• Chronic complication of DM
Adel Gassab MohammedMD. CABMS. MSc , Specialist Endocrinologist,
College of medicine
ORCID iD: https://orcid.org/0000-0001-9084-1038.
Email: adelgassab@utq.edu.iq
• Chronic complication of DM
• Retinopathy• Nephropathy
• Neuropathy
• Foot disease
• Microvascular
• Coronary circulation
• Cerebral circulation
• Peripheral circulation
• Macro vascular
• Diabetic retinopathy
• One of the common causes of blindness in adults between 30-65 years of age
• Prevalence increases with duration of diabetes
• Almost all individual with type 1 diabetes
• Type 2 will have some degree after 20 years.
• Risk factors: long duration, poor glycemic control, hypertension, hyperlipidemia, pregnancy, renal disease, obesity, smoking
• Diabetic retinopathy
• Pathogenesis• Hyperglycemia increase retinal blood flow
• disrupt intracelllular metabolism in retinaendothelial cells & pericytes impaired vascular autoregulation, capillary hypoperfusion & closure chronic retina ischemia stimulates production of growth factor (Vascular endothelial growth factor (VEGF)further stimulates deleterious endothelial cell growth& increase vascular permeability
• Diabetic retinopathy
• Risk Factors• Long duration of diabetes
• Poor glycemic control
• Hypertension
• Hyperlipidemia
• Pregnancy
• Nephropathy/renal disease
• obesity,
• smoking
• Diabetic retinopathy
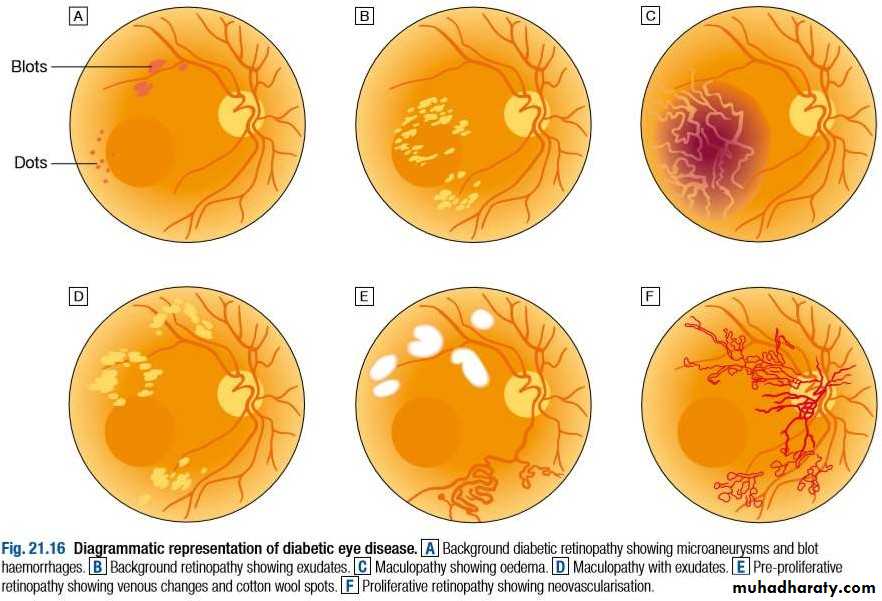
• Non proliferative
• Microaneurysm- dot
• Retinal hemorrhage- blot
• Capillary hypoperfusion
• Cotton wool spots
• Venous beading
• Intra-retinal microvascular abnormalities ( pre- proliferatives)
• Proliferative-
• growth of new blood
• vessels on retina vitrous hemorrhagefibrosis &scarringtractional retina detachment
• Clinical features
• Diabetic retinopathy
• Cystoid macular edemaincrease vascular permeability& deposition of hard exudates in central retina loss of vision• Proliferativestimulates new vessels to grow on the ant. Surface of the iris (rubeosis iridis)secondory glaucoma
• Diabetic retinopathy
• Prevention
• Glycemic, blood pressure, lipid profile controlreduce incidence & progression of DR
• Screening annual screening retinopathy (those with risk factor)
• Diabetic retinopathy
• Management• Good glycemic & BP control
• HbA1c – 53mmol/mol (7%)
• – BP- <130/80 mmHg
• Ranibizumab- diabetic macula edema
• Retinal photocoagulation
• Severe proliferative
• Severe non-proliferative retinopathy
• New vessels+ vitreous hemorrhage
• New vessels- vitreous hemorrhage
• CSMO
• F(x): treat leaking microaneurysm & areas of retinal thickening in macular area & reduce macular edema
• Destroy areas of retinal ischemia
• Reduce risk of recurrent hemorrhage• Patients should reviewed regularly
• Vitrectomy advanced diabetic eye due to type 1
