Aesthetic surgical corrections.
Coverage of the denuded root surface.
Reconstruction of papillae.
Aesthetic surgical correction around implants.
Surgical exposure of unerupted teeth for orthodontics
Periodontal plastic surgery is defined as the surgical procedures performed to correct or eliminate anatomic, developmental, or traumatic deformities of the gingiva or alveolar mucosa.
The periodontal plastic surgical techniques included in the traditional definition of Mucogingival surgery are:
(1) widening of attached gingiva,
(2) deepening of shallow vestibules, and
(3) resection of the aberrant frena.
Aesthetic surgical therapy for natural dentition and tissue engineering.
Objectives
Five objectives of periodontal plastic surgery are:1. Problems associated with attached gingiva.
2. Problems associated with a shallow vestibule
3. Problems associated with an aberrant frenum.
4. Aesthetic surgical therapy.
5. Tissue engineering.
Problems Associated With Attached Gingiva
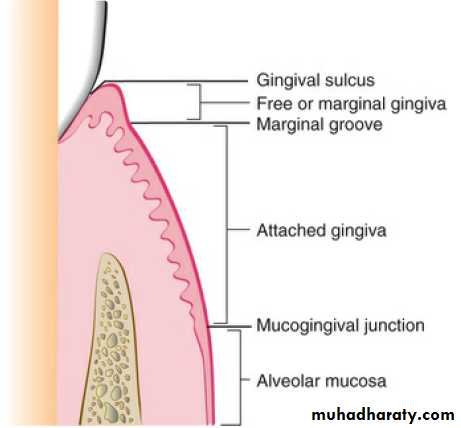
The ultimate goal of Mucogingival surgical procedures is the creation or widening of attached gingiva around teeth and implants.The width of the attached gingiva varies in different individuals and on different teeth of the same individual.
Attached gingiva is not synonymous with keratinized gingiva because the latter also includes the free gingival margin.
The width of the attached gingiva is determined by subtracting the depth of the sulcus or pocket from the distance between the crest of the gingival margin and the Mucogingival junction.
The original rationale for Mucogingival surgery was predicated on the assumption that a minimal width of attached gingiva was required to maintain optimal gingival health.
However, several studies have challenged the view that a wide, attached gingiva is more protective against the accumulation of biofilm than a narrow or a non existent zone.
No minimal width of attached gingiva has been established as a standard necessary for gingival health.
The maxillary anterior area, especially the facial aspect of the canine, often has extensive gingival recession.
In these cases, the covering of the denuded root surface widens the zone of attached gingiva and creates an improved aesthetic result.
Recession and the resultant denuded root surface have special aesthetic concerns for individuals with a high smile line.
A wider zone of attached gingiva is also needed around teeth that serve as abutments for fixed or removable partial dentures and in the ridge areas bearing a denture.
Widening the attached gingiva accomplishes four objectives:
1. Enhances plaque removal around the gingival margin.2. Improves aesthetics.
3. Reduces inflammation around restored teeth.
4. Allows gingival margin to bind better around teeth and implants with attached gingiva.
Problems Associated With a Shallow Vestibule
Another objective of periodontal plastic surgery is the creation of vestibular depth when it is lacking.Gingival recession displaces the gingival margin apically, reducing vestibular depth, which is measured from the gingival margin to the bottom of the vestibule. With minimal vestibular depth, proper hygiene procedures are reduced.
The sulcular brushing technique requires the placement of the toothbrush at the gingival margin, which may not be possible with reduced vestibular depth.
Minimal attached gingiva with adequate vestibular depth may not require surgical correction if proper a traumatic hygiene is practiced with a soft brush. Minimal amounts of keratinized attached gingiva with no vestibular depth benefit from Mucogingival correction. Adequate vestibular depth is also necessary for the proper placement of removable prostheses.
