Dr. Inas Aziz M. Jawad
U N I V E R S I T Y O F M O S U L
C O L L E G E O F D E N T I S T R Y
2020-2021
Department of
Prosthodontics

Dental Implants
I.
Definition
II.
Advantages & disadvantages
III.
Classifications
IV.
Materials used for dental
implant.
Definition:
A prosthetic device or
alloplastic material that
is surgically inserted into
soft or hard tissues, to be
used for functional or
cosmetic purposes.
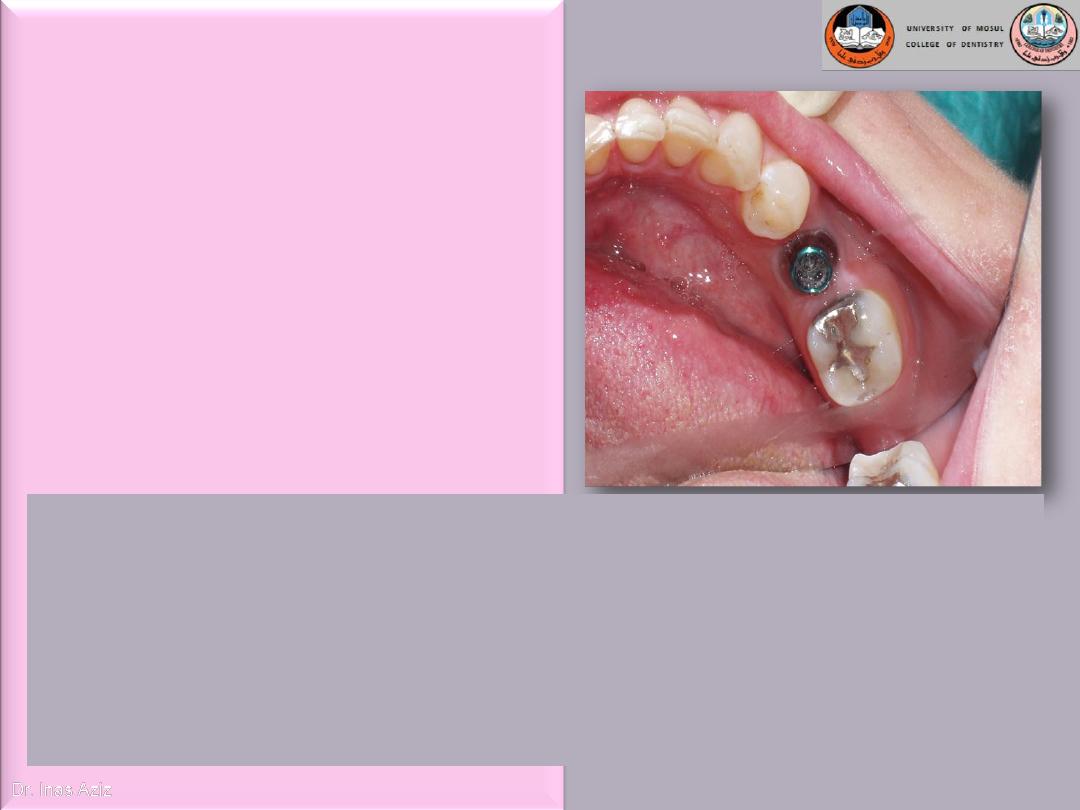
Dental Implant:
Dental implant provides an excellent fixed (non-removable)
solution to replace a single tooth or even many teeth that have
been lost. It overcomes many disadvantages of other
conventional methods of restorations (removable or fixed
prostheses).
Dental implants
Advantages of implant over conventional treatment
1) Better maintenance of residual bone.
2) Better improvement of occlusion, occlusal vertical
dimension, phonetics and facial esthetics.
3) Improve / regain oral proprioception
4) Increase prosthesis success
5) Maintains muscle of mastication and facial expression
6) Reduce size of prosthesis
7) Improve stability and retention of removable prosthesis
8) More permanent replacement
9) More psychological health
10) In cases of partial missing, adjacent teeth do not require
splinted restoration, therefore this decreases adjacent tooth
loss and maintains bone in site.

Disadvantages of implant treatment
1)
Expensive.
2)
The patient requires surgery.
3)
Time consuming.
4)
Technically complex.
