
Dr. Inas Aziz M. Jawad
U N I V E R S I T Y O F M O S U L
C O L L E G E O F D E N T I S T R Y
2020-2021
Department of
Prosthodontics
Part II

Contents:
I.
Osseointegration
II.
Prerequisites for Achieving
Osseointegration
III.
The Biomechnics of Dental
Implants
IV.
Treatment-Planning
Determinants for edentulous
mandible.
Osseointegration
The phenomenon of
osseointegration
was
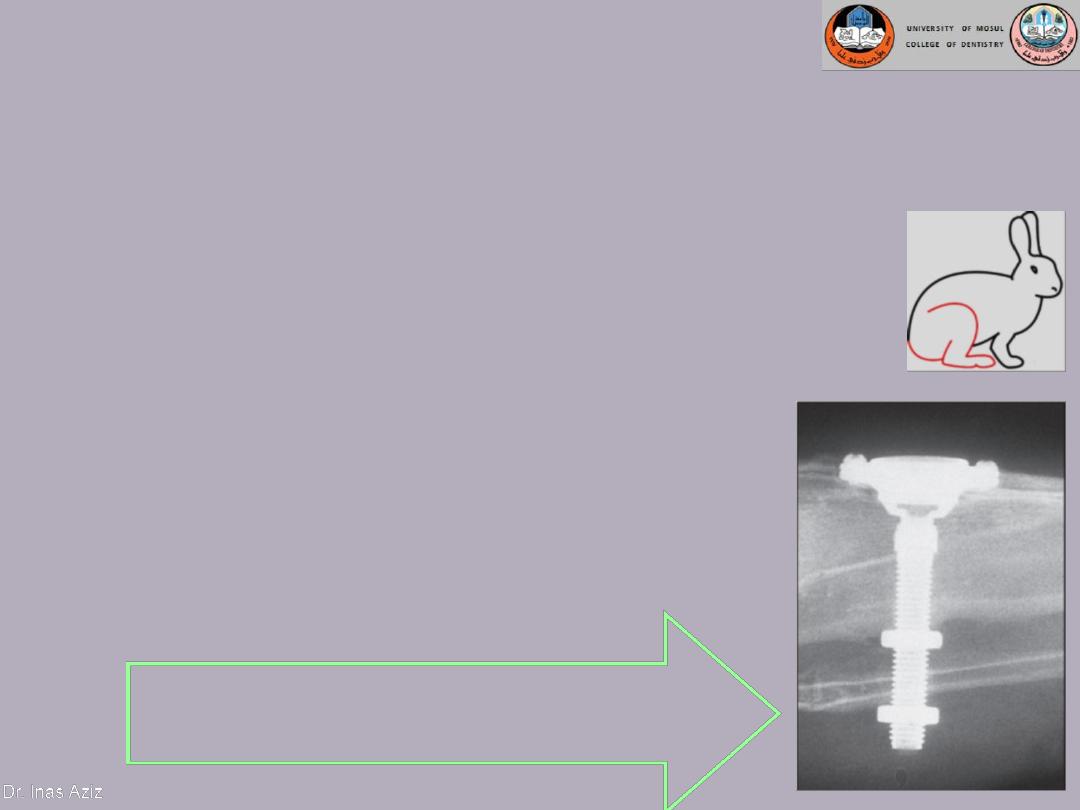
discovered by Professor Per-Ingvar Brånemark
These implants were made of titanium, and
when an implant was placed in a rabbit tibia,
bone was deposited on its surface, firmly
anchoring the implant in the surrounding bone.
A radiograph of the titanium optical chamber
embedded in a rabbit tibia bone.
When the concept of osseointegration was introduced
to the international dental community in the early
1980s, it represented a radically new concept in
implant dentistry.
Osseointegration
When bone forming cells (osteoblasts) attach
themselves to the titanium implant, a structural
and functional bridge forms between the
body’s bone and the newly implanted, foreign
object. This process resulted from remodeling
within bone tissue is called Osseointegration.