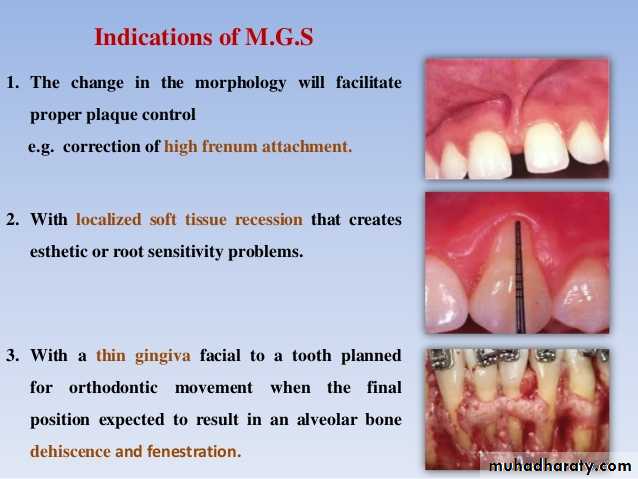
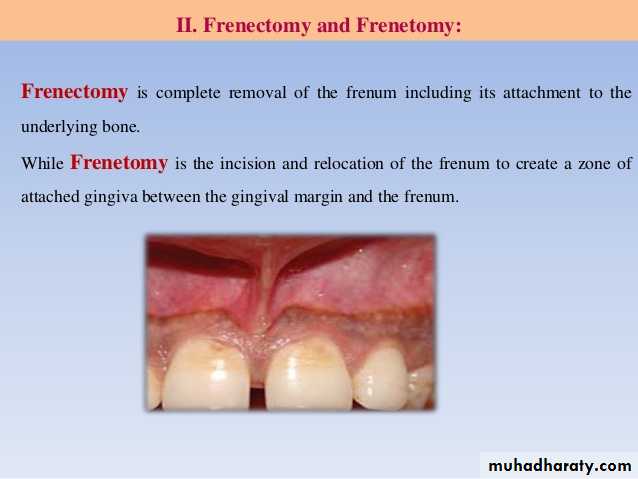
Problems Associated With an Aberrant Frenum
An important objective of periodontal plastic surgery is correction of frenal or muscle attachments that may extend coronal to the Mucogingival junction.If adequate keratinized, attached gingiva exists coronal to the frenum, it may not be necessary to remove the frenum.
A frenum that encroaches on the margin of the gingiva can interfere with biofilm removal, and the tension on the frenum tends to open the sulcus. In these cases, surgical removal of the frenum is indicated.
Aesthetic Surgical Therapy
Recession of the facial gingival margin alters the proper gingival symmetry and results in an aesthetic problem.The interdental papilla is also important to satisfy the aesthetic goals of the patient. A missing papilla creates a space that many call a black hole. Regeneration of the lost or reduced papilla is one of the most difficult goals in aesthetic periodontal plastic surgery.
Another area of concern is an excessive amount of gingiva in the visible area. This condition is often called as a gummy smile, and it can be corrected surgically by crown lengthening.
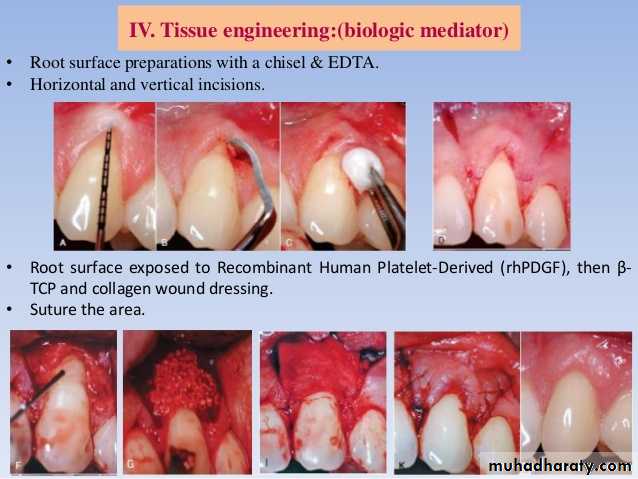
Tissue Engineering
The future of periodontal plastic surgery will encompass the use of tissue-engineered products at the recipient site to reduce donor site morbidity.Results of numerous experimental and clinical studies support the clinician's use of a minimally invasive approach to periodontal plastic surgery.