CLASSIFICATIONS
OF
DENTAL IMPLANTS
I) Depending on the placement within the
tissues
1) Epithelial / mucosal implants
2) Epiosteal / Subperiosteal implants
3) Endosteal / endosseous implants
4) Transosteal / transosseous implants
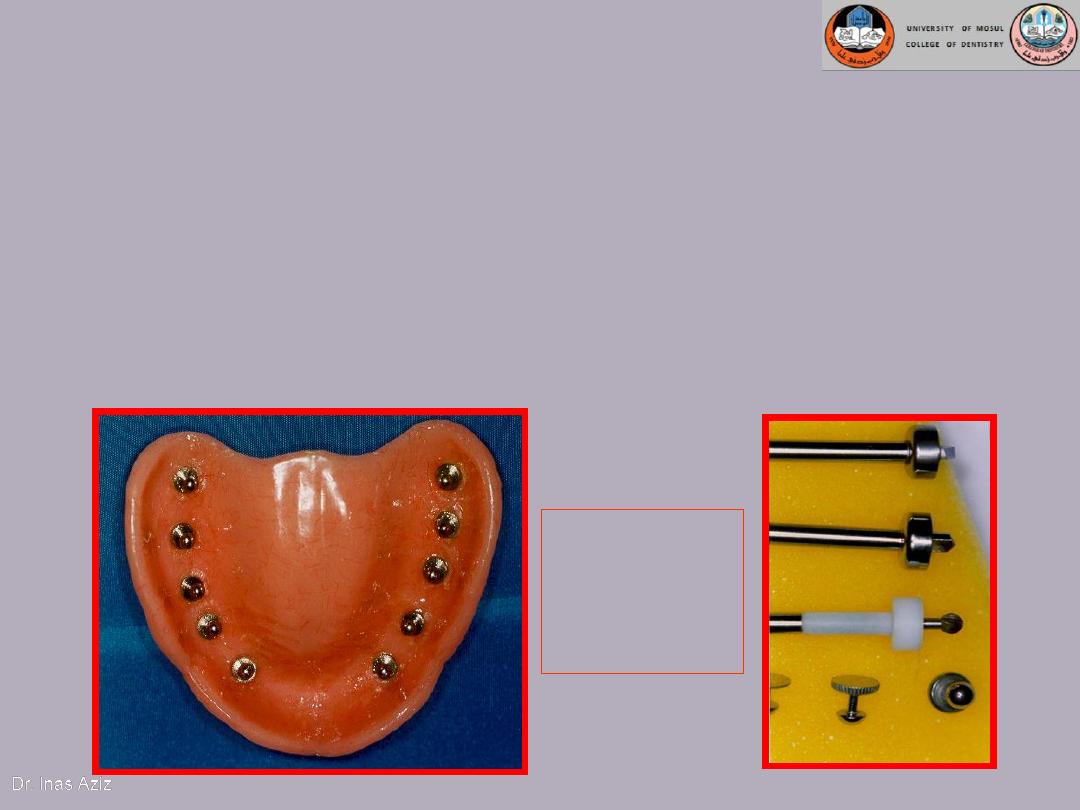
Epithelial / mucosal implants
They are inserted into the oral mucosa.
Disadvantages
1. painful healing
2. requirement of continual wear
Titanium
Mucosal
Implants

Epiosteal / Subperiosteal Implants
• They placed directly beneath
the periosteum overliying the
bony cortex (not anchored
inside the bone)
• Receive primary bone support
by resting on it.
Disadvantages :
1) Slow, predictable rejection of
the implant
2) Bone loss associated with
failure

