• Synapse & Neurotransmission
• Lecture 2• Dr. Suroor Mohamed
Synapses – specialized junction where an axon terminal contacts another neuron or cell type , by which excitable cells communicate with one another where information is transmitted from between them. As Nerve to nerve synapse, nerve to muscle - neuromuscular junction, and nerve to gland - neuroglandular junction
synapse: is the functional connection between a neuron and a second cell . In the CNS, this other cell is also neuron In the PNS, the other cell may be either a neuron or an effecter cell within a muscle or gland.
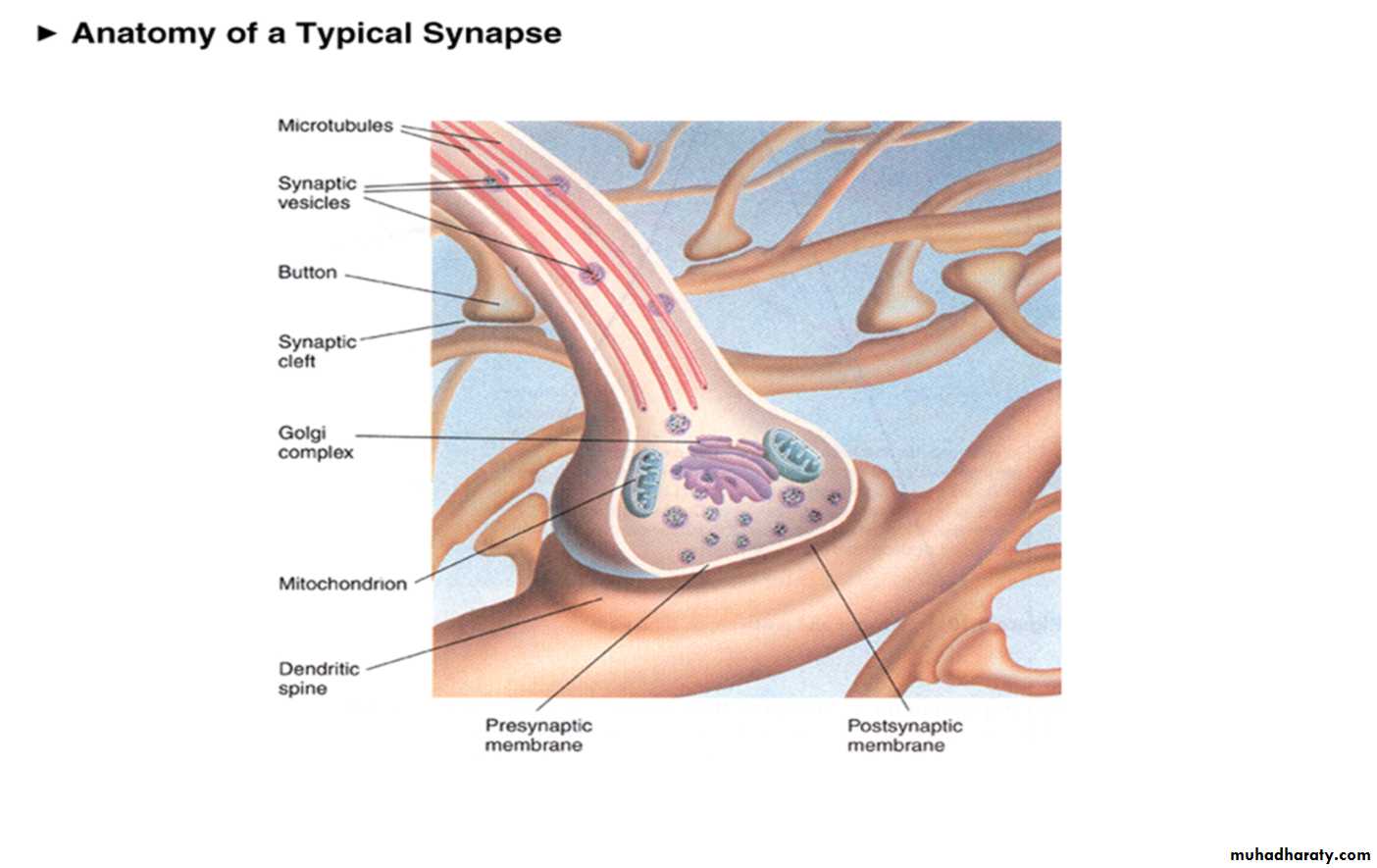
What are the components of a synapse ?
Synaptic knob of the pre-synaptic cell ( contains transmitter )(2) Synaptic cleft (space ) contains enzyme that destroys the transmitter
(3) Post-synaptic membrane ( contains receptors for the transmitter )
There are two general types of synapses
Electrical Synapses (Gap Junctions)
Chemical Synapses (Neurological)
Types of Synapses Electrical Synapses
Electrical synapses allow current to flow from one excitable cell to the next via low resistance pathways between the cells called gap junctions which are account for the very fast conduction in these tissues. Like in cardiac ventricular muscle, in the uterus, and in the bladder, allowing cells in these tissues to be activated simultaneously and ensuring that contraction occurs in a coordinated manner.
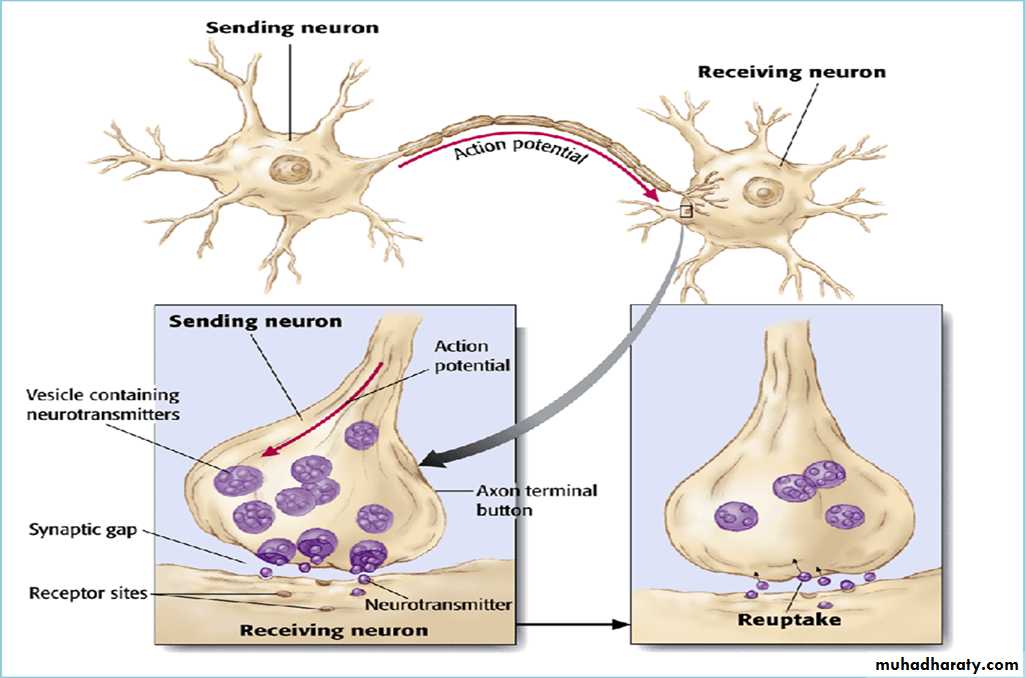
Chemical Synapses Transmission across the majority of synapses in the nervous system is one-way, and occurs through the release of chemical neurotransmitters from pre synaptic cells. There is a gap between the presynaptic cell membrane and the postsynaptic cell membrane, known as the synaptic cleft.
Information is transmitted across the synaptic cleft via a neurotransmitter, a substance that is released from the presynaptic terminal and binds to receptors on the postsynaptic terminal.