Osseointegration
is defined as a time dependent healing
process whereby clinically asymptomatic rigid fixation of
alloplastic materials is achieved, and maintained, in bone
during functional loading (Zarb &Albrektsson,)
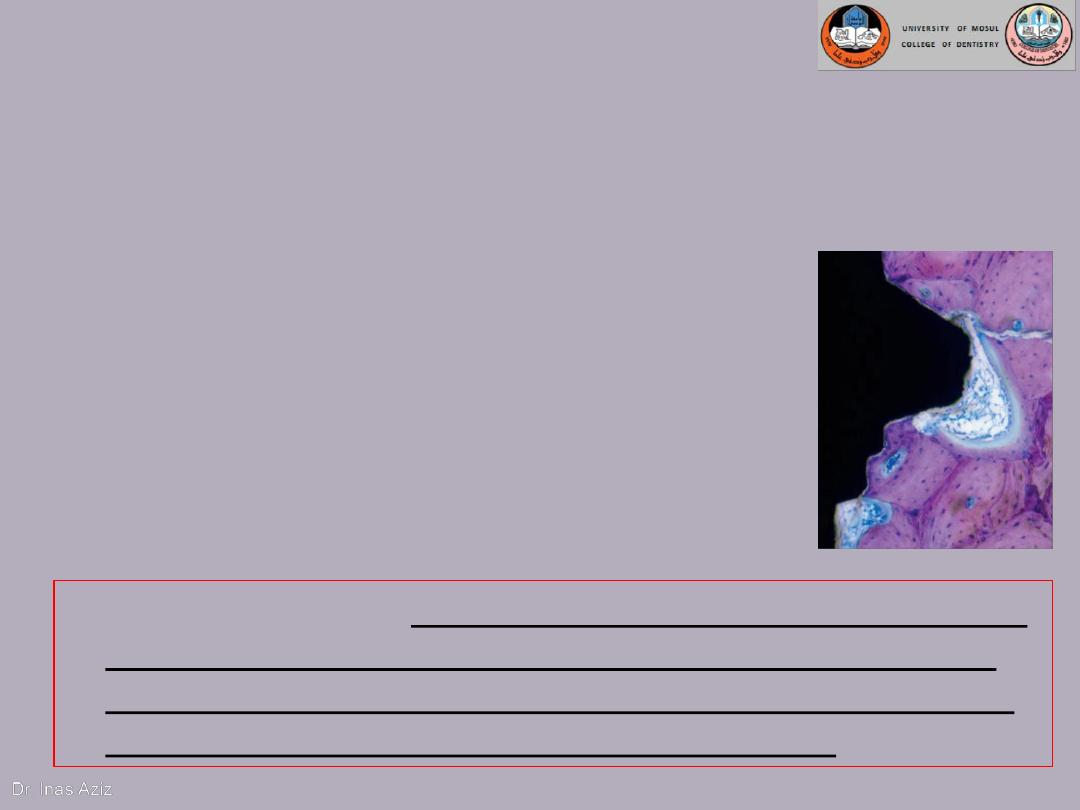
Histologic appearance resembled a functional ankylosis with no
intervention of fibrous or connective tissue between bone and
implant surface.