• Other causes of visual loss in people with diabetes
• Cataract
• Age related macular degeneration
• Retinal vein occlusion
• Retinal arterial occlusion
• Non arteritic ischemic optic neuropathy
• glaucoma
• Diabetic nephropathy
• Cause of morbidity & mortality• Most common causes of end-stage renal failure
• About 30% patients with type 1 diabetes developed nephropathy after 20 years diagnosis
• From the outset, the risk is not equal in all patients
• Diabetic nephropathy
• Risk factors• Poor glycemic control
• Long duration of diabetes
• Presence of other microvascular complication
• Ethnicity (Asians, Pima Indians)
• Pre-existing hypertension
• Family h/o diabetic nephropathy
• Family h/o hypertension
• Diabetic nephropathy
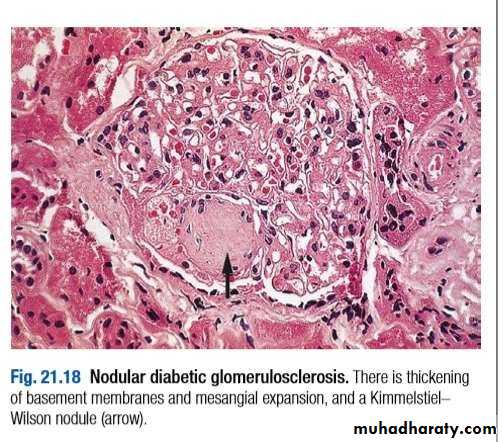
• Pathogenesis
• mesangial expansion is directly induced by hyperglycemia, perhaps via increased matrix production or glycosylation of matrix proteins.
• thickening of the glomerular basement
• membrane (GBM) occursglomerular sclerosis is caused by intraglomerular hypertension (induced by dilatation of the afferent renal artery or from ischemic injury induced by hyaline narrowing of the vessels supplying the glomeruli).
• Diabetic nephropathy
• Diagnosis & screening• Microalbuminuria
• marcoalbuminuria
• Who to screen
• Patients with type 1 diabetes annually from 5 years after diagnosis
• Patients with type 2 diabetes anually from time of diagnosis
• Early morning urine measured for albumin:creatinine ratio, Microalbuminuria present if
• Male ACR 2.5-30 mg/mmol creatinine
• Female ACR 3.5-30mg/mmol creatinine
• Elevated ACR followed by repeat test
• Microalbuminura establish if 2 out of 3 tests positive
• Diabetic nephropathy
• Management
• Reduce risk of progression of nephropathy & CVS disease
• Aggressive reduction of BP
• Aggressive CVS risk factor reduction
• Type 1-ACEI-reduction of BP
• Type 2-ARB
• Blockade of renin angiotensin 2 mediated vasoconstriction of efferent arterioles in glomeruli dilatation of these vessels decrease glomeruli filtration pressure decrease hyperfiltration & protein leak
• CI : renal artery stenosis
• Electrolyte & renal f(x) should be check
• Alternatives: diltiazem, verapamil
• Renal replacement therapy
• Renal transplantation
• Pancreatic transplantation
• Diabetic neuropathy
• Mainly manifest in the peripheral nervous system.• Causes substantial morbidity & mortality
• Diagnosed base on clinical sign & symptoms after the exclusion of all causes neuropathy.
• Affect 50-90% of patients with diabetes, of those 15-30% having painful diabetic neuropathy.
• Prevalence –duration of diabetes & degree of metabolic control.
• Diabetic neuropathy
• Pathogenesis
• Occurs secondary to metabolic disturbance.