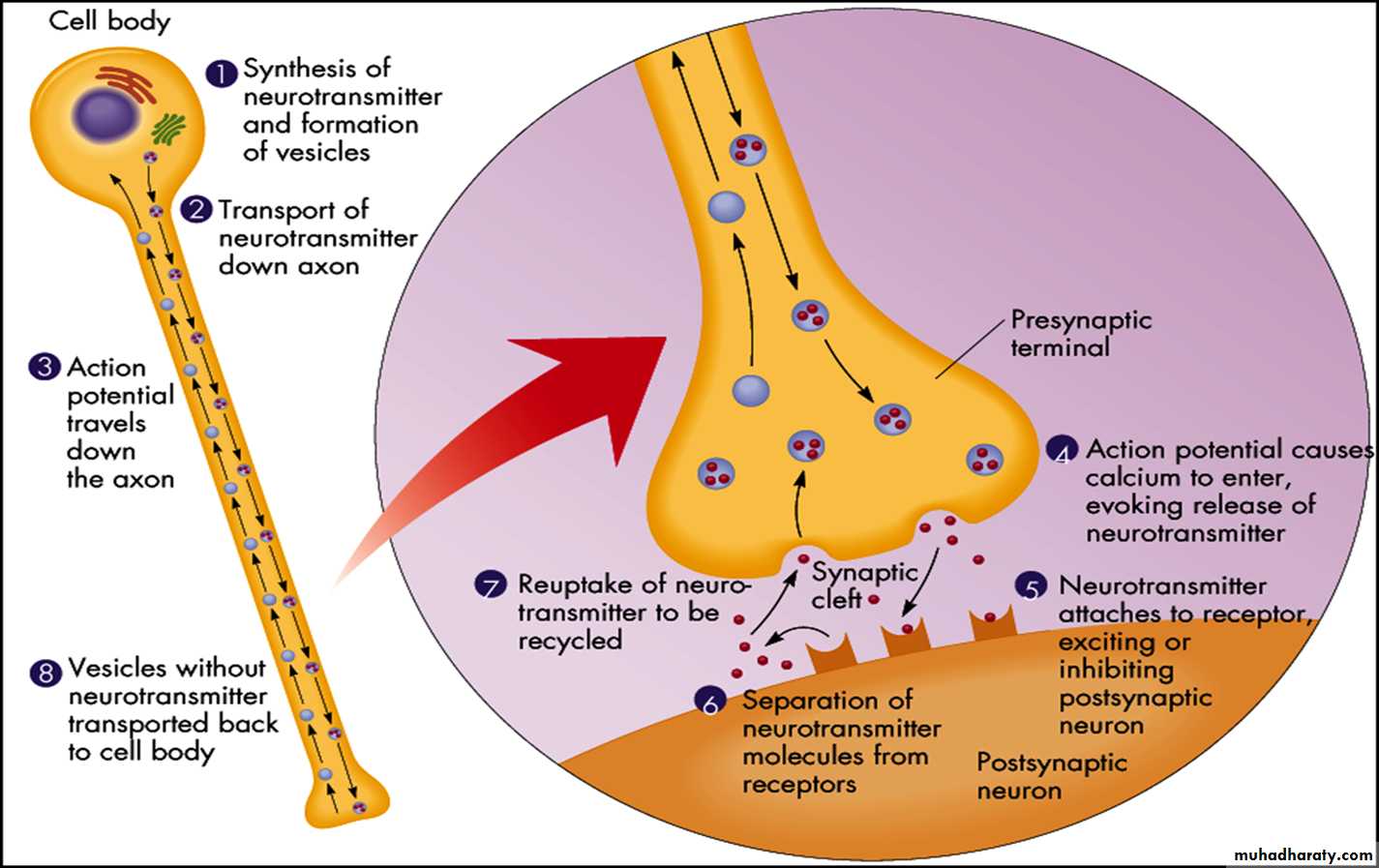
The following sequence of events occurs at chemical synapses:
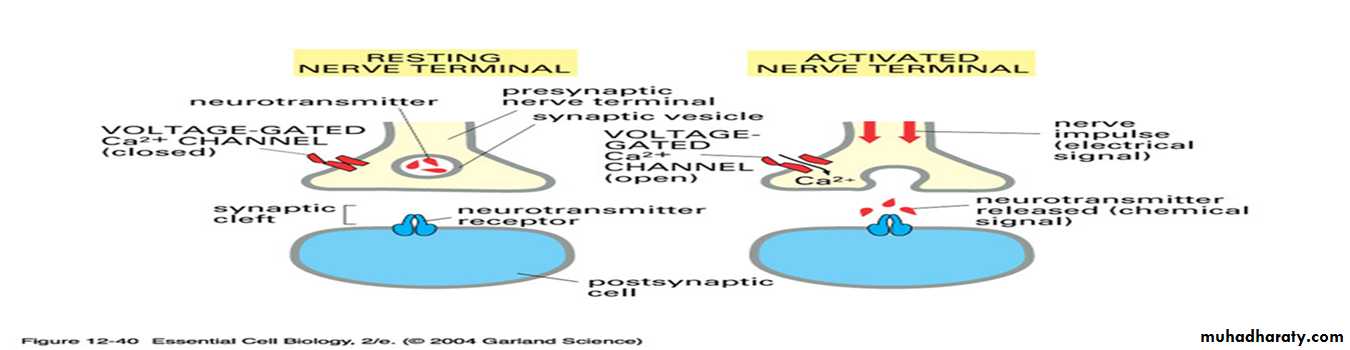
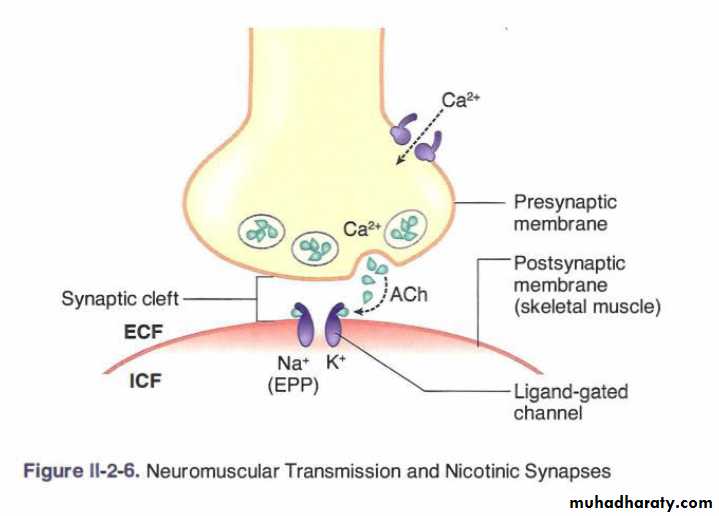
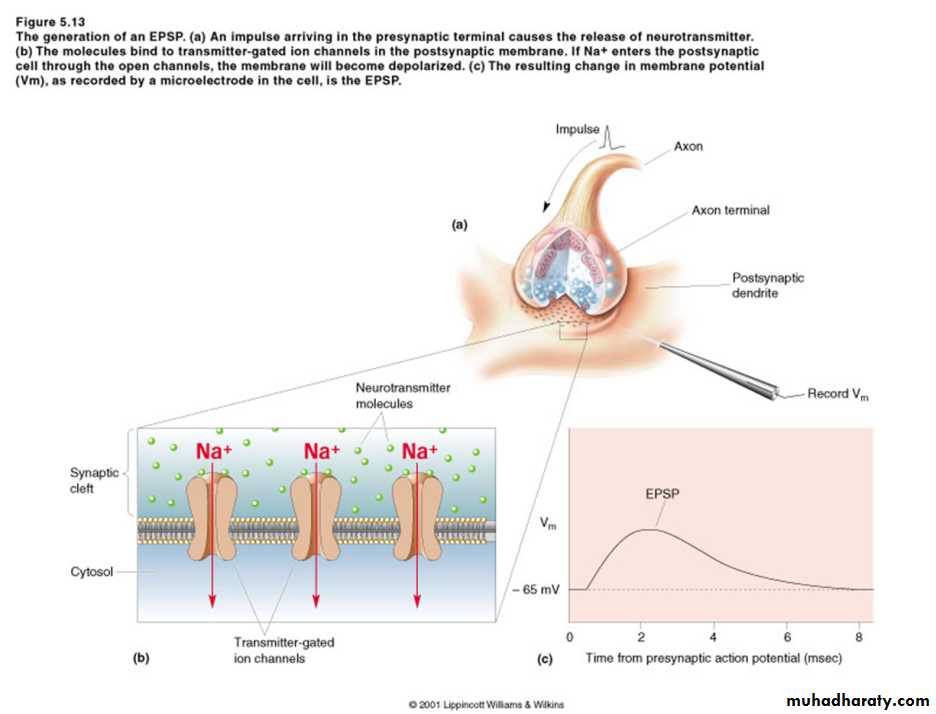
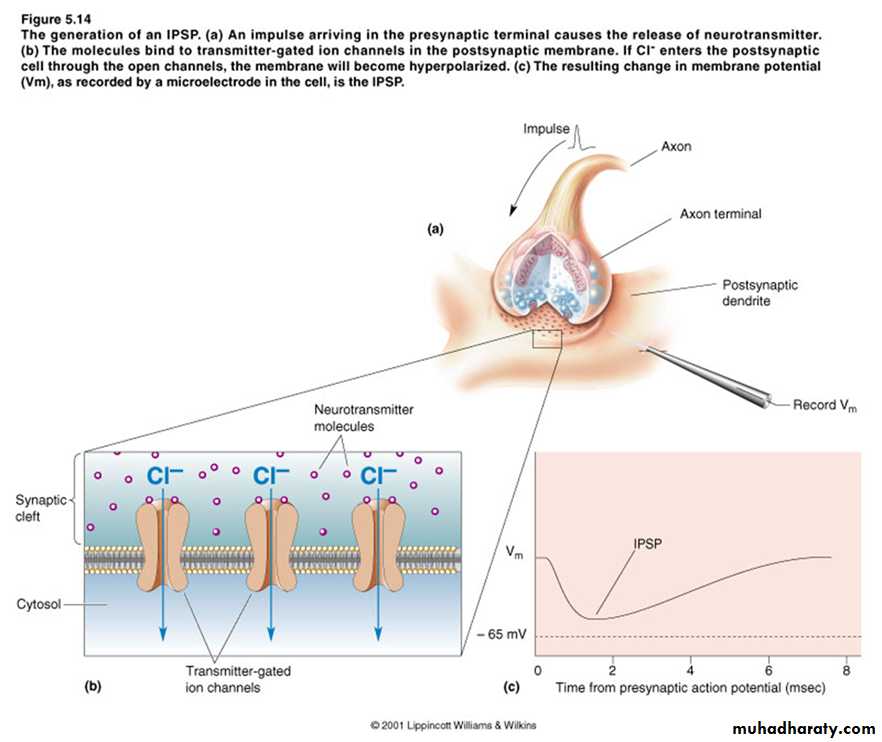
An action potential in the presynaptic cell causes Ca2+ channels to open. An influx of Ca2+ into the presynaptic terminal causes the neurotransmitter, which is stored in synaptic vesicles, to be released by exocytosis. The neurotransmitter diffuses across the synaptic cleft, binds to receptors on the postsynaptic membrane, and produces a change in membrane potential on the postsynaptic cell. The change in membrane potential on the postsynaptic cell membrane can be either excitatory or inhibitory, depending on the nature of the neurotransmitter released from the presynaptic nerve terminal. Opening of ion channels often produces either depolarization the inside of the post synaptic membrane called( excitatory post synaptic potential)(EPSP). In other cases, causing hyper polarization inside the post synaptic membrane( more negative) called inhibitory post synaptic potential(IPSP).If the neurotransmitter is excitatory, it causes depolarization of the postsynaptic cell;
if the neurotransmitter is inhibitory, it causes hyperpolarization of the postsynaptic cell.
**In contrast to electrical synapses, neurotransmission across chemical synapses is unidirectional (from presynaptic cell to postsynaptic cell).
Response of the postsynaptic neuron?
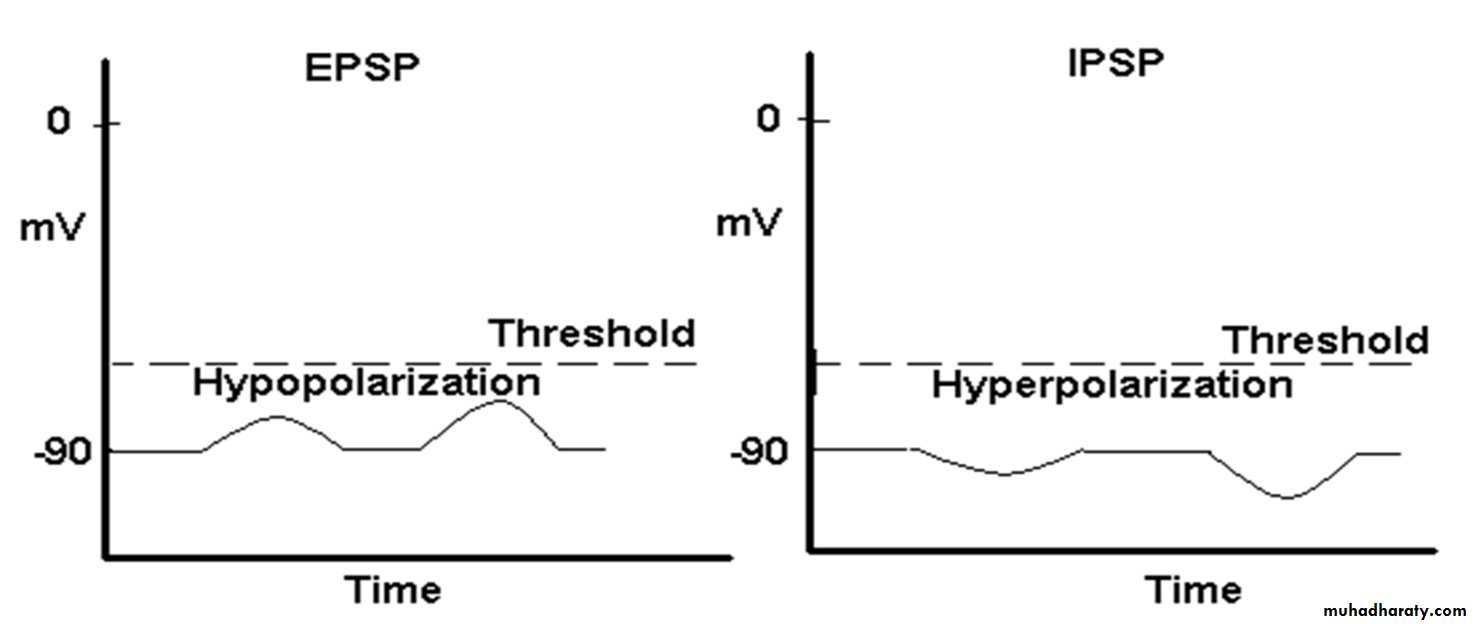
If the membrane potential is depolarized and brought closer or to threshold, then it is called an Excitatory PostSynaptic Potential (EPSP). For example, if Na+ ions enter the cell - the inside of the cell becomes more positive, and the RMP of -70 mV gets moved closer to threshold (-55 mV).If the membrane potential is hyperpolarized and moved further away from threshold, then it is called an Inhibitory PostSynaptic Potential (IPSP). For example, if K+ ions leave or CI- ions enter the cell, the inside becomes more negative, and the RMP of -70 mV gets moved further away from threshold, making the cell less likely to reach threshold.