Osseointegration
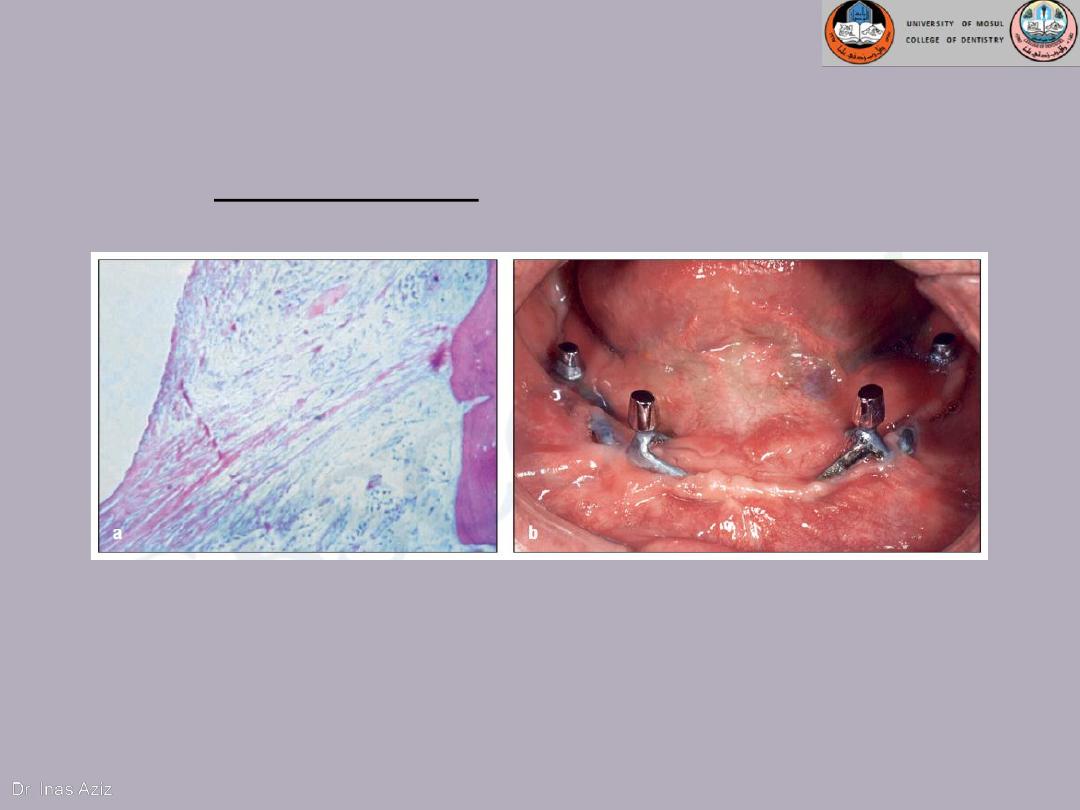
(a) Subperiosteal implants of
chrome-cobalt are enveloped
by fibrous connective tissue.
(b) Epithelial migration led to the
formation of extended peri-implant
pockets, which in turn developed into
chronic infection. The infection led to
exposure of the implant struts and
eventual loss of the implant.
The implant material is an important factor for Osseo
integration to occur.

Prerequisites for Achieving
Osseointegration
The successful outcome of any implant procedure is mainly
dependent on the interrelationship of the various components of an
equation that includes the following:
• 1.Biocompatibility of the implant material
• 2.Macroscopic and microscopic nature of the implant surface &
designs
• 3.The status of the implant bed in both a health and a
morphologic (bone quality) context
• 4.The surgical technique per se
• 5.The undisturbed healing phase
• 6.Loading conditions
• The challenge confronting the clinician is that these several
factors must be controlled almost simultaneously, if a predictably
successful outcome is to be expected.
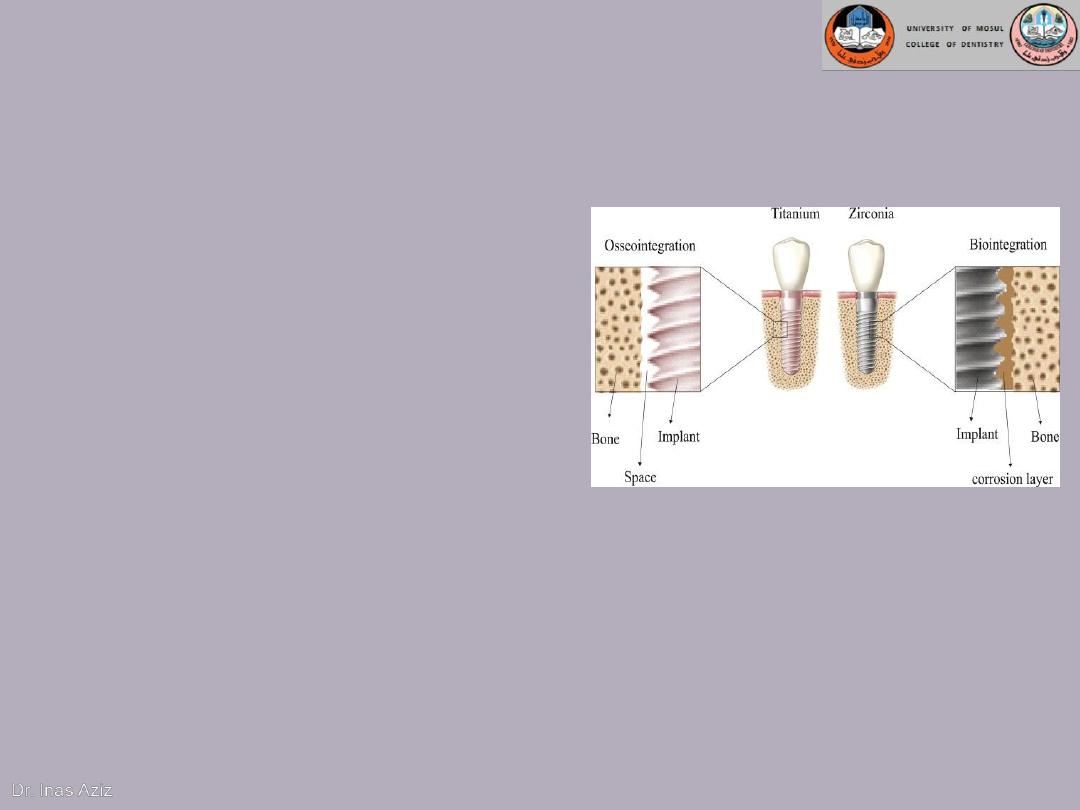