• Pathological features:
• Axonal degeneration of both myelinated+unmyelinated fibres
• thickening of schwann cell basal lamina
• pacthy segmental demyelination
• abnormal intraneural capillaries
• Diabetic neuropathy
• Classification• somatic
• Polyneuropathy
• Symmetrical- mainly sensory & distal
• Asymmetrical-mainly motor& proximal
• (amyotrophy)
• Mononeuropathy ( mononeuritis multiplex)
• visceral
• Cardiovascular sudomotor
• Gastrointestinal vasomotor
• Genitourinary pupillary
• Diabetic neuropathy
• Clinical features
• Symmetrical sensory
• polyneuropathy
• Asymtomatic
• Mc signs :
• diminished perception of vibration sensation distally
• Gloves & stocking impairment
• Loss of tendon reflexes in LL
• A diffuse small fibre neuropathy altered perception of pain & temperature, a/w symptomatic autonomic neuropathyfoot ulcers & Charcot neuroarthropathy
• Symtomatic
• Sensory abnormalities
• predominant
• Paraesthesiae in the feet
• Pain the LL
• Burning sensation in the soles of
• feet
• Cutaneous hyperaesthesiae
• Abnormal gait- wide based
• a/w numbness in the feet
• Callus skin at pressure point
• Electrophysiological test-slow conduction both motor & sensory
• Test vibration & thermal
• thresholds- abnormal
• Daibetic neuropathy
• Asymmetrical motor diabetic neuropathy
• Called as diabetic amyothrophy
• Progressive weakness & wasting of proximal muscles of LL
• Severe pain –ant. Aspect of legs (hyperaesthesiae & paraaesthesiae)
• Loss of weight ( neuropathic cachexia)
• Tendon reflexes –absent
• Extensor plantar responses +++
• CSF protein –raised
• Management-mainly supportive
• Recovery within 12 month, some deficit may permanent
• Diabetic neuropathy
• Mononeuropathy• Motor or sensory function affected within a single peripheral or cranial nerve
• Severe & rapid in onset, but eventually recover
• Most common CN affected : 3rd& 6th (diplopia)
• Nerves compression palsies most commonly occur median nerve (carpal tunnel syndrome), less common ulnar nerves
• Lateral popliteal nerves compression foot drop
• Diabetic neuropathy
• Autonomic neuropathy• Not necessarily associated with peripheral somatic neuropathy.
• Parasympathetic / sympathetic nerves may be predominantly affected in one/ more visceral system.
• Cardiovascular
• Postural hypotension
• Resting tachycardia• Fixed heart rate
• Gastrointestinal
• Dysphagia• Abdominal fullness, nausea , vomiting
• Nocturnal diarrhea + fecal incontinence
• constipation
• Genitourinary
• Difficulty in micturition, urinary incontinence, recurrent infection• Erectile dysfunction & retrograde ejaculation
• sudomotor
• Nocturnal sweat w/o hypoglycemia• Gustatory sweating
• anhydrosis
• vasomotor
• Feet feel cold
• Dependent edema• Bullous formation
• Pupillary
• Decreased pupil size• Resistance to mydriatics
• Delayed/ absent reflexes to light
• Diabetic neuropathy
• Pain ¶esthesia from peripheral• somatic neuropathies
• Intensive insulin therapy
• Anticonvulsants (gabapentin, pregabalin, carbamazepin, phenytoin)
• Tricyclic antidepressants
• (amytriptyline, imipramine)
• Other antidepressant(duloxetine)
• Opiates ( tramadol, oxycodone)
• Membrane stabilisers (
• mexiletine, IV lidocaine)
• Antioxidant (α-lipoic acid)
• Management Postural hypotension
• Support stockings
• Fludrocortison
• NSAIDS
• α-adrenoceptor agonist (midodrine)
• Diarrhea
• Loperamide
• Broad spectrum antibiotiics
• Clonidine
• octreotide
• Diabetic neuropathy
• Gastroparesis
• Dopamine antagonist ( metoclopromide, domperidone)
• Erythmycin
• Gastric pacemaker, percutaneus enteral feeding
• Constipation
• Stimulant laxatives
• Erectile dysfuction
• Phosphodiesterase type 5 inhibitors (sildenafil, vardenafil, tadalafil)
• Dopamine agonist (apomorphine)
• Prostalglandin E1 ( alprostadil)
• Vacuum tumescence devices
• Psychological counselling
• Atonic bladder
• Intermittent self catheterization
• Excessive sweating
• Anticholinergic drugs ( propantheline, poldine,oxybutinin)
• Clonidine
• Topical antimuscurinic agents (glycopyrrolate cream)
• Macrovascular Disease Due to Diabetes
• greater risk for heart attacks, strokes and poor circulation to the legs.• People with diabetes can have problems with their blood vessels. It is common for the arteries to get narrow. This can lead to disorders all through the body.
