بسم الله الرحمن الرحيم
Lecture 7, 8 - Neurophysioloy Dr. Noor
2nd stage 2021
………………………………………………………………
The Autonomic Nervous System
Objective :
What is the physiologic anatomy of sympathetic and para sympathetic Nervous System?
What is Effects of Sympathetic and Parasympathetic Stimulation on Specific Organs?
The portion of the nervous system that controls most visceral functions of the body is called the autonomic nervous system. This system helps to control arterial pressure, gastrointestinal motility, gastrointestinal secretion, urinary bladder emptying, sweating, body temperature, and many other activities, some of which are controlled almost entirely and some only partially by the autonomic nervous system.
One of the most striking characteristics of the autonomic nervous system is the rapidity and intensity with which it can change visceral functions.
For instance, within 3 to 5 seconds it can increase the heart rate to twice normal, and within 10 to 15 seconds the arterial pressure can be doubled; or, at the other extreme, the arterial pressure can be decreased low enough within 10 to 15 seconds to cause fainting. Sweating can begin within seconds, and the urinary bladder may empty involuntarily, also within seconds.
General Organization of the Autonomic Nervous System
The autonomic nervous system is activated mainly by centers located in the spinal cord, brain stem, and hypothalamus. Also, portions of the cerebral cortex, especially of the limbic cortex, can transmit signals to the lower centers and in this way influence autonomic control.
The autonomic nervous system also often operates by means of visceral reflexes. That is, subconscious sensory signals from a visceral organ can enter the autonomic ganglia, the brain stem, or the hypothalamus and then return subconscious reflex responses directly back to the visceral organ to control its activities.
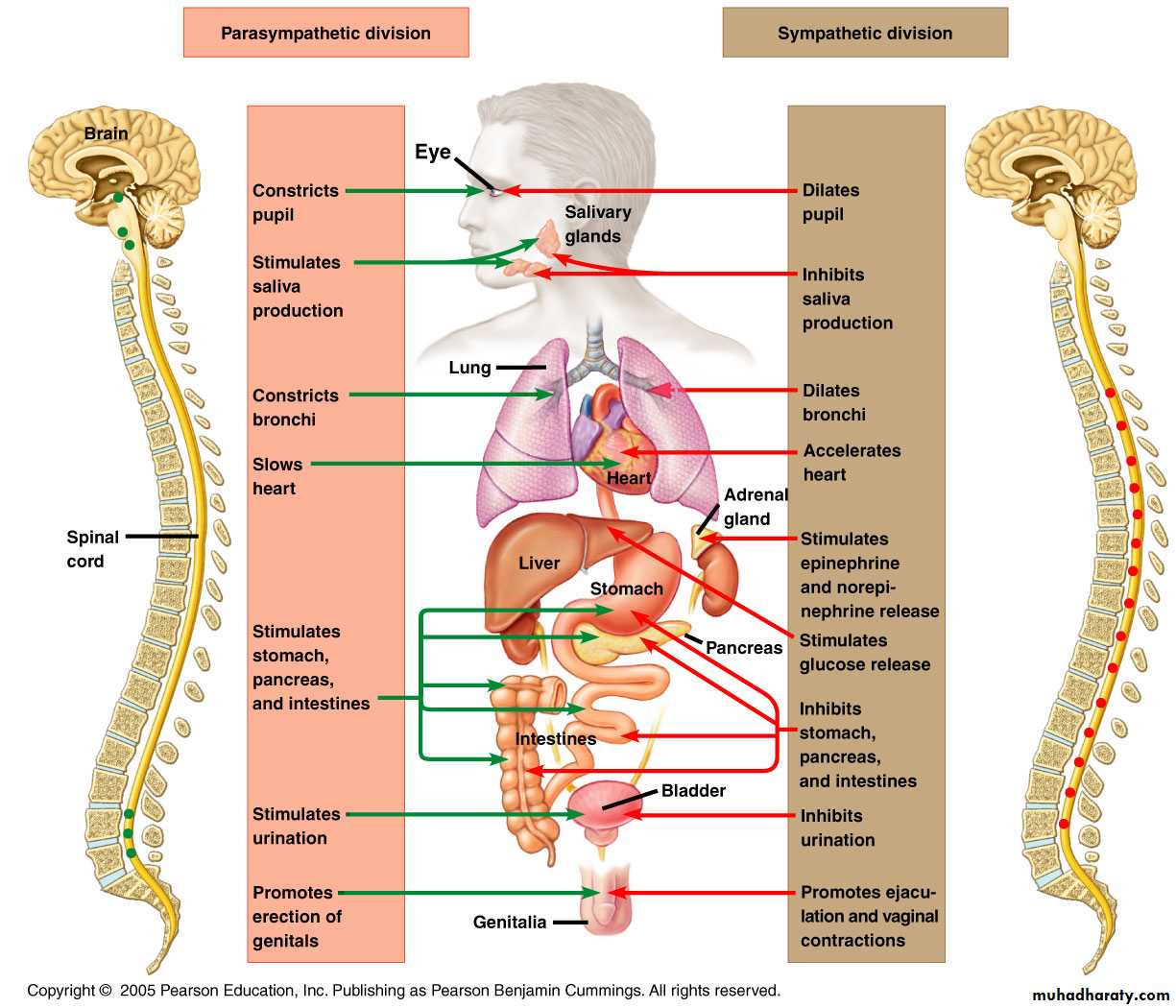
The efferent autonomic signals are transmitted to the various organs of the body through two major subdivisions called the sympathetic nervous system and the parasympathetic nervous system.