1.Biocompatibility of the implant material
This is the property of implant
material to show favorable
response in given biological
environment in a particular
function. It depends on the
corrosion resistance and
cytotoxicity of corrosion
products.
Clinical significance of corrosion: Implant bio-material should be
corrosion resistant. Corrosion can result in roughening of the
surface, weakening of the restoration, release of elements from
the metal or alloy, toxic reactions. Adjacent tissues may be
discolored and allergic reactions in patients may result due to
release of elements.

1.Biocompatibility of the implant material
Today, the most accepted material
1)
Cp titanium (commercially pure
titanium)
2)
Titanium alloy (titanium-6aluminum-
4vanadium)
3)
Zirconium
4)
Hydroxyapatite (HA), one type of
calcium phosphate ceramic material
Titanium with
(HA) coating
Zirconium
2.Macroscopic and microscopic nature of the
implant surface & designs
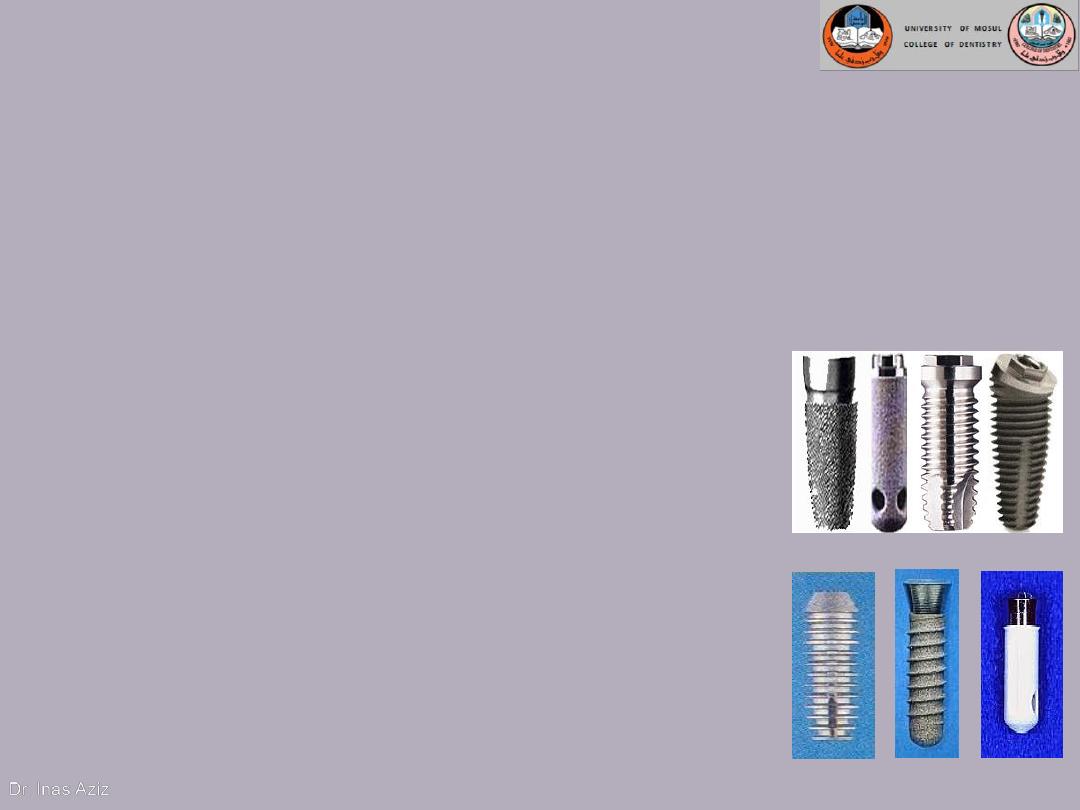
A. Implant design (root-form)
Cylindrical Implant
- most conducive
Threaded Implant:most implant forms
have been developed as a serrated thread.