• Synaptic Input—Excitatory and Inhibitory Postsynaptic Potentials
• The inputs being either excitatory or inhibitory , if the sum of the inputs is sufficient to bring the postsynaptic cell to threshold, it will then fire an action potential.
Excitatory Postsynaptic Potentials (EPSPs) are synaptic inputs that depolarize the postsynaptic cell, bringing the membrane potential closer to threshold and closer to firing an action potential. EPSPs are produced by opening Na+ and K+ channels, similar to the nicotinic ACh receptor. The membrane potential is driven to a value approximately halfway between the equilibrium potentials for Na+ and K+, or 0 mV, which is a depolarized state.
• Excitatory neurotransmitters include ACh, norepinephrine, epinephrine, dopamine, glutamate, and serotonin.
Inhibitory Postsynaptic Potentials (IPSPs) are synaptic inputs that hyperpolarize the postsynaptic cell, taking the membrane potential away from threshold and farther from firing an action potential. IPSPs are produced by opening Cl− channels. The membrane potential is driven toward the Cl− equilibrium potential (approximately −90 mV), which is a hyperpolarized state.
Inhibitory neurotransmitters are γ-aminobutyric acid (GABA) and glycine.
AP ACTION OTENTIAL is NOT produced at the synapse ?
a. change in membrane potential is conducted electronically (local graded response) across the somab. membrane threshold is lower at axon hillock
c. AP will be generated IF the sum of all inputs to the cell causes the membrane potential to reach threshold
Neurotransmitter
Neurotransmitters are signal molecules that are released from neurons depending on the location of neuron and type of effector (target) cell it acts on , that s allow the transmission of signals from one neuron to the next across synapses
They are also found at the axon endings of motor neurons, where they stimulate the muscle fibers.