• The Metabolic Syndrome
• This is a group of problems:
• too much belly fat
• high blood pressure
• high blood fats (“triglycerides”)
• low HDL (“good”) cholesterol
• high blood sugar
Each of the problems listed above raises the risk of CHD (coronary heart disease). And they may play roles in strokes and PAD (peripheral artery disease). High insulin levels and a large waist boost the risk of death from CHD.
• Coronary Heart Disease
• Some arteries carry blood to the heart. In CHD, these arteries get narrow. People who have diabetes are at risk for CHD. Women who have diabetes are at high risk for heart attacks.• for chest pain (”angina”). And they are at risk for heart attacks. Diabetes is just one risk factor for CHD. There are other risk factors:
• smoking
• high blood pressure
• high LDL (“bad”) cholesterol
• low HDL (“good”) cholesterol
• people with type 2 diabetes and no history of CHD
• people without diabetes who had already suffered a heart attack• Stroke
• high A1C levels (high blood sugar)• long history of diabetes
• High blood sugar may raise stroke risk in different ways. It may:
• allow cholesterol to build up faster along arteries to the brain
• promote blood clots
Another risk factor for stroke is high blood pressure. Many people with diabetes have high blood pressure.
• Peripheral Artery Disease
• Some arteries carry blood to the legs. In PAD, these arteries get narrow. It’s marked by leg pain with exercise that stops quickly with rest. This is a sign of poor circulation. Poor circulation can slow the healing of injuries to the skin. This may lead to sores on feet and legs.• Diabetes and smoking each raise the risk of PAD. A person with diabetes who smokes has an even greater risk. People with PAD should deal with the same risk factors noted for CHD. These are:
• smoking
• high blood pressure
• high LDL (“bad”) cholesterol
• low HDL (“good”) cholesterol
If you have very bad PAD you may need surgery. This will bypass the blocked blood vessels. Or you can have a surgery called angioplasty to treat PAD. A small balloon is used to open up the narrowed artery.
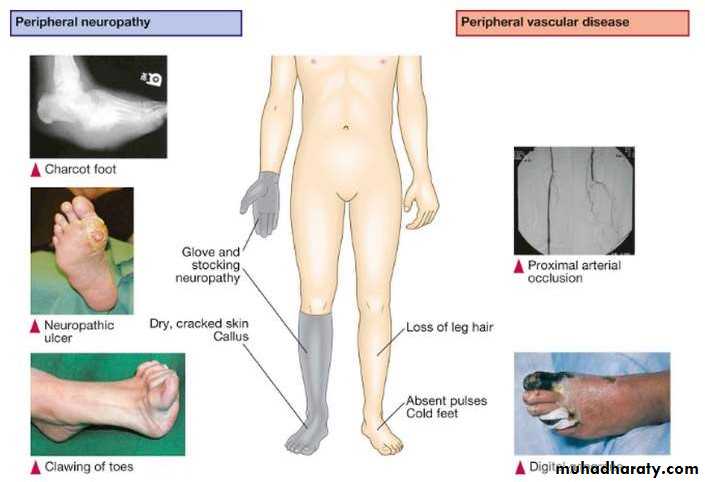
• Diabetic foot
• Aetiology• Foot ulceration
• Trauma in the presence of neuropathy/ peripheral vascular disease + infection 2’ to disruption of protective epidermis
• Ulcer develops at site of plaque of callus skin beneth tissue necrosisbreaks through to surface
• Charcot neuroarthropathy
• Progressive condition affecting joints & bones of foot
• Earlt inflammationjoint dislocationsubluxationpathological fracture of foot debilitating deformity
• Diabetic foot
• Pathophysiology
• Unperceived trauma progressive destruction & increased blood flow mismatch of bone destruction & synthesis
• Diabetic foot
• Clinical features• Diabetic foot
• Managements• Foot ulcer
• Referred to multidiciplinary foot team
• Treatment:
• debridement of dead
• tissue
• Prompt treatment with antibiotics, pressure relief using dressing
• Neurosichemic –vascular assessment often carried outultrasound/angiograp hy
• Gangrene- amputation
• Charcot foot
• Investigation:MRI
• Treatment:
• Immobilisation
• Avoid weight bearing on
• affected foot
• References
• http://emedicine.medsc ape.com/article/238946
• -overview#a0104• http://emedicine.medsc ape.com/article/237378
• -overview#a0104