a.
to maintain a clear steady state bone
response.
b.
to enhance initial stability
c.
to increase surface contact.
Different implant materials and designs are being used to
obtain surfaces increasing osseointegration.
2.Macroscopic and microscopic nature of the
implant surface & designs (cont.)
B. Implant surface
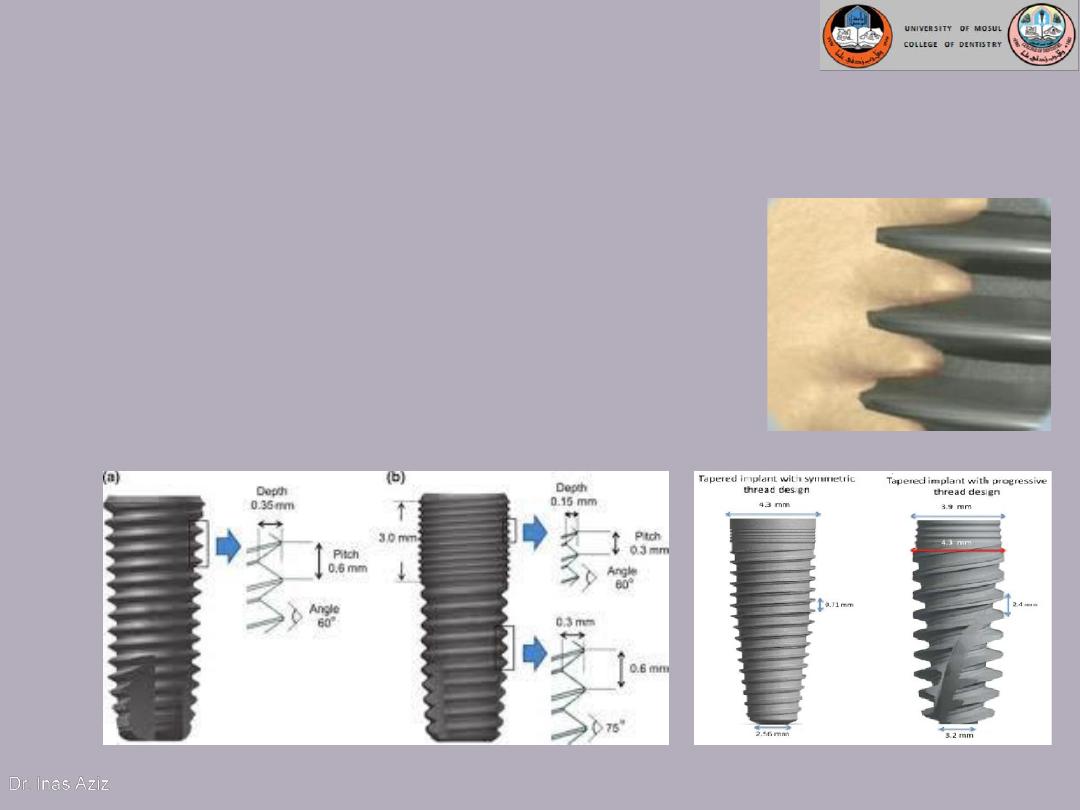
Increased pitch (the number of threads
per unit length) and increased depth
between individual threads allows for
improved contact area between bone
and implant.