Neurotransmitters function by changing the permeability of the cell membrane to various ions such as sodium and potassium. If an excess of sodium ions flow into the nerve cell, an impulse is generated. If an excess of potassium ions flow out, the impulse is inhibited.
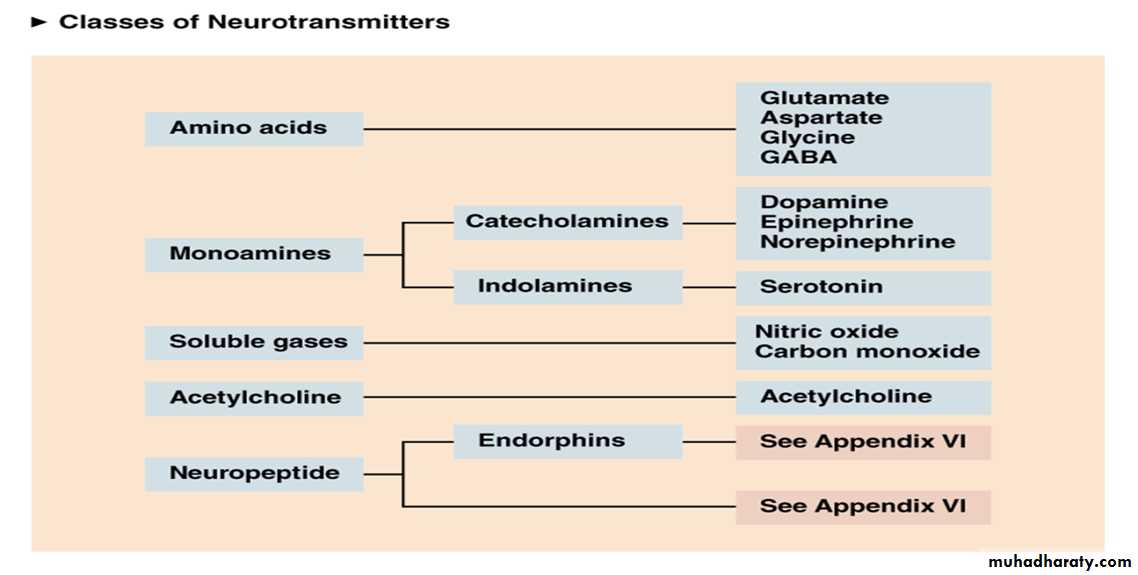
Neurotransmitters are divided into two groups depending on the rate of action
A. Small-molecule - rapidly acting transmitters (usually open ion channels)1. Acetylcholine
2. Amines
3. Amino acids
4. NO
B. Neuropeptides - action is slow (usually act on DNA or through second messenger systems) - Released in very small quantities but effect is very potent
1. Opioids
2. peptides
3. Hypothalamic and pituitary peptides
The following criteria are used to formally designate a substance as a neurotransmitter:
The substance must be synthesized in the presynaptic cell; the substance must be released by the presynaptic cell on stimulation; and, if the substance is applied exogenously to the postsynaptic membrane at physiologic concentration, the response of the postsynaptic cell must mimic the in vivo response.Fate of released neurotransmitters
a. Neuropeptides - diffusion and enzymatic hydrolysis
b. Small molecule transmitters
1) diffusion
2) enzymatic hydrolysis
3) re-uptake into the presynaptic terminal
4) Bind to receptor than degradation (enzymatic hydrolysis)
A) Excitatory NT
1) Glutamate - accounts for approximately 75% of all excitatory transmission in the brain, so it is the most common excitatory NT in the brain. It is released in cerebral cortex, brain stem. Involved in learning and memory. Also called glutamic acid.2) Aspartate - similar to glutamate but found mostly in the spinal cord for excitation. (aspartic acid)
B) Inhibitory NT
3) GABA - Gamma AminoButyric Acid (GABA) is the most common inhibitory NT in the brain. Released in thalamus, hypothalamus, cerebellum, occipital lobe and retina.4) Glycine - is the simplest amino acid and is the most common inhibitory NT in the spinal cord. It is also released in the brain and retina.
Acetylcholine was the first neurotransmitter to be discovered.
It is responsible for much of the stimulation of muscles, including the muscles of the gastro-intestinal system.It is also found in sensory neurons and in the autonomic nervous system, and has a part in scheduling REM (dream) sleep.
Acetylcholine is transmitted within cholinergic pathways that are concentrated mainly in specific regions of the brainstem and are thought to be involved in cognitive functions, especially memory. Severe damage to these pathways is the probable cause of Alzheimer’s disease.
The plant poisons curare cause paralysis by blocking the acetylcholine receptor sites of muscle cells. The well-known poison botulin works by preventing the vesicles in the axon ending from releasing acetylcholine, causing paralysis.
ACh binds to two types of receptors, 1) nicotinic and 2) muscarinic.
In the PNS, ACh is the sole NT used by the Somatic nervous system (SNS): at the NMJ ACh binds to nicotinic receptors on skeletal muscle and causes excitation (contraction) of skeletal muscle.
In the Autonomic nervous system (ANS), it is release by all neurons at the ganglia and binds to nicotinic receptors on postgalionic neurons. It is also released by parasympathetic postgalionic neurons and binds with muscarinic receptors on effector tissue (cardiac muscle, smooth muscle and glands).
In general terms, nicotinic receptors are always excitatory (in that when stimulated they cause an EPSP) and muscarinic receptors are generally inhibitory (in that when stimulated they usually cause an IPSP).
Botox = a neurotoxin produced by a bacterium Chlostridium botuninum , It causes food poisoning (botulism)
The toxin blocks the release of acetyl choline neurotransmitter to muscles , Causes muscle paralysis
Cosmetically used to smooth lines and creases
Medically used to relax muscles that causing illnesses such as spasms and strabismus (cross-eyed).
Botulinum toxin binds to pre-synaptic membranes at neuromuscular junctions, enters the neuron, and then a component of the toxin interferes with the release of neurotransmitter.Release of acetylcholine is blocked.
No acetylcholine? No muscular contraction. (flaccid paralysis)
after botox
Muscles physiologyThere are three types of muscle tissues in the body:
1. skeletal muscle: Located throughout the body connected to bones
and joints, striated in appearance, under somatic nervous control.2. smooth muscle or visceral muscle: Located in the walls of organs,
no striations, under involuntary or autonomic nervous control.3. cardiac muscle: Located only in the heart, striated in appearance,
under involuntary or autonomic nervous control.
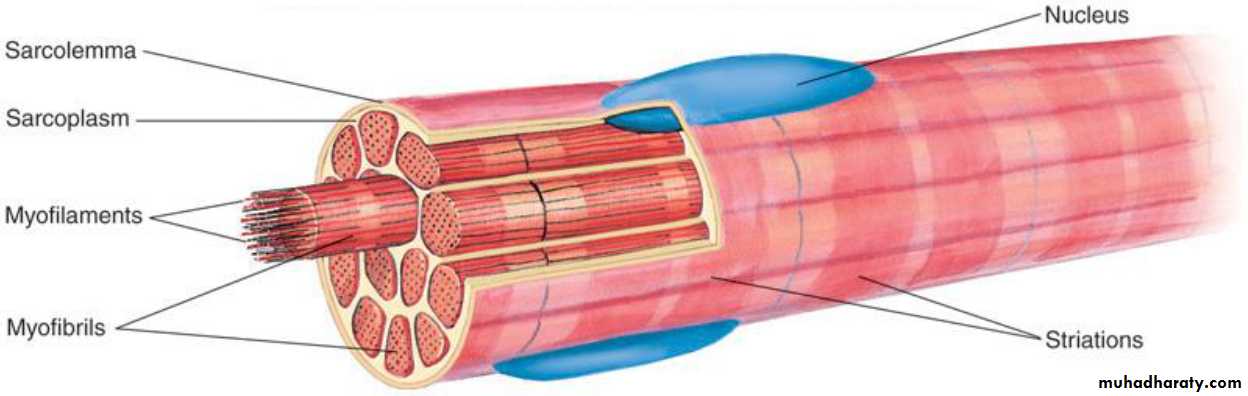
All muscle tissues consist of elongated cells called fibers.
The cytoplasm of muscle cells is called sarcoplasm and the
surrounding cell membrane or plasma lemma is called sarcolemma.