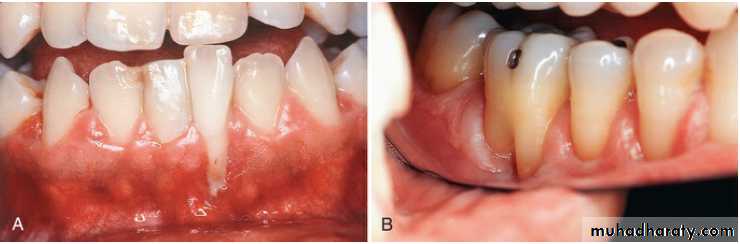
Cause of Marginal Tissue Recession
The most common cause of gingival recession and the loss of attached gingiva is abrasive and traumatic tooth brushing habits. The bone and soft tissue anatomy of the facial, radicular surface of the dentition is usually thin, especially around the anterior area. Teeth positioned facially may have an even thinner bone and gingiva.In many instances, the areas have a complete absence of bone beneath the thin overlying gingival tissue. This defect in the bone is called a dehiscence. This anatomic status combined with external trauma from aggressive brushing can lead to the loss of gingival tissue.
Recession of the gingival tissue and bone exposes the cemental surface of the root, which results in abrasion and ditching of the cemental surface apical to the cement enamel junction (CEJ).
The Cementum is softer than enamel and is destroyed before the enamel surface of the crown.
Another cause of gingival recession is periodontal disease and chronic marginal inflammation. The loss of attachment caused by the inflammation is followed by the loss of bone and gingiva.
Advanced periodontal involvement in areas of minimally attached gingiva results in the base of the pocket extending close to or apical to the Mucogingival junction. Periodontal therapy for these areas results in gingival recession caused by the loss of gingiva and bone.
Frenal and muscle attachments that encroach on the marginal gingiva can distend the gingival sulcus, which creates an environment for biofilm accumulation.
This condition increases the rate of periodontal recession and contributes to the recurrence of recession, even after treatment.
These problems are more common on facial surfaces, but they may also occur on the lingual surface.
Orthodontic tooth movement through a thin buccal osseous plate may lead to a dehiscence beneath a thin gingiva. This situation can also lead to the recession of the gingival margin.
Factors That Affect Surgical Outcome
1. Irregularity of Teeth:Abnormal tooth alignment is an important cause of gingival deformities that require corrective surgery and an important factor in determining the outcome of treatment.
Location of the gingival margin, width of the attached gingiva, and alveolar bone height and thickness are affected by tooth alignment.
On teeth that are tilted or rotated labially, the labial bony plate is thinner and located further apically than on the adjacent teeth.
On the lingual surface of these teeth, the gingiva is thick, and the bone margins are closer to the CEJ.
Orthodontic correction is indicated when Mucogingival surgery is performed on malposed teeth in an attempt to widen the attached gingiva or to restore the gingiva over denuded roots.
2. Mucogingival Line (Junction):
Normally, the Mucogingival line in the incisor and canine areas is located approximately 3 mm apical to the crest of the alveolar bone on the radicular surfaces and 5 mm interdentally. In periodontal disease and on malposed, disease-free teeth, the bone margin is located further apically and may extend beyond the Mucogingival line.The distance between the Mucogingival line and the CEJ before and after periodontal surgery is not necessarily constant. After inflammation is eliminated, the tissue tends to contract and draw the Mucogingival line in the direction of the crown.
Criteria for Selection of Techniques
The following criteria are used for selection of Mucogingival techniques:1. Surgical site free of biofilm, calculus, and inflammation.