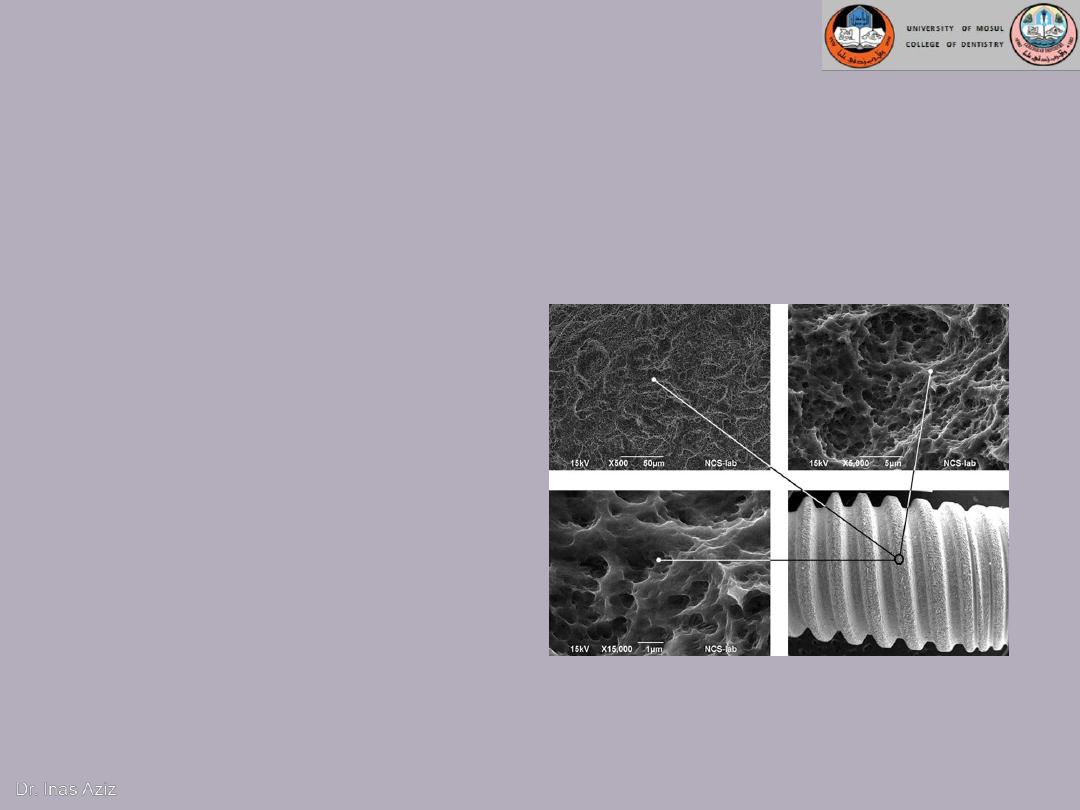
B. Implant surface
Mild rough surface increases the contact area between bone
and implant surface.