Each muscle fiber sarcoplasm contains numerous myofibrils, which
contain two types of contractile protein filaments, actin and myosin
Skeletal muscles
About 40% of the body mass is skeletal muscle, and perhaps another 10%is smooth muscle and cardiac muscle. Many of the principles of
contraction apply to all three types of muscle.
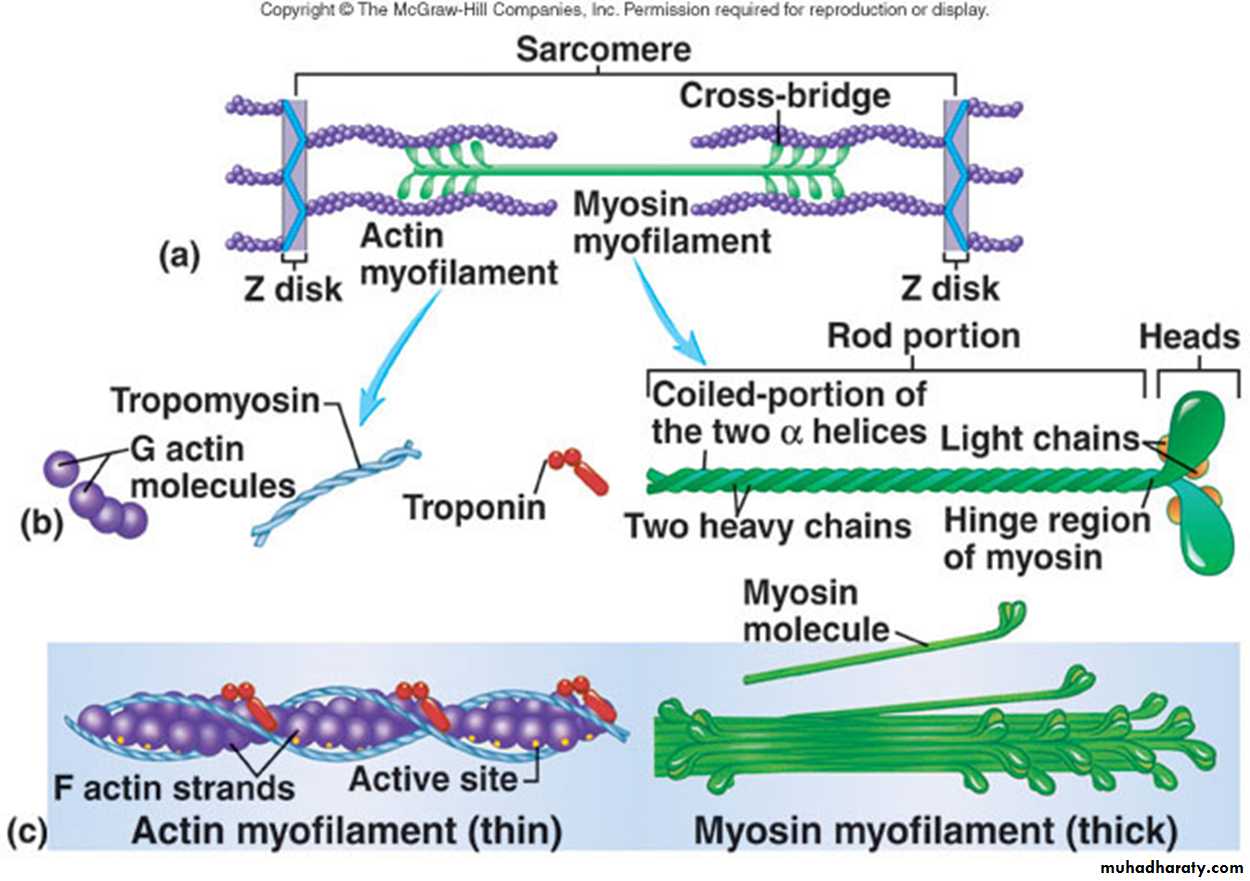
Skeletal muscle fibers are long, cylindrical ,multinucleated cells ,with
peripheral nuclei. Each muscle fiber is composed of subunits called
myofibrils that extend the length of the fiber. each myofibril is composed
of about 1500 myosin filaments and 3000 actin filaments lying side by
side. These filaments are large polymerized protein molecules that are
responsible for muscle contraction. the thick filaments are myosin, and
the thin filaments are actin; note the following features:
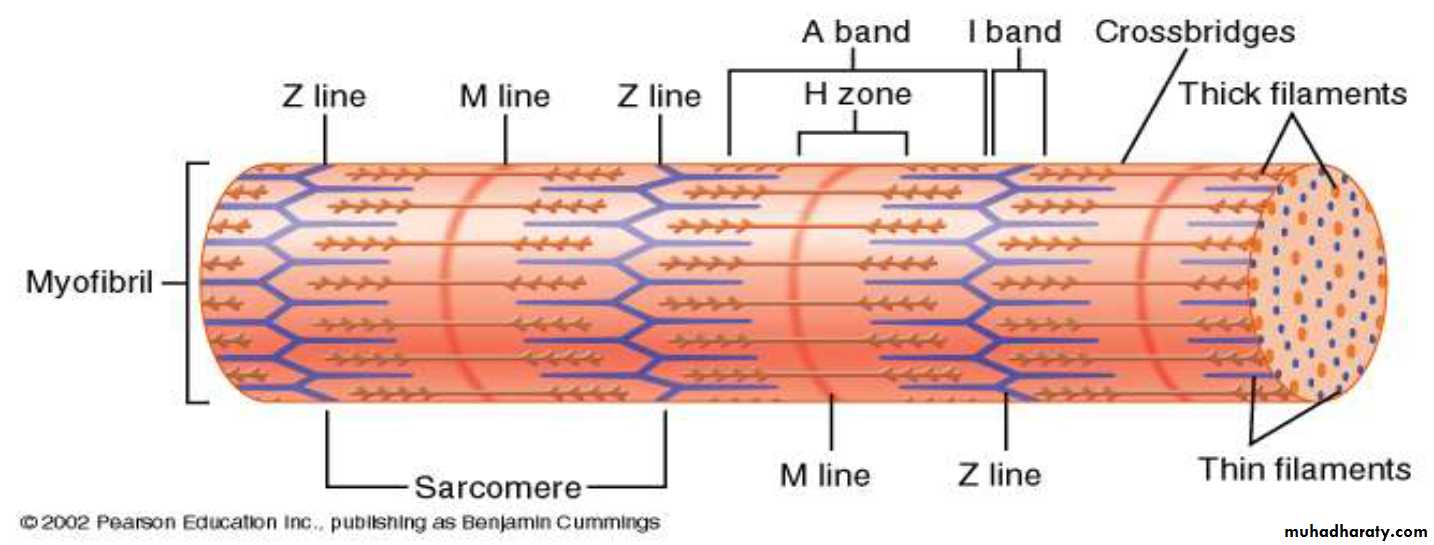
•Light and dark bands. The myosin and actin filaments partially inter
digitate and thus cause the myofibrils to have alternate light and dark
bands. The light bands contain only actin filaments and are called I
bands. The dark bands called A bands contain myosin filaments as well
as the ends of the actin filaments. The length of the A band is the length
of the myosin filament.
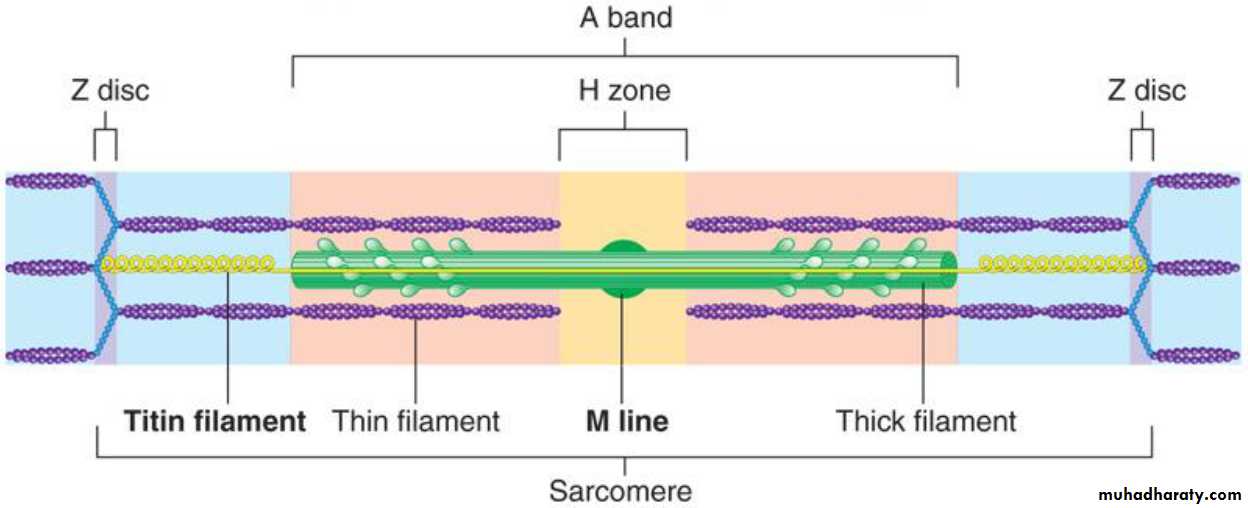
•Cross-bridges. The small projections from the sides of the myosin filaments are cross-bridges. They protrude from the surfaces of the myosin filament along its entire length except in the center. Myosin crossbridges interact with actin filaments causing contraction.