• Usually indicated in a severely resorbed, completely
edentulous mandible which does not offer enough
bone height to accommodate root form implants as
anchoring devices.

Endosteal / Endosseous Implants
• Extends into basal
bone for support
• It transects into
one cortical plate
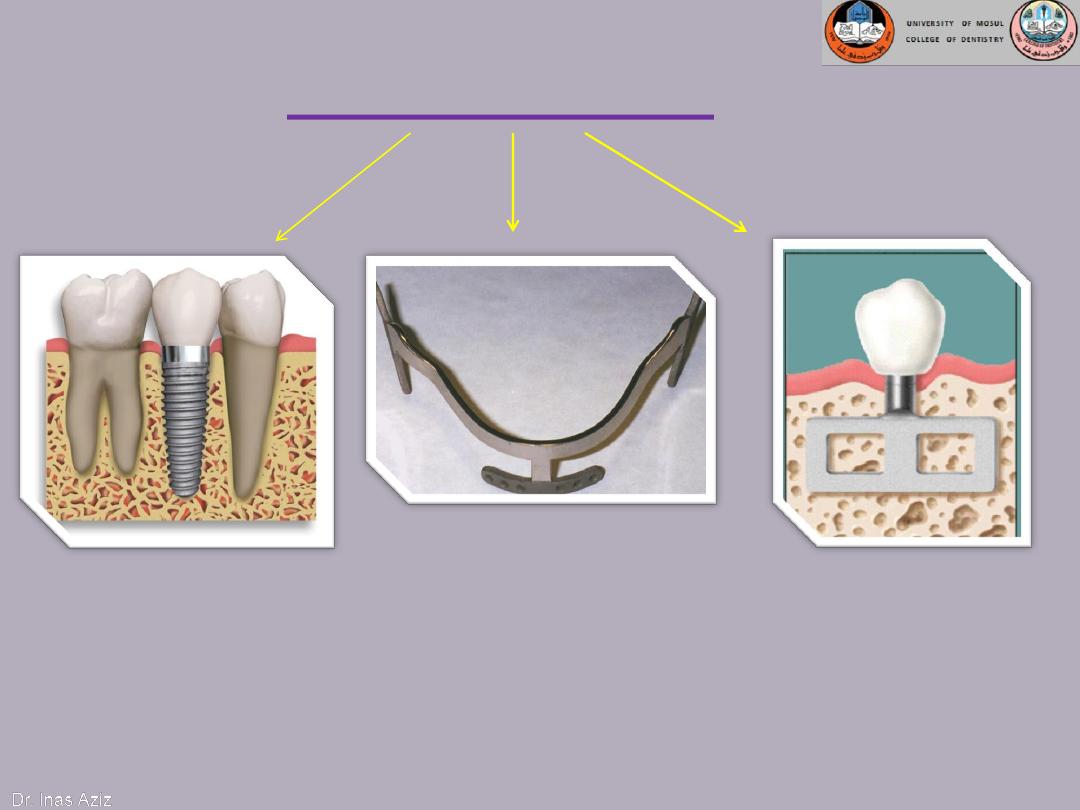
Endosteal implants
1-Root form implants
3-Plate form implants
1. Cylinder
2. Screw root form
3. Cone shaped
4. Combination
2-Ramus frame implants
Endosteal or Endosseous implant
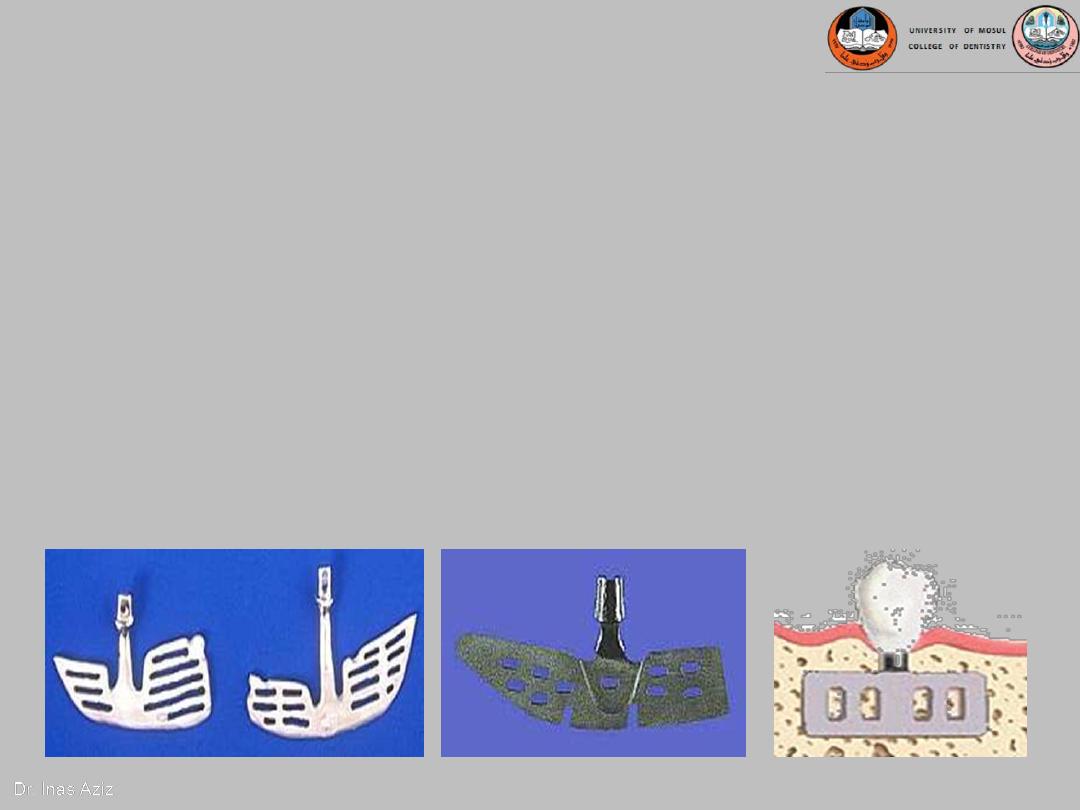
A. Plate-form implant :
Blade Implants have a long track record,
much longer than the Root form Implants.
Their name is derived from their flat,
blade-like (or plate-like) portion, which is
the part that gets embedded into the