2. Adequate blood supply to the donor tissue
3. Anatomy of the recipient and donor sites
4. Stability of the grafted tissue to the recipient site.
5. Minimal trauma to the surgical site.
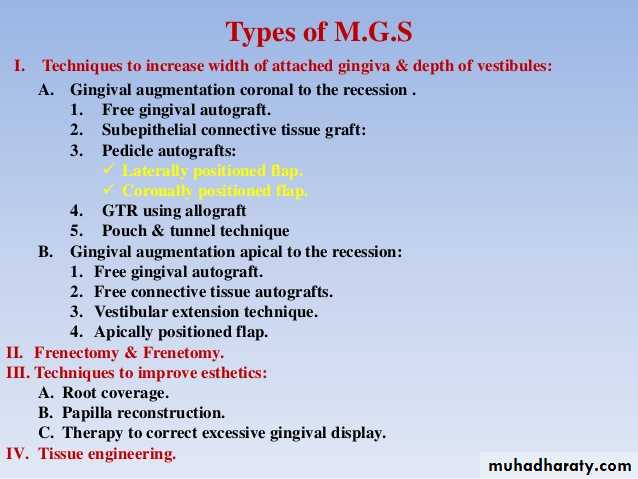
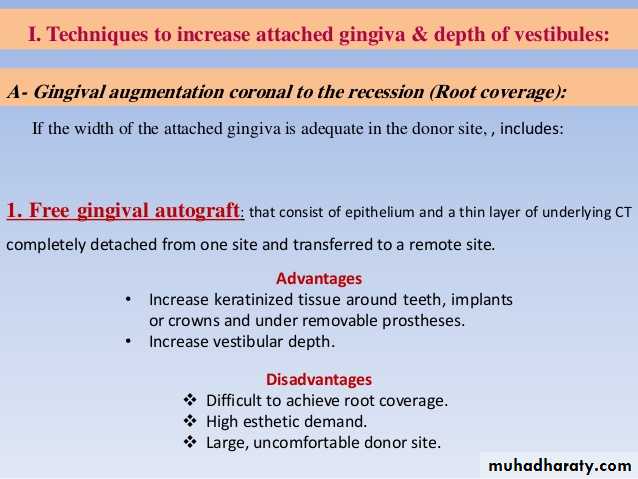
Techniques to Increase Attached Gingiva
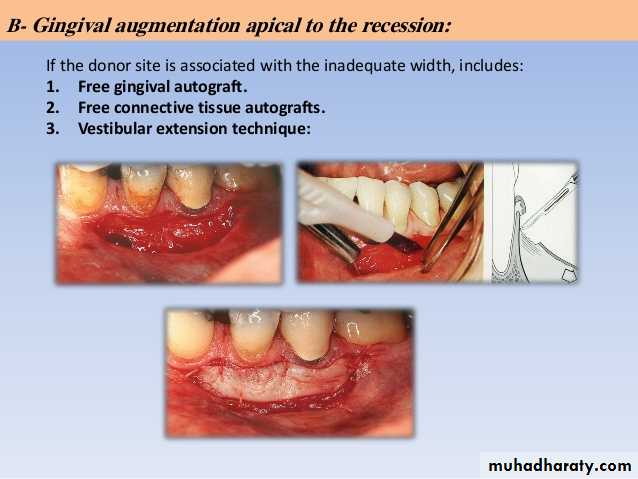
To simplify and better understand the techniques and the result of the surgery, the following classifications are presented:Gingival augmentation apical to the area of recession. The donor graft tissue (i.e., pedicle or free) is placed on a recipient bed apical to the recessed gingival margin.
Gingival augmentation coronal to the recession (i.e., root coverage). The donor graft tissue (i.e., pedicle or free) is placed covering the denuded root surface.