•Z disc. The ends of the actin filaments are attached to Z discs .The Z disc passes across the myofibril and from one to another, attaching and aligning the myofibrils across the muscle fiber. The entire muscle fiber therefore has light and dark bands, giving skeletal and cardiac muscle astriated appearance
Sarcomere. The portion of a myofibril that lies between two successive Z discs is called a sarcomere..
Z lines: boundary of the sarcomere.
I Band: region of only actin myofilaments.
H Zone: region of only myosin myofilaments.
A Band: region of both actin and myosin.
M-Line: The exact midpoint of the sarcomere.
Myofilaments are arranged in sarcomeres
•Sarcomeres are contractile units of skeletal muscle consisting of the components between 2 Z discs•Myofibrils are a single file line of repeating sarcomeres
A band is dark area, contains thick myofilaments
–Light area at center of A band is H zone ( area where there are no thin myofilaments)
•I band is light area, only contains thin myofilaments
–At center of I band is Z line/disc where thin myofilaments attach
The Myosin Filament Is Composed of Multiple Myosin Molecules. The
tails of myosin molecules bundle together to form the body of thefilament, whereas the myosin heads and part of each myosin molecule
hang outward to the sides of the body, providing an arm that extends the
head outward from the body.
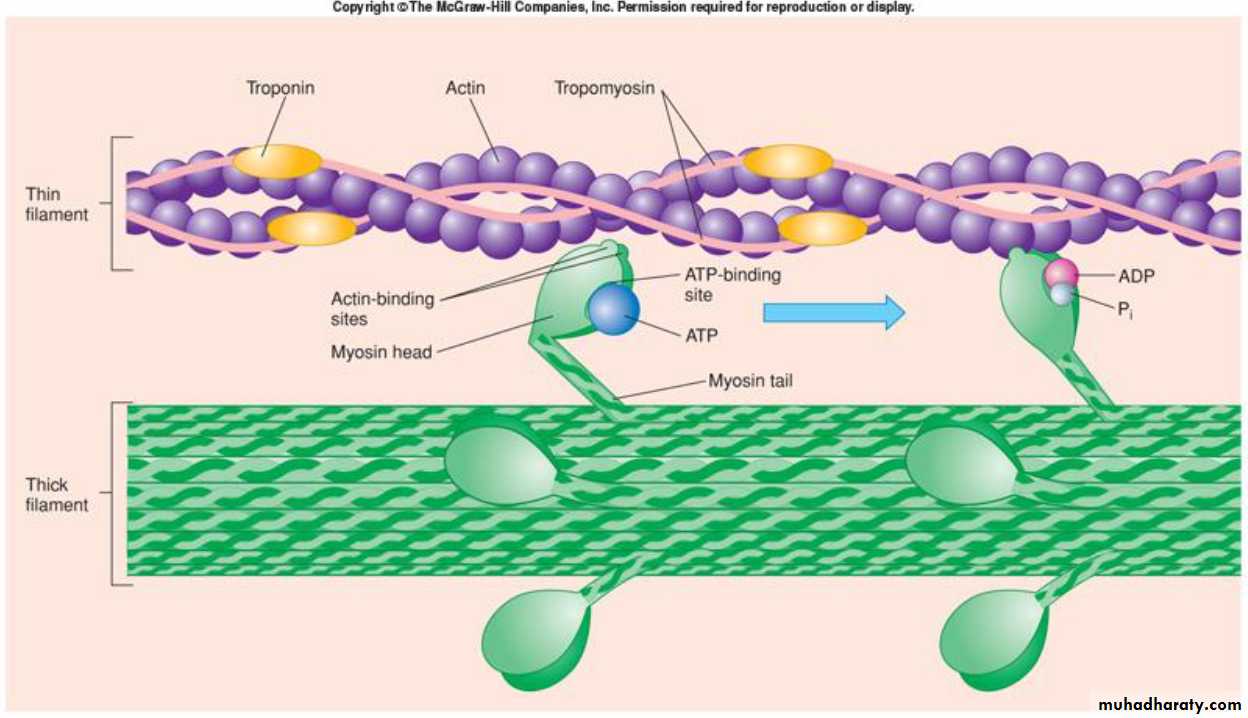
The protruding arms and heads together are called cross-bridges. An
important feature of the myosin head is that it functions as an adenosine
triphosphatase (ATPase) enzyme, which allows it to cleave adenosine
triphosphate (ATP) and thus energize the contraction process
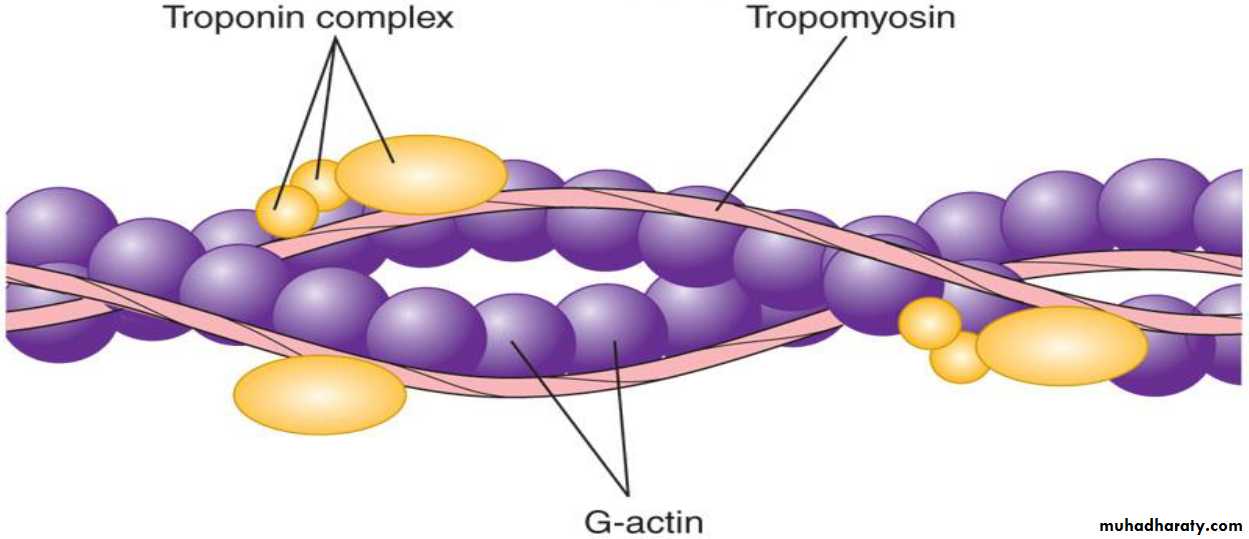
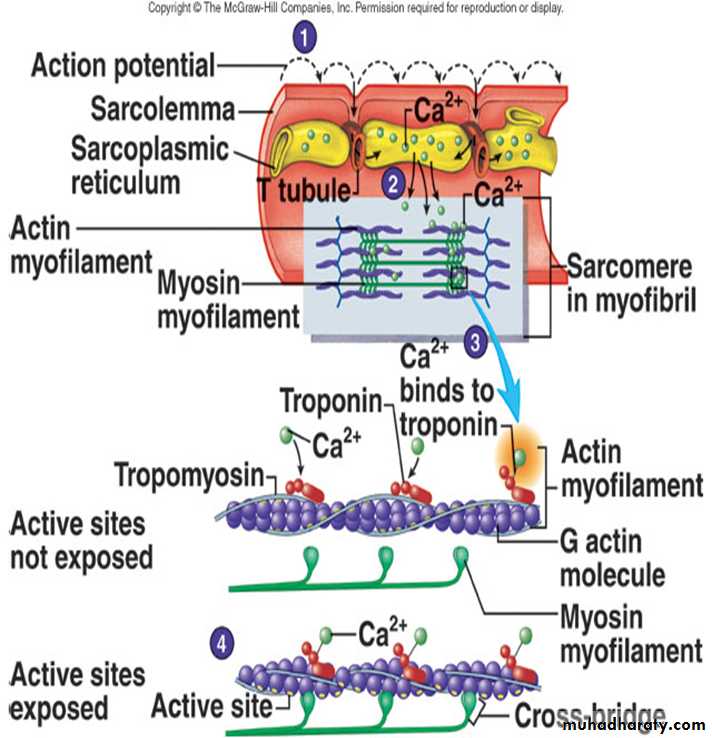
The Actin Filament Is Composed of Actin, Tropomyosin and Troponin.