bone.

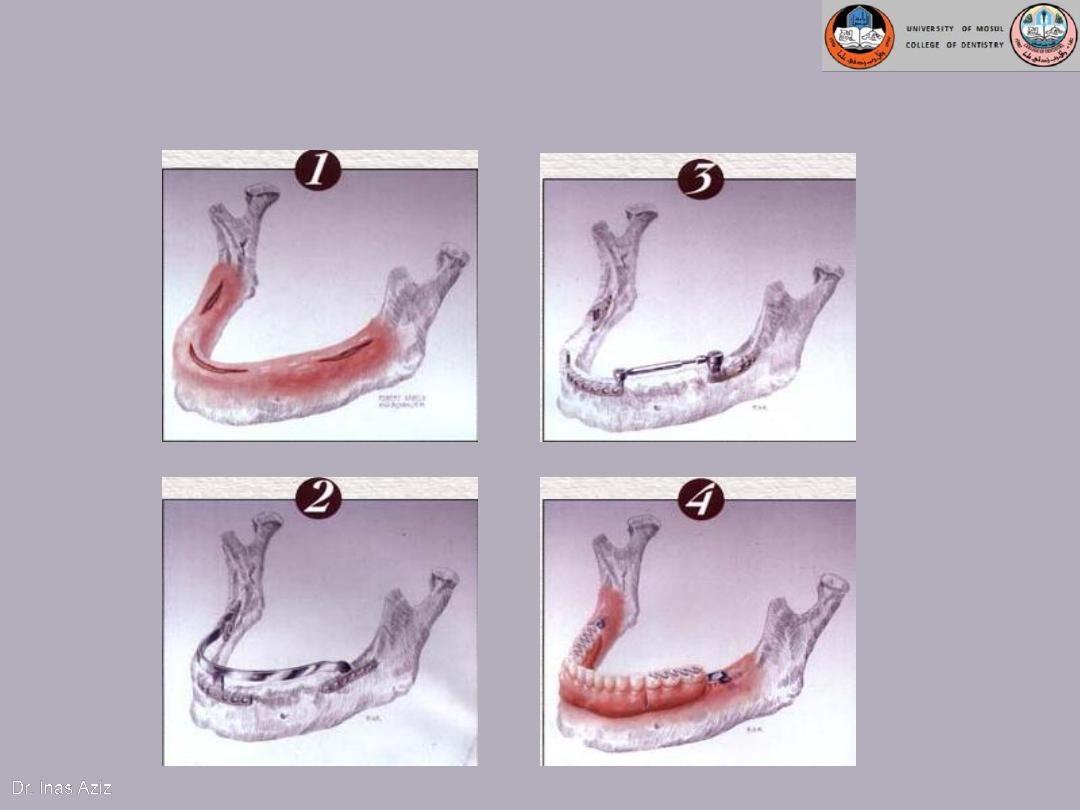
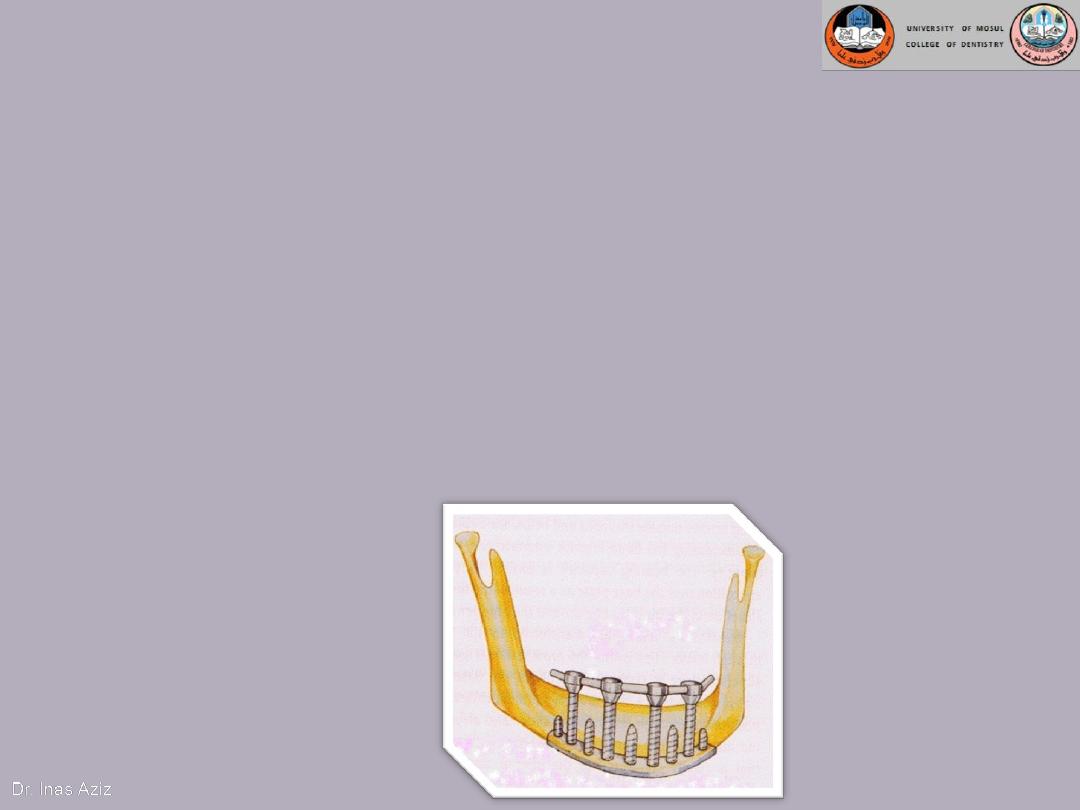
These implants are designed for the edentulous lower jaw
only and are surgically inserted into the jaw bone in three
different areas: the left and right back area of the jaw (the
approximate area of the wisdom teeth), and the chin area in
the front of the mouth.
It’s indicated in a severely resorbed, edentulous mandible
which does not offer enough bone height to accommodate
Root form Implants.
It provides a tripodial stabilization of the thin lower jaw and
protects it from fracturing.
B. Ramus-frame implant
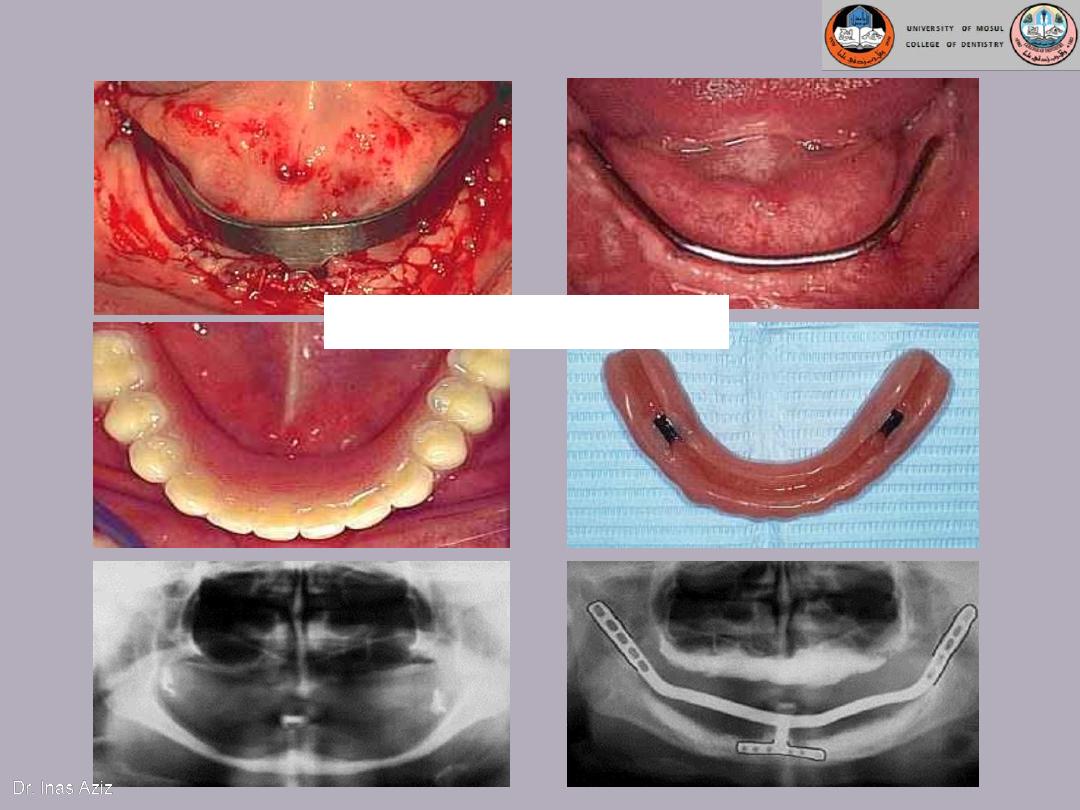
Ramus-frame implant
Ramus-frame implant
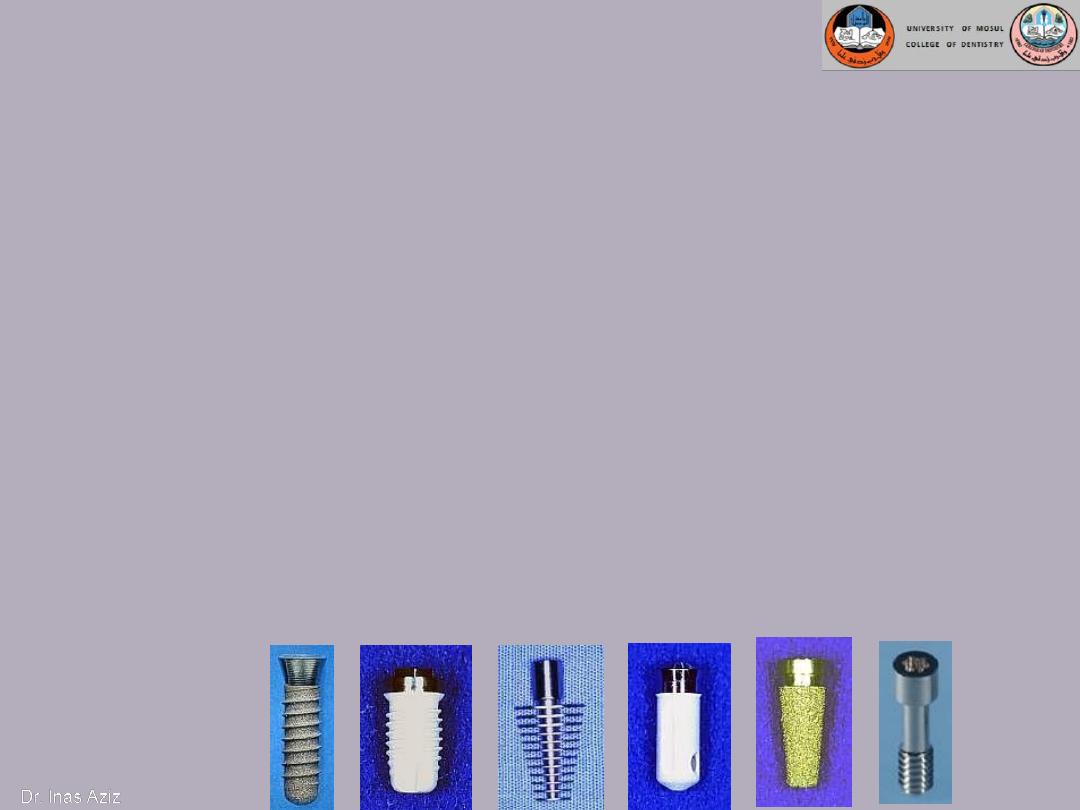
C. Root form implant
The most popular implants in the world today.
come in a variety of shapes, sizes, and materials
can be placed wherever a tooth or several teeth are
missing when enough bone is available to
accommodate them.
if the bone volume is not sufficient to place Root form
Implants, Bone grafting procedures within reasonable
limits should be initiated, in order to benefit from
these implants.
Transosteal / Transosseous Implant
• Also called as Staple Bone Implant, Transmandibular Implant
• Penetrates both cortical plate and passes through the entire
thickness of the alveolar bone
• Use restricted to anterior area of mandible
• It is not used much any more because they necessitate an
extraoral surgical approach.