Reactive implant surface
by anodizing (Oxide layer)
,acid etching or HA
coating enhanced
osseointegration
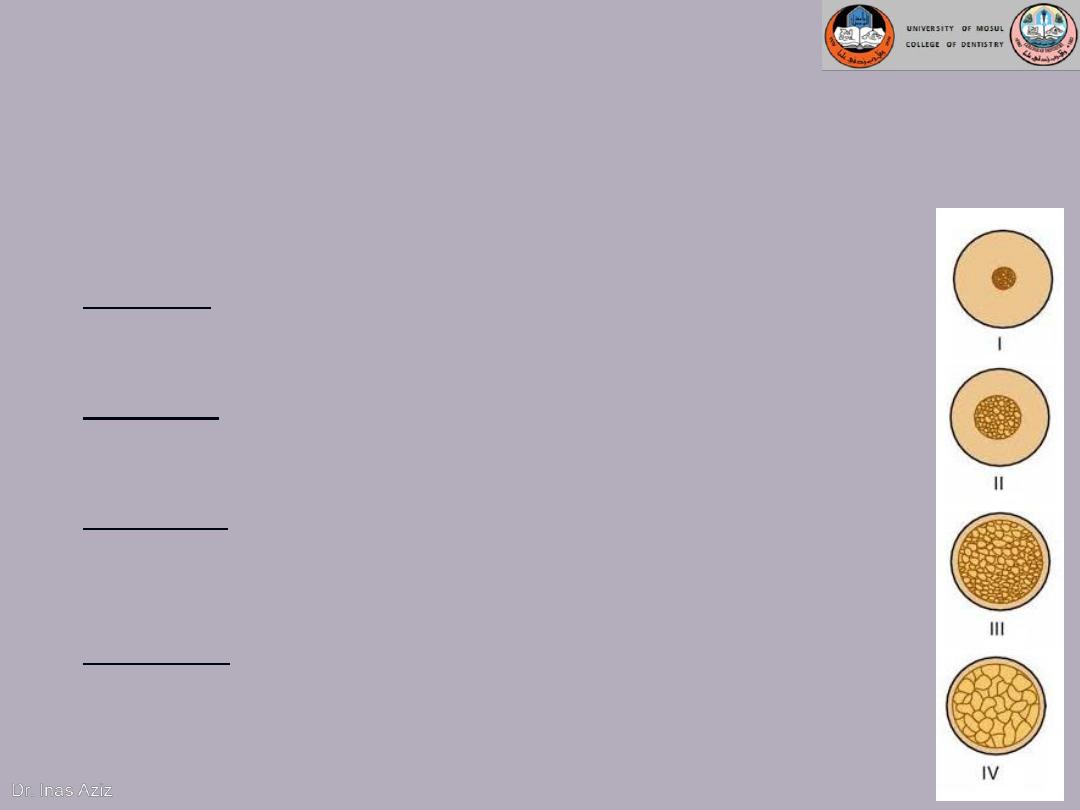
3.The status of the implant bed in both a
health and a morphologic (bone quality)
context
Good bone quality and healthy surgical site
Quality I: Was composed of homogenous compact bone,
usually found in the anterior lower jaw.
Quality II: Had a thick layer of cortical bone surrounding dense
trabecular bone, usually found in the posterior lower jaw.
Quality III: Had a thin layer of cortical bone surrounding dense
trabecular bone, normally found in the anterior upper jaw but
can also be seen in the posterior lower jaw and the posterior
upper jaw.
Quality IV: Had a very thin layer of cortical bone surrounding
a core of low-density trabecular bone, It is very soft bone and
normally found in the posterior upper jaw. It can also be seen
in the anterior upper jaw.
4.The surgical technique per se
Minimum possible trauma and minimal tissue violence at
surgery is essential for proper osseointegration.
Careful cooling while surgical drilling is performed at low
rotatory rates
Use of sharp drills
Use of graded series of drills
Proper drill geometry is important, as intermittent
drilling.
The insertion torque should be of a moderate level
because strong insertion torques may result in stress
concentrations around the implant, with subsequent bone
resorption.

5.The undisturbed healing phase
Micromovement of the implant is thought to
disturb the tissue and vascular structures
necessary for initial bone healing.
Excessive micromovement of the implant during
healing prevents the fibrin clot from adhering to
the implant surface. Eventually, the healing
processes are reprogrammed, leading to a
connective tissue–implant interface as opposed
to a bone-implant interface.
6. Loading conditions
After the placement of dental
implants, a 3 – 6 month load-free
healing period.
Advantages: allow the optimal
period to ensure successful
healing and the bone formation
required osseointegration.
Disadvantage: a. long treatment
time.
b. Delayed restoration of esthetic
and function.
It means placing a full occlusal load
onto the implant via the
prosthesis, within 72 hours after
placement.
Advantages: a. allow for shorter
treatment time.
b. allow for immediate restoration
of function and esthetics.
Disadvantage: an increased risk of
implant failure because the
increased vertical or lateral force
upon the implant during the
healing phase results in implant
motion, aberrant healing and
fibrous tissue encapsulation.
2- Immediate loading:
1- Delayed loading:
The Biomechnics of Dental Implants
In all incidences of clinical loading, occlusal forces
are first introduced to the prosthesis and then
reach the bone-implant interface via the implant.