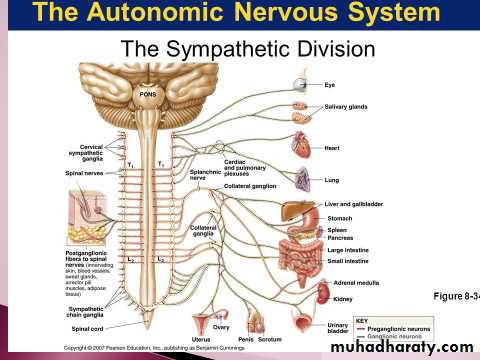
Physiologic Anatomy of the Sympathetic Nervous System
The sympathetic nerve fibers originate in the spinal cord along with spinal nerves between cord segments T-1 and L-2 and pass first into the sympathetic chain and then to the tissues and organs that are stimulated by the sympathetic nerves.Preganglionic and Postganglionic Sympathetic Neurons
The sympathetic nerves are different from skeletal motor nerves in the following way: Each sympathetic pathway from the cord to the stimulated tissue is composed of two neurons, a preganglionic neuron and a postganglionic neuron, in contrast to only a single neuron in the skeletal motor pathway.The cell body of each preganglionic neuron lies in the intermediolateral horn of the spinal cord; its fiber passes, through an anterior root of the cord into the corresponding spinal nerve. Immediately after the spinal nerve leaves the spinal canal, the preganglionic sympathetic fibers leave the spinal nerve and pass through a white ramus into one of the ganglia of the sympathetic chain.
Then the course of the fibers can be one of the following three: (1) It can synapse with postganglionic sympathetic neurons in the ganglion that it enters; (2) it can pass upward or downward in the chain and synapse in one of the other ganglia of the chain; or (3) it can pass for variable distances through the chain and then through one of the sympathetic nerves radiating outward from the chain, finally synapsing in a peripheral sympathetic ganglion.
The postganglionic sympathetic neuron thus originates either in one of the sympathetic chain ganglia or in one of the peripheral sympathetic ganglia. From either of these two sources, the postganglionic fibers then travel to their destinations in the various organs.
Segmental Distribution of the Sympathetic Nerve Fibers.
The sympathetic pathways that originate in the different segments of the spinal cord are not necessarily distributed to the same part of the body as the somatic spinal nerve fibers from the same segments. Instead, the sympathetic
fibers from cord segment T-1 generally pass up the sympathetic chain to terminate in the head; from T-2 to terminate in the neck; from T-3, T-4, T-5, and T-6 into the thorax; from T-7, T-8, T-9, T-10, and T-11 into the abdomen; and from T-12, L-1, and L-2 into the legs. This distribution is only approximate and overlaps greatly.
Physiologic Anatomy of the Parasympathetic Nervous System
The parasympathetic fibers leave the central nervous system through cranial nerves III, VII, IX, and X; additional parasympathetic fibers leave the lower most part of the spinal cord through the second and third sacral spinal nerves and occasionally the first and fourth sacral nerves. About 75 per cent of all parasympathetic nerve fibers are in the vagus nerves (cranial nerve X), passing to the entire thoracic and abdominal regions of the body.The vagus nerves supply parasympathetic nerves to the heart, lungs, esophagus, stomach, entire small intestine, proximal half of the colon, liver, gallbladder, pancreas, kidneys, and upper portions of the ureters. Parasympathetic fibers in the third cranial nerve go to the pupillary sphincter and ciliary muscle of the eye. Fibers from the seventh cranial nerve pass to the lacrimal, nasal, and submandibular glands. And fibers from the ninth cranial nerve go to the parotid gland.