Gingival Augmentation Coronal to Recession
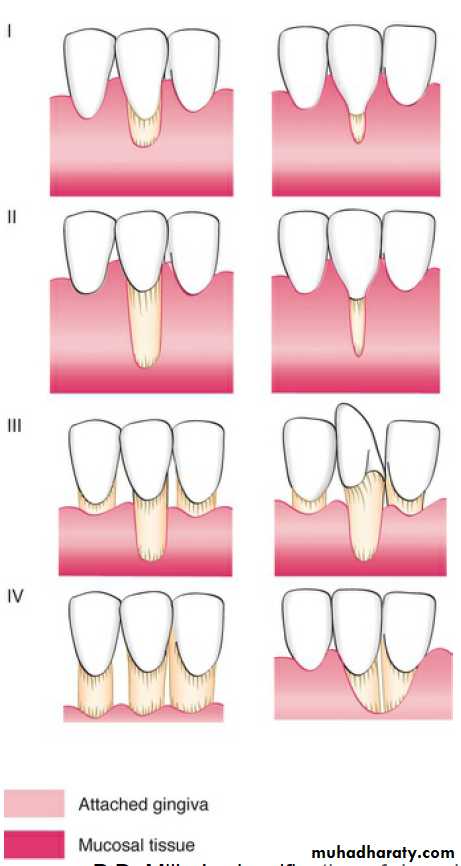
Understanding the different stages and conditions of gingival recession is necessary for predictable root coverage. Several classifications of denuded roots have been proposed.The predictability of root coverage can be enhanced by the pre surgical examination and the correlation of the recession by using the classification proposed by Miller, as follows:
Class I.:
Class II.:Class III.:
Class IV. :
Several techniques are used for gingival augmentation coronal to recession (i.e., root coverage):
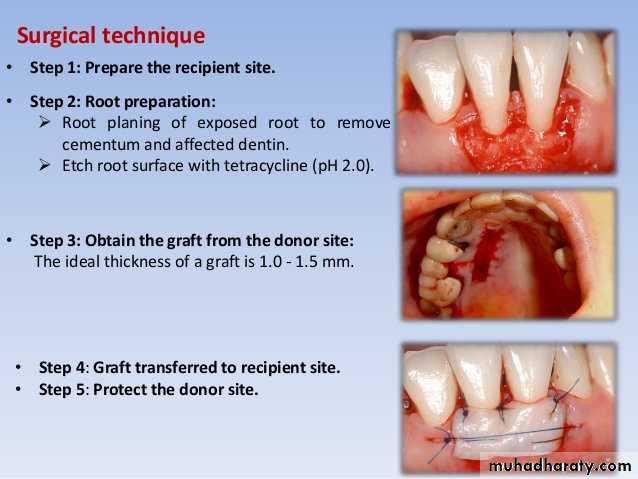
1. Free gingival autograft.
2. Free connective tissue autograft.
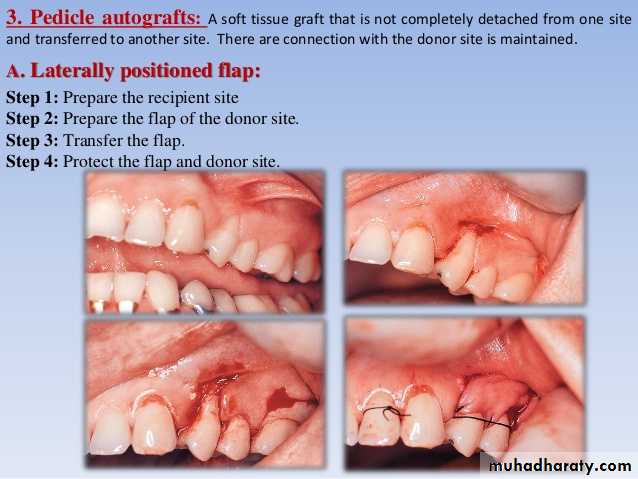
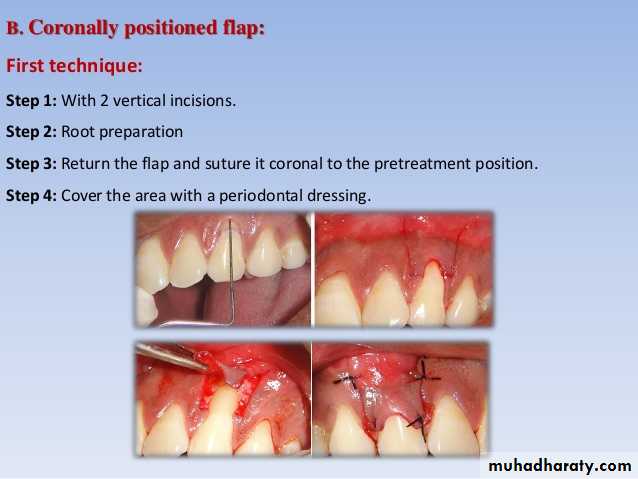
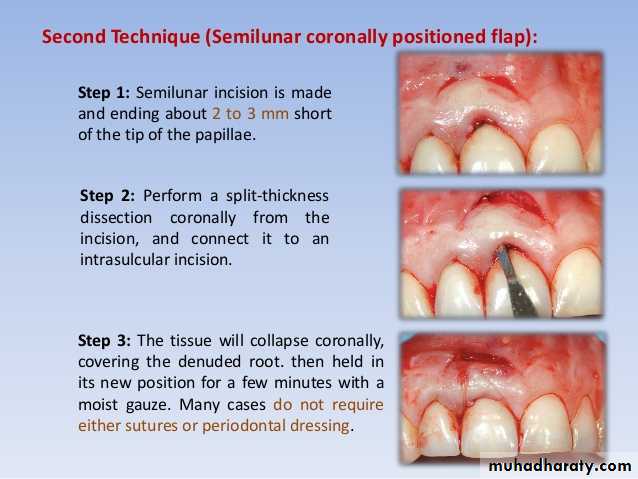
3. Pedicle autografts:
• Laterally (horizontally) positioned pedicle flap
• Coronally positioned flap; includes semilunar pedicle (i.e., Tarnow method)