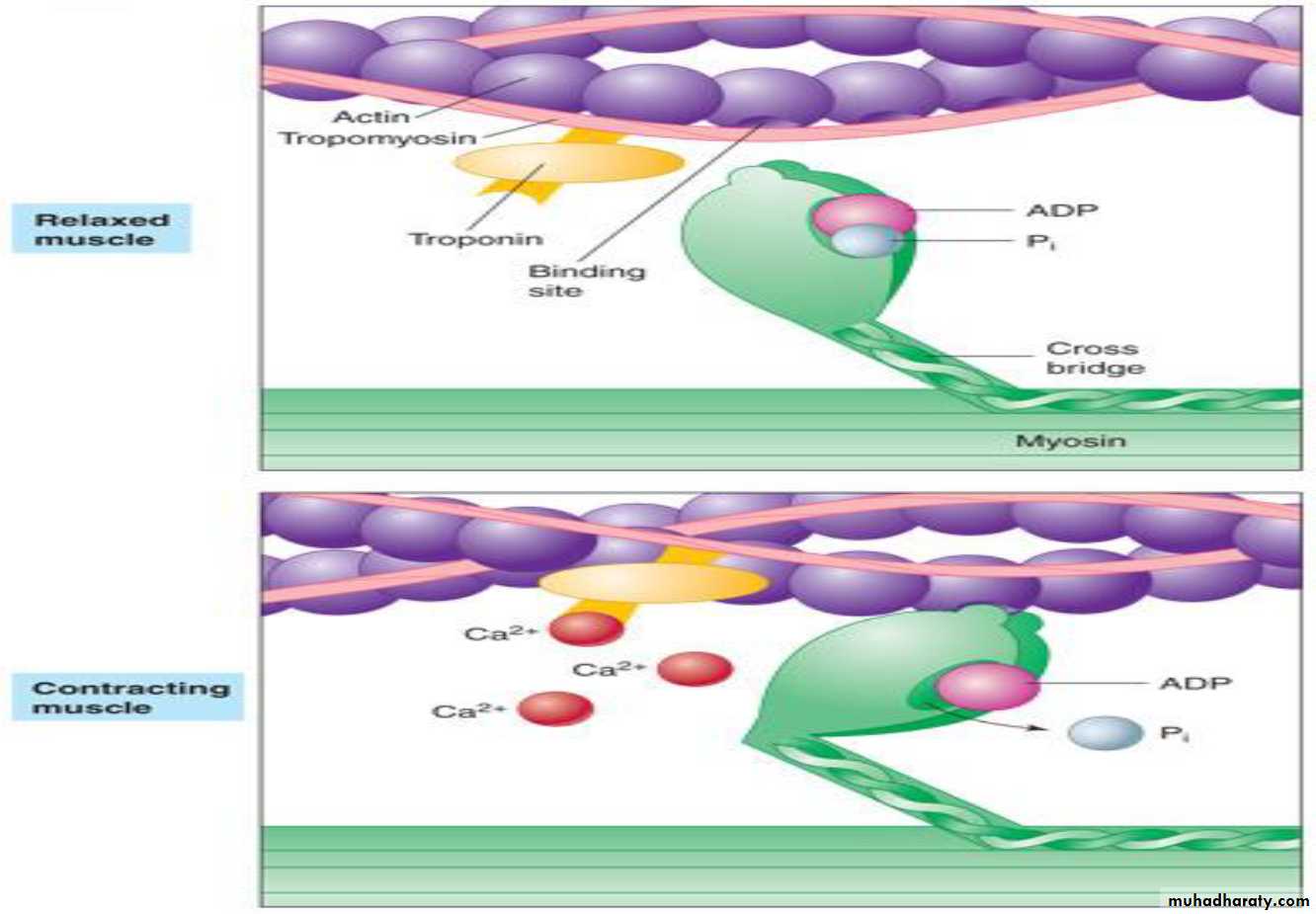
Each actin filament is about 1 mm long. The bases of the actin filaments are inserted strongly into the Z discs, whereas the other ends protrude in both directions into the adjacent sarcomeres where they lie in the spaces between the myosin molecules.The actin filament is inhibited by the troponin-tropomyosin complex :The active sites on the normal actin filament of the relaxed muscle are inhibited or physically covered by the troponin-tropomyosin complex.
Consequently، the sites cannot attach to the heads of the myosin filaments
to cause contraction until the inhibitory effect of the troponin tropomyosin
complex is itself inhibited.
Activation by calcium ions: The inhibitory effect of the troponin tropomyosin
complex on the actin filaments is inhibited in the presence of calcium ions. Calcium ions combine with troponin , causing the troponin complex to tug on the tropomyosin molecule. This “uncovers”
the active sites of the actin،allowing contraction to proceed
Control of cross bridge attachment to actin is via troponin-tropomyosin system
•The filament tropomyosin lies in groove between double row of G-actins of thin myofilament •Troponincomplex is attached to tropomyosin at intervals.In relaxed muscle, tropomyosin blocks binding sites on actin so crossbridges can’t connect. This occurs when sarcoplasmic Ca++levels are low
•Binding, thus contraction, can only occur when binding sites are exposed
When cytoplasmic Ca++levels rise, Ca++binds to troponin causing conformational change which moves tropomyosin and exposes binding sites
–Allows crossbridges to connect and contraction to occur , Crossbridge cycles stop when Ca++levels decrease
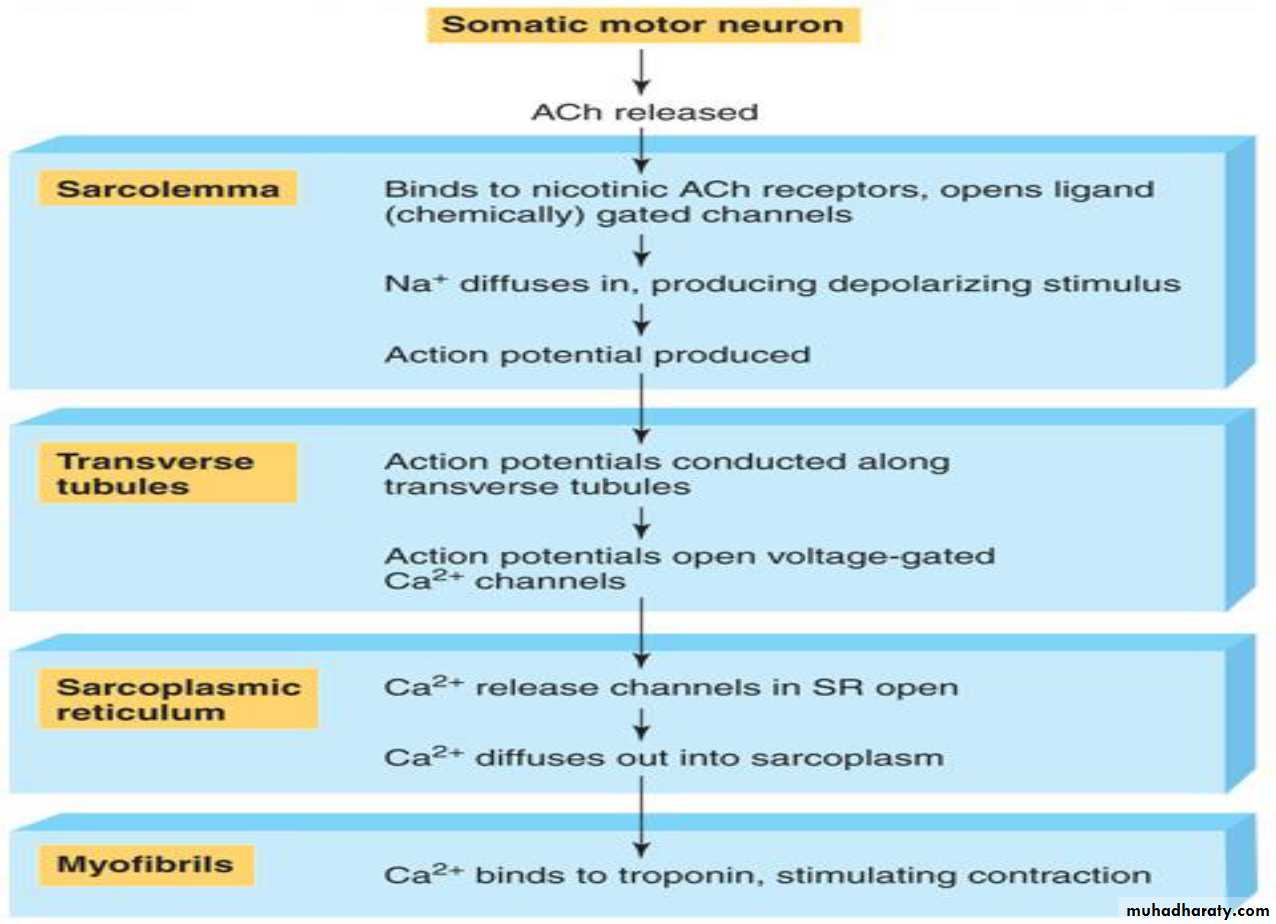
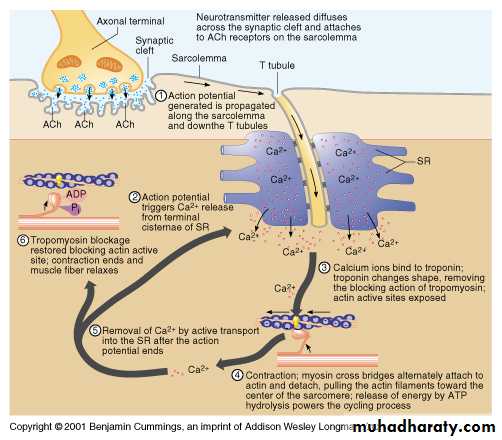
Excitation-Contraction Coupling
Skeletal muscle sarcolemma is excitable–Conducts APs just like axons
•Release of ACh at NMJ causes large depolarizing motor end-plate potentials and APs by opening sodium channels
•APs spread over sarcolemma and down into muscle via T tubules
**T tubules are extensions of sarcolemma
•APs in T tubules cause release of Ca++from terminal cisternae
1. Action potential (AP) travels down axon to neuromuscular junction.
2. AP causes calcium channels to open at synaptic end bulb which, in turn, causes synaptic vesicles to undergo exocytosis thus releasing their neurotransmitter (Ach).3. ACh diffuses across synaptic cleft and binds to membrane receptors on motor end (muscle cell).
4. Binding of ACh causes sodium channels to open and thus a depolarization of motor end plate.
5. Acetylcholinesterase breaks down the ACh.
6. At threshold an action potential ensues and spreads from motor end plate outward along sarcolemma.
7. Action potential travels down into muscle cell via transverse tubules.
8. AP causes calcium channels to open on terminal cisternae and calcium diffuses out throughout sarcoplasm.
9. Calcium binds to troponin causing the troponin/tropomyosin complex to move such that binding sites on actin for cross bridges are exposed.
10. Cross bridges connect to actin.
11. ATP is then released and the crossbridge bends pulling the thin myofilaments inward toward the center of sarcomere.
12. Z lines are pulled toward one another and the sarcomere shortens.
13. Another ATP binds to the crossbridge; crossbridge releases from actin; ATP is then split and the energy causes crossbridge to straighten again (energized state).