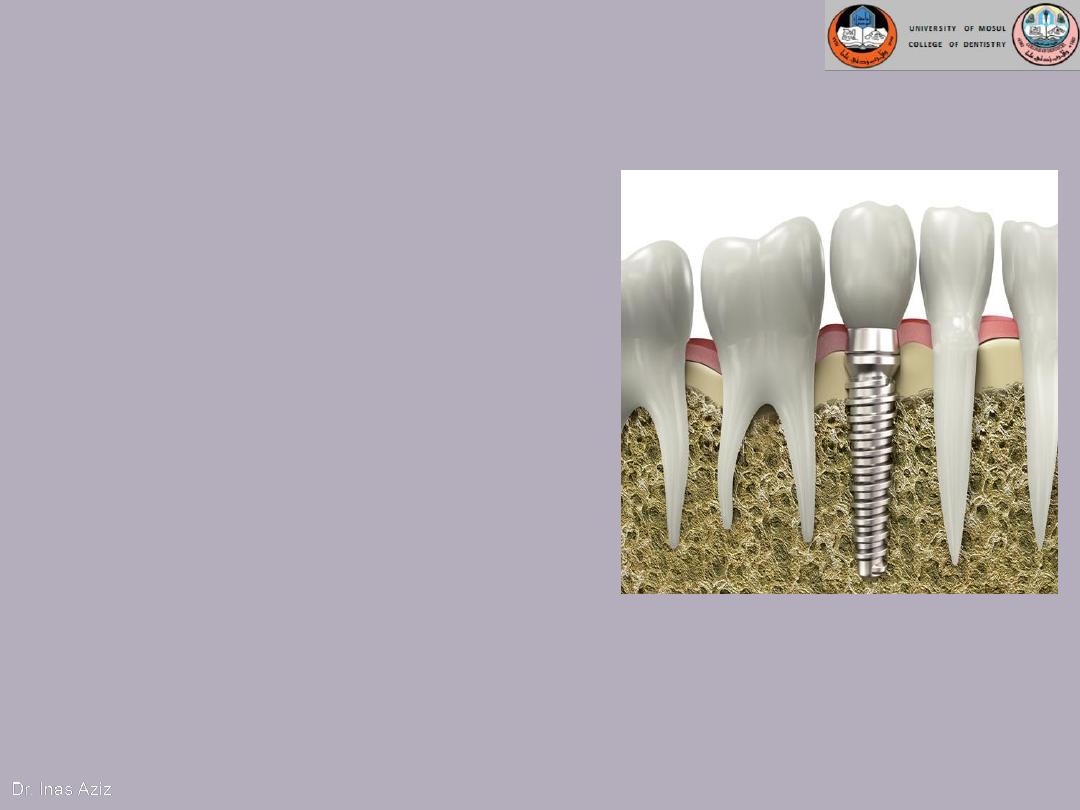
The most universally used
implants are
root form
endosseous implants
which
extend into basal bone for
support and transect one
cortical plate.
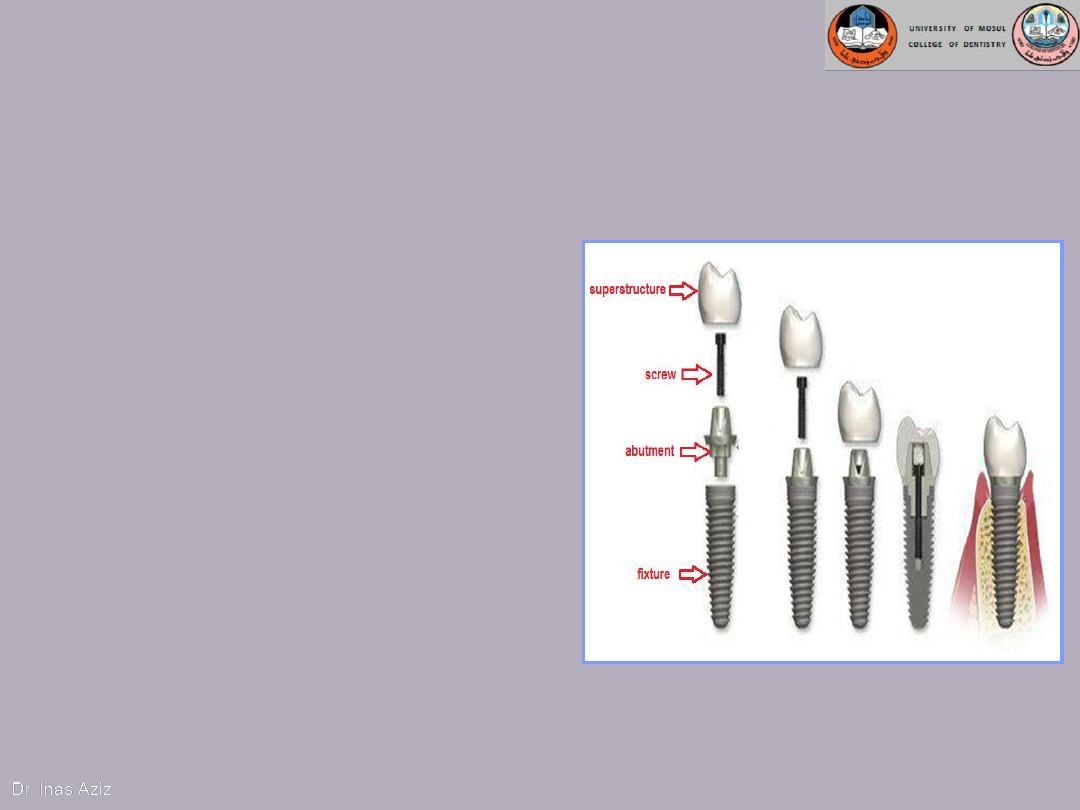
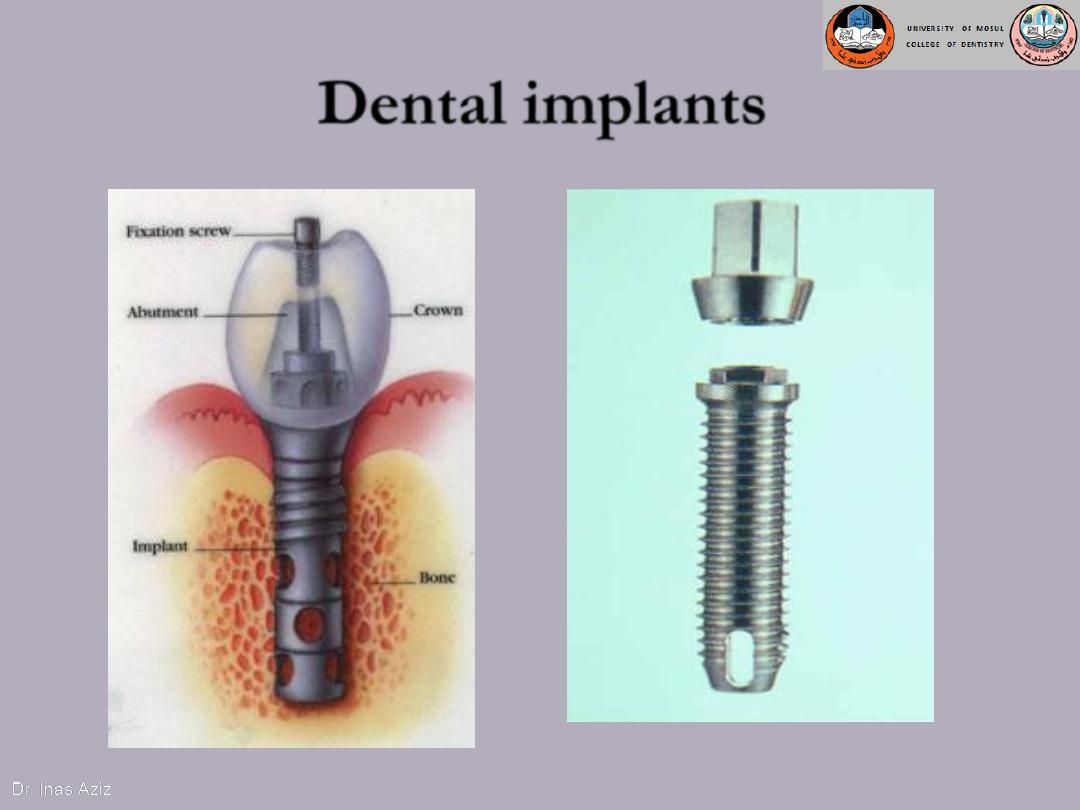
A dental implant actually consists of:
A. PRIMARY COMPONENTS:
1.
anchorage part/ implant body/
fixture.
2.
abutment.
3.
superstructure.
B. ACCESSORIES:
a– Surgical 1. cover screw
2. gingival former
b– Prosthetic 1. implant analogue