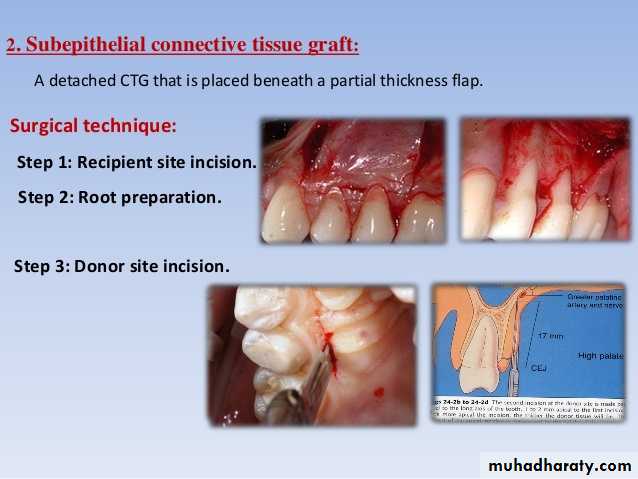
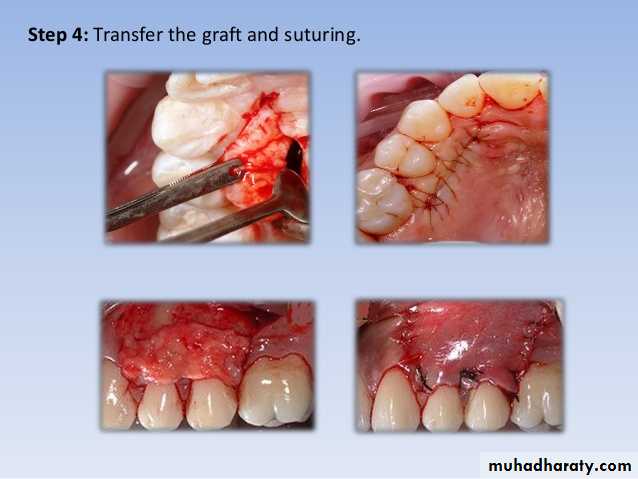
4. Subepithelial connective tissue graft (i.e., Langer method)
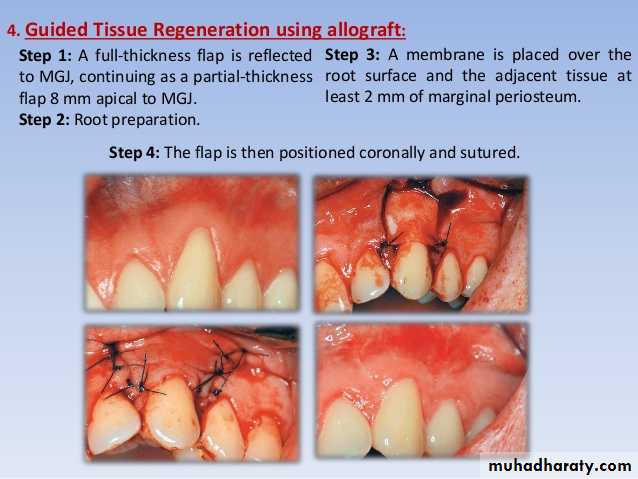
5. Guided tissue regeneration (GTR).
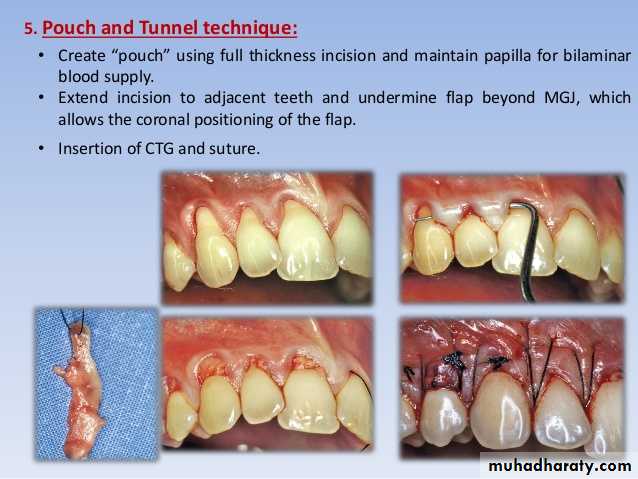
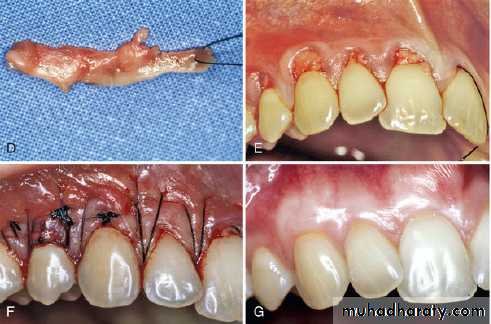
6. Pouch and tunnel technique (i.e., coronally advanced tunnel technique).
ΙΙΙ-Techniques to Improve Aesthetics
The maxillary anterior area in a patient with a high lip line may cause concerns about the aesthetic appearance of gingival tissues.This area is called the aesthetic zone, and it requires special consideration in restorative, periodontal, and implant therapy.
Therapy to correct these gingival conditions is discussed under the topics of root coverage, papilla reconstruction, and correction of excessive gingival display.