14. Entire process is repeated so long as there are stimulatory action potentials.
Muscle contraction
Steps for Contraction1-Neuron sends impulse releasing acetylcholine
2-Ca+ ions are released & actin exposes active sites
3-Myosin cross bridges attaches to actin & sarcomeres shorten
4-The muscle shortens & contracts
Mechanism of skeletal muscle contraction
The initiation and execution of muscle contraction occur in the followingsequential steps:
1. Skeletal muscle fibers are innervated by large, myelinated nerve fibers that originate from somatic motor neurons of the spinal cord. Each nerve fiber normally stimulates three to several hundred skeletal muscle fibers.
The nerve ending makes a junction, called the neuromuscular junction.
When a nerve impulse (action potential) reaches the neuromuscular
junction، vesicles containing acetylcholine are released into the synaptic cleft. This occurs because When the action potential spreads over the nerve terminal the calcium-gated channels open
allowing calcium ions to diffuse into the terminal of nerve. The calcium ions are believed to exert an attractive influence on the acetylcholine
vesicles، forcing these vesicles to fuse with the neural membrane and empty their acetylcholine into the synaptic space via the process of exocytosis. .
2. Acetylcholine opens acetylcholine-gated ion channels on the postsynaptic muscle membrane. This allow large numbers of sodium ions to pour into the inside of the muscle fiber, carrying with them large numbers of positive charges. This effect creates a local potential change at the muscle fiber membrane. This potential normally leads to opening of voltage-gated sodium channels, which initiate an action potential.
3. The action potential travels along the muscle fiber membrane, causing the sarcoplasmic reticulum to release calcium ions into the myofibrils that have been stored in the sarcoplasmic reticulum
4. The calcium ions initiate attractive forces between the actin and myosin filaments, causing them to slide together; this called the Sliding Filament Mechanism. Mechanical forces generated by the interaction of myosin cross-bridges with actin filaments cause the actin filaments to slide inward among the myosin filaments. But when AP travels over the muscle
forces are inhibited fiber membrane, the sarcoplasmic reticulum releases large quantities of calcium ions, which activate the forces between the myosin and actin filaments, and contraction begins.
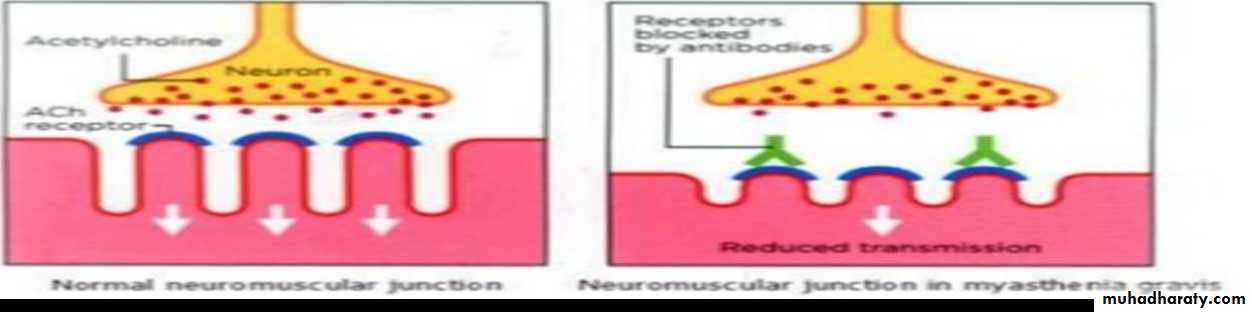
Myasthenia Gravis
Myasthenia gravis, which occurs in about 1 in every 20,000 persons, causes muscle paralysis because of inability of the neuromuscular junctions NMJ to transmit enough signals from the nerve fibers to the muscle fibers.
• Myasthenia gravis is an autoimmune disease(Antibodies which destroy the nicotinic Ach in NMJ , Antibodies 90% serum of patients) in which the patients have developed immunity against their own acetylcholine receptors the patient dies of paralysis, paralysis of the respiratory muscles .
• The disease can be managed by administering neostigmine or other anticholinesterase
drug, which allows larger than normal amounts of acetylcholine to accumulate in the synaptic space.
It's characterized by weakness of skeletal muscles due development of antibodies in the body against its own Ach activated ion channels.