2. impression post
Dental Implant Components

Dental Implant Components
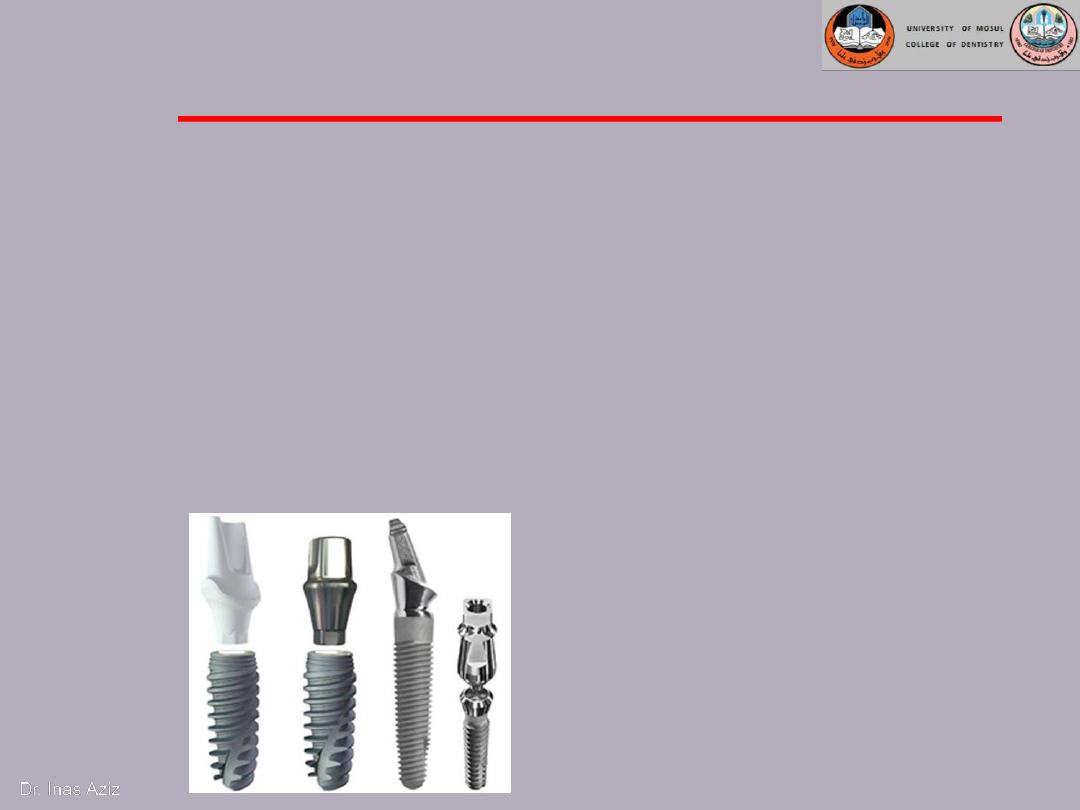
ANCHORAGE PART/ IMPLANT
BODY (FIXTURE):
is the implant
component that is placed into jaw
bone to act just like a tooth root,
providing a sound and permanent
foundation.
Types of fixture:
1.
Cylindrical or tapered
cylindrical
2.
Smooth or threaded surface to
increase surface contact and
maximize initial contact with
the bone.
3.
Solid or with holes or vents to
allow bone growth through.