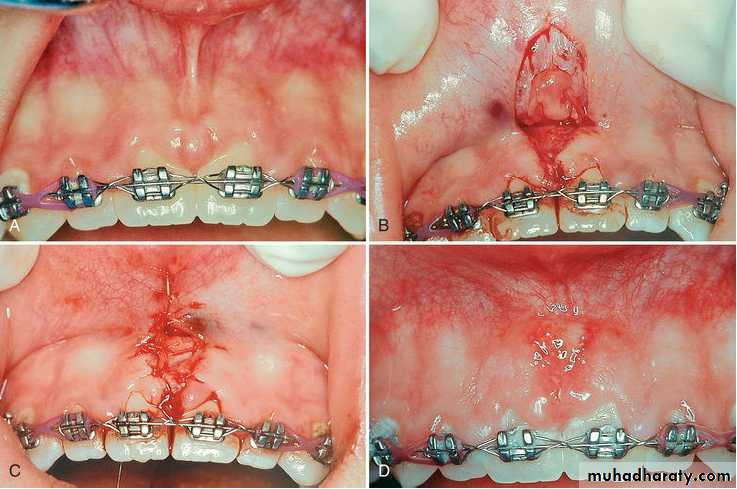
Papilla Reconstruction:
Loss of the interdental papilla is a major aesthetic problem for many patients. It is often referred to as the black triangle or hole.Reconstruction of the lost or reduced interdental papilla is the most difficult and unpredictable problem in aesthetic periodontal therapy.
The predictable reconstruction of the papilla is determined by augmentation of the gingival tissue, the presence or absence of the underlying bone, and contact of the two adjacent teeth.
All techniques must be based on the principle of adequate blood supply to the donor tissue. Of the many gingival grafting procedures used in periodontal therapy, the technique that offers the best blood supply to the donor tissue is the pedicle graft because it maintains a connection between the donor tissue and the origin of the graft.