The sacral parasympathetic fibers are in the pelvic nerves, which pass through the spinal nerve sacral plexus on each side of the cord at the S-2 and S-3 levels. These fibers then distribute to the descending colon, rectum, urinary bladder, and lower portions of the ureters.Also, this sacral group of parasympathetics supplies nerve signals to the external genitalia to cause erection.
Preganglionic and Postganglionic Parasympathetic Neurons.
The parasympathetic system, like the sympathetic, has both preganglionic and postganglionic neurons.
However, except in the case of a few cranial parasympathetic nerves, the preganglionic fibers pass uninterrupted all the way to the organ that is to be controlled. In the wall of the organ are located the postganglionic neurons. The preganglionic fibers synapse with these, and very, very short postganglionic fibers, a fraction of a millimeter to several centimeters in length, leave the neurons to innervate the tissues of the organ.
This location of the parasympathetic postganglionic neurons in the visceral organ itself is quite different from the arrangement of the sympathetic ganglia, because the cell bodies of the sympathetic postganglionic neurons are almost always located in the ganglia of the sympathetic chain or in various other discrete ganglia in the abdomen, rather than in the excited organ itself.
Basic Characteristics of Sympathetic and Parasympathetic Function
Cholinergic and Adrenergic Fibers— Secretion of Acetylcholine orNorepinephrine
The sympathetic and parasympathetic nerve fibers secrete mainly one or the other of two synaptic transmitter substances, acetylcholine or norepinephrine.Those fibers that secrete acetylcholine are said to becholinergic.Those that secrete norepinephrine are said to be adrenergic, a term derived from adrenalin, which is an alternate name for epinephrine.
All preganglionic neurons are cholinergic in both the sympathetic and the parasympathetic nervous systems. Acetylcholine or acetylcholine-like substances, when applied to the ganglia, will excite both sympathetic and parasympathetic postganglionic neurons. Either all or almost all of the postganglionic neurons of the parasympathetic system are also cholinergic.
Conversely, most of the postganglionic sympathetic neurons are adrenergic. However, the postganglionic sympathetic nerve fibers to the sweat glands, to the piloerector muscles of the hairs, and to a very few blood vessels are cholinergic.
Thus, the terminal nerve endings of the parasympathetic system all or virtually all secrete acetylcholine. Almost all of the sympathetic nerve endings secrete norepinephrine, but a few secrete acetylcholine. These hormones in turn act on the different organs to cause respective parasympathetic or sympathetic effects. Therefore, acetylcholine is called a parasympathetic transmitter and norepinephrine is called a sympathetic transmitter.
Two Principal Types of Acetylcholine Receptors—Muscarinic and Nicotinic Receptors
Acetylcholine activates mainly two types of receptors. They are called muscarinic and nicotinic receptors. Muscarinic receptors are found on all effector cells that are stimulated by the postganglionic cholinergic neurons of either the parasympathetic nervous system or the sympathetic system.
Nicotinic receptors are found in the autonomic ganglia at the synapses between the preganglionic and postganglionic neurons of both the sympathetic and parasympathetic systems. (Nicotinic receptors are also present at many non autonomic nerve endings—for instance, at the neuromuscular junctions in skeletal muscle.
Adrenergic Receptors—Alpha and Beta Receptors
There are also two major types of adrenergic receptors, alpha receptors and beta receptors. (The beta receptors in turn are divided into beta1 and beta2 receptors because certain chemicals affect only certain beta receptors. Also, there is a division of alpha receptors into alpha1 and alpha2 receptors.)
Norepinephrine and epinephrine, both of which are secreted into the blood by the adrenal medulla, have slightly different effects in exciting the alpha and beta receptors. Norepinephrine excites mainly alpha receptors but excites the beta receptors to a lesse rextent as well. Conversely, epinephrine excites both types of receptors approximately equally. Therefore, the relative effects of norepinephrine and epinephrine on different effector organs are determined by the types of receptors in the organs. If they are all beta receptors, epinephrine will be the more effective excitant.
Note that certain alpha functions are excitatory, whereas others are inhibitory. Likewise, certain beta functions are excitatory and others are inhibitory. Therefore, alpha and beta receptors are not necessarily associated with excitation or inhibition but simply with the affinity of the hormone for the receptorsin the given effector organ. .