IMPLANT SUPERSTRUCTURE
:
is a prosthesis fabricated with the
support of dental implants.
Types:
.
Crown
Fixed Bridge
1. Fixed prostheses:
crowns and bridges, or act
as orthodontic anchor.
2. Removable prostheses:
overdenture, maxillofacial
prostheses.
3. Fixed detachable
prostheses: Hybrid
dentures
II) Depending on the materials used
1) METALLIC IMPLANTS
Gold alloys
Cobalt-chromium alloys
Stainless Steel
Niobium
Tantalum
Commercially pure Titanium(CpTi)
Titanium alloy (Ti-6Al-4V)
2) CERAMIC IMPLANTS:
Aluminum oxide
Zirconium
Hydroxyapatite
Tricalcium phosphate
Bioglass
Carbon silicon
3) POLYMERIC IMPLANTS:
Polyethelene
Polyamide
PMM
Polytetra
Polyurethene
Implant materials
Implant materials can be classified based on the type of material
used and the biological response they elicit when implanted
1- Biotolerant: these materials are not easily rejected when
implanted into living tissue but are surrounded by a fibrous
layer.
E.g. 1) Metals like gold, Co-Cr alloy, stainless steel, zirconium,
nobium
2) Polymers like polyethylene, polyamide,
polymethylmerthacrylate, polyurethane
Dr. Inas Aziz
Implant materials (cont.)
2- Bioinert: these materials allow close apposition of bone on
their surface, leading to contact osteogenesis.
E.g.
1)
Metals like commercially pure titanium (Cp- Ti) and titanium
alloy
2)
Ceramics like aluminum oxide and zirconium oxide
CreatingSmiles

Implant materials (cont.)
3- Bioactive: these materials allow the formation of bone onto
their surface, by ion exchange with host tissue leads to the
formation of a chemical bond along the interface.
E.g.
Ceramics like HA, tricalcium phosphate, bioglass, fluorapatite,
and carbon-silicon.
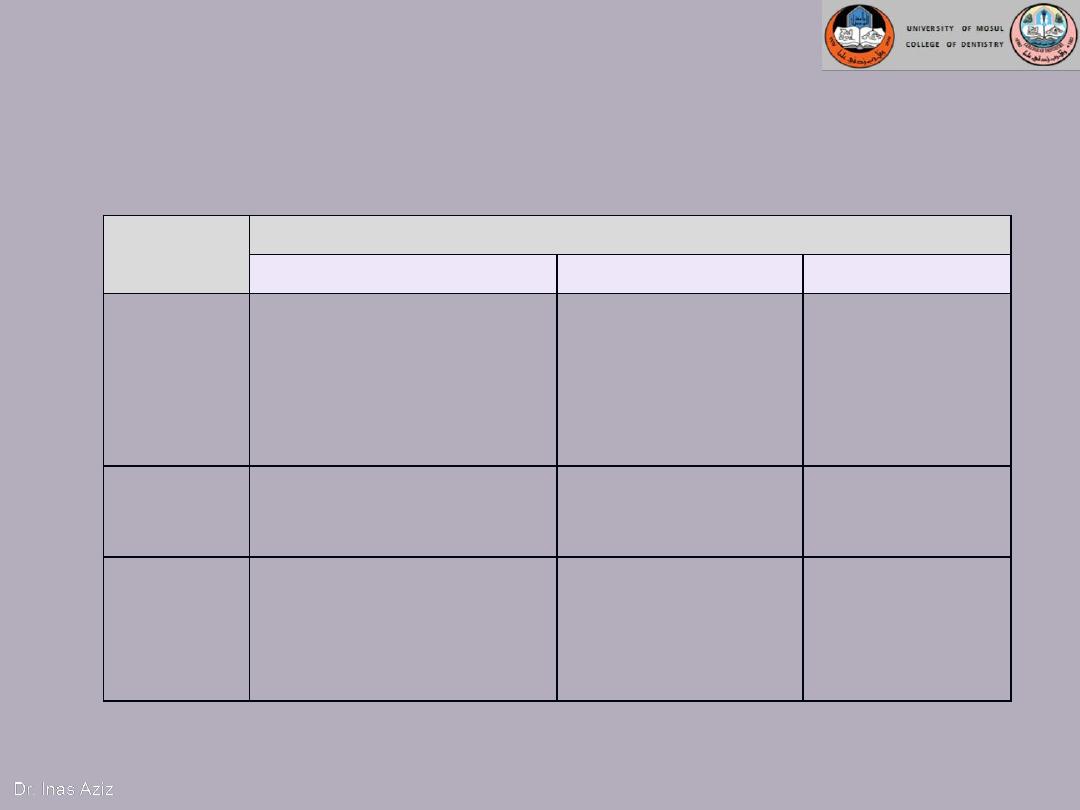
Implant materials (cont.)
Implant materials can be classified based on the type of material
used and the biological response they elicit when implanted
Biodynamic
activity
Chemical compositions
metals
ceramics
polymers
biotolerant
Gold alloys
Cobalt-chromium alloys
Stainless Steel
Niobium
Tantalum
Polyethelene
Polyamide
PMM
Polytetra
Polyurethene
bioinert
Commercially pure
Titanium(Cp Ti)
Titanium alloy (Ti-6Al-4V)
Aluminum oxide
Zirconium
bioactive
Hydroxyapatite
Tricalcium
phosphate
Bioglass
Carbon silicon
Biological response
means the relation of the implant material with the
surrounding tissues.

THAN
K YOU
Thanks