This is affected by:
1)
Force directions and magnitudes,
2)
Prosthesis type,
3)
Prosthesis material,
4)
Implant design,
5)
Number and distribution of supporting
implants,
6)
Bone density, and
7)
The mechanical properties of the bone-implant
interface.
Prosthetic Attachments
They include:
1. Implant abutment
2. Implant superstructure
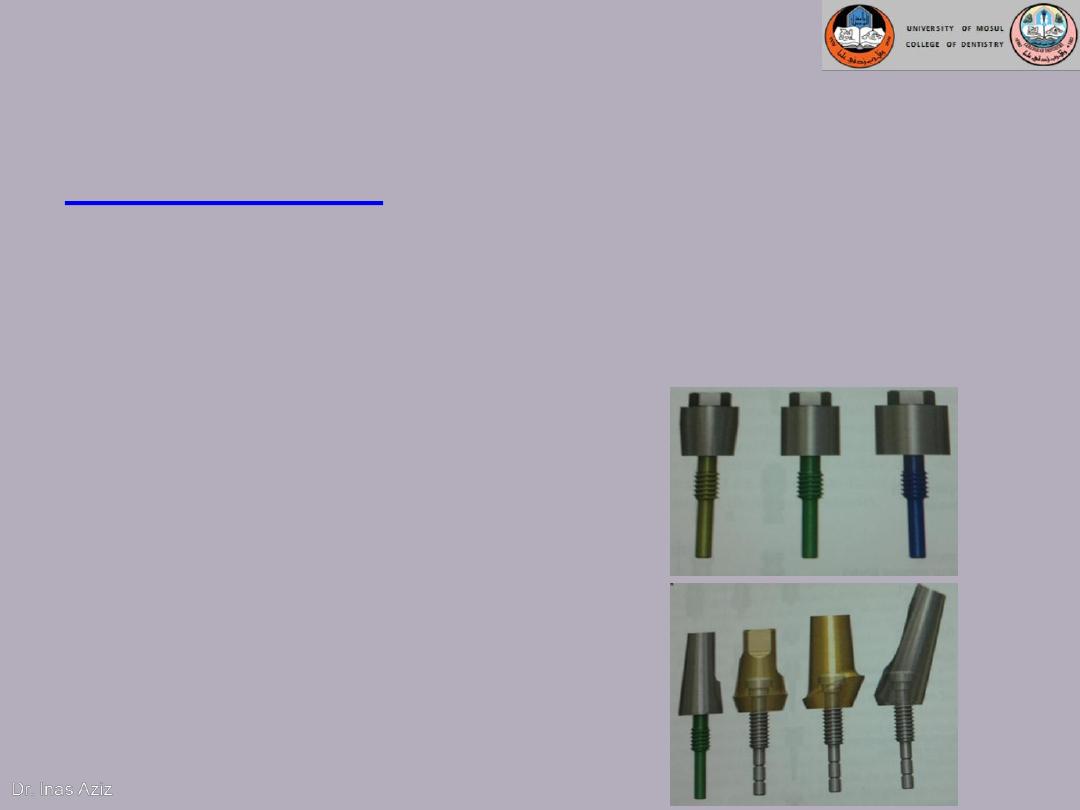
Prosthetic Attachments
Implant abutment
: it is the portion of the implant that
supports or retains a prosthesis or implant
superstructure.
It is classified, based on method by which prosthesis or
superstructure is retained to the abutment, into:
1- Screw retention
2- cement retention
Prosthetic Attachments
Super structure:
is defined as the superior part of
multiple layer prosthesis that includes the replaced
teeth and associated structures.
The superstructure for completely
edentulous patients
Implant-retained removable overdenture
Implant-supported removable overdenture
Fixed detachable prosthesis (Hybrid prosthesis)
Implant supported Fixed prosthesis:
1) Screwed-in Fixed Bridge
2) Cemented Fixed Bridge

Treatment-Planning Determinants
for edentulous mandible
Implant-Retained Versus
Implant-Supported Overdentures Versus
Fixed Prostheses
1.
Alveolar ridge resorption
2.
Amount of keratinized attached mucosa
3.
Oral compliance
4.
Esthetics
5.
Cost
6.
Patient preference

THANK
YOU