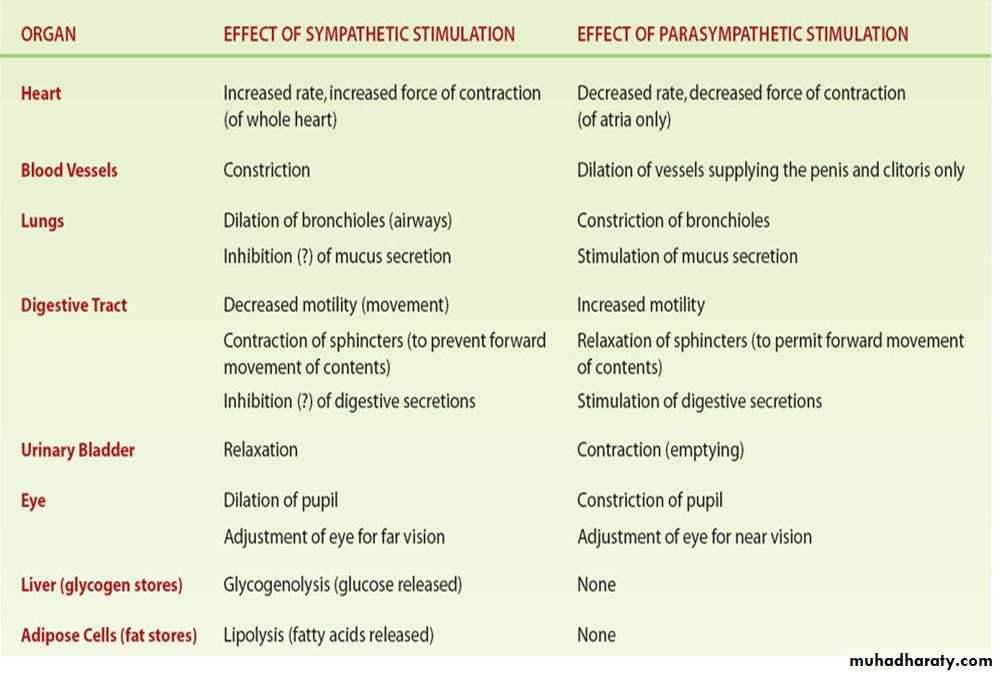
Effects of Sympathetic and Parasympathetic Stimulation on Specific Organs
Autonomic Reflexes
Many visceral functions of the body are regulated by autonomic reflexes.
Cardiovascular Autonomic Reflexes:
Several reflexes in the cardiovascular system help to control especially the arterial blood pressure and the heart rate. One of these is the baroreceptor reflex. Briefly, stretch receptors called baroreceptors are located in the walls of several major arteries, including especially the internal carotid arteries and the arch of the aorta.
When these become stretched by high pressure, signals are transmitted to the brain stem, where they inhibit the sympathetic impulses to the heart and blood vessels and excite the parasympathetics; this allows the arterial pressure to fall back toward normal.
Gastrointestinal Autonomic Reflexes.
The uppermost part of the gastrointestinal tract and the rectum are controlled principally by autonomic reflexes. For instance, the smell of appetizing food or the presence of food in the mouth initiates signals from the nose and mouth to the vagal, glossopharyngeal, and salivatory nuclei of the brain stem. These in turn transmit signals through the parasympathetic nerves to the secretory glands of the mouth and stomach, causing secretion of digestive juices sometimes even before food enters the mouth.
When fecal matter fills the rectum at the other end of the alimentary canal, sensory impulses initiated by stretching the rectum are sent to the sacral portion of the spinal cord, and a reflex signal is transmitted back through the sacral parasympathetics to the distal parts of the colon; these result in strong peristaltic contractions that cause defecation.
Other Autonomic Reflexes.
Emptying of the urinary bladder is controlled in the same way as emptying the rectum; stretching of the bladder sends impulses to the sacral cord, and this in turn causes reflex contraction of the bladder and relaxation of the urinary sphincters, thereby promoting micturition.
Also important are the sexual reflexes, which are initiated both by psychic stimuli from the brain and by stimuli from the sexual organs. Impulses from these sources converge on the sacral cord and, in the male, result first in erection, mainly a parasympathetic function, and then ejaculation, partially a sympathetic function.
“Alarm” or “Stress” Response of the Sympathetic Nervous System
When large portions of the sympathetic nervous system discharge at the same time—that is, a mass discharge— this increases in many ways the ability of the body to perform vigorous muscle activity. Let us summarize
these ways:
1. Increased arterial pressure
2. Increased blood flow to active muscles concurrent
with decreased blood flow to organs such as the
gastrointestinal tract and the kidneys that are not
needed for rapid motor activity
3. Increased rates of cellular metabolism throughout
the body
4. Increased blood glucose concentration
5. Increased glycolysis in the liver and in muscle
6. Increased muscle strength
7. Increased mental activity
8. Increased rate of blood coagulation
The sum of these effects permits a person to perform far more strenuous physical activity than would otherwise be possible. Because either mental or physical stress can excite the sympathetic system, it is frequently said that the purpose of the sympathetic system is to provide extra activation of the body in states of stress: this is called the sympathetic stress response.
Thank you