• Lec : 12
• Medicaments used in treatment of periodontal diseases• UNIVERSITY OF MOSUL
• COLLEGE OF DENTISTRY
• By:
• Dr.Ghayath Aljawady
• B.D.S, M.Sc., Ph.D in periodontics
• 2020-2021
• Department of:
• Oral and Maxillofacial surgery / Periodontics unit
• Department of:
Dental plaque (D.P)
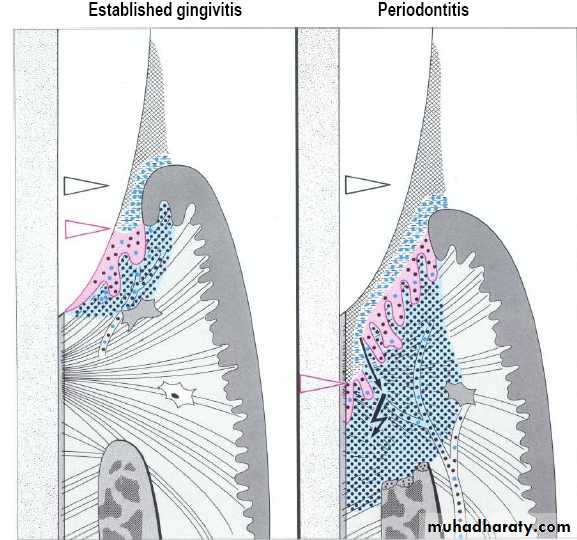
Accumulation of D.P. induce inflammatory response in Gingiva that may spread to connective tissue and bone.
So, plaque control measures aimed inhibition of plaque formation or reducing at regular intervals amount of plaque to a level at and below which no inflammatory disease develops.
Non-Specific & Specific Plaque Theories
Non-specific plaque theoryLarge no. of M.O. responsible for initiation & progression of p.d. disease (non-specific p. theory)
So mechanical & chemical plaque control aimed elimination of entire plaque mass.
Support this theory control of plaque accumulation by mechanical debridement & O.H. measures, induce control of disease inspite of direction toward specific p. theory.
Specific p. theory
Only certain plaque is pathogenic & its pathogenicity depend on presence or in specific M.O.So if plaque contain pathogenic m.o. result in p.d. disease & if not no p.d. disease occur.
That is why patient with plaque & gingivitis not develop to p.d. (contained Gingivitis).
Also patient with p.d. show site specificity in pattern of disease as some sites were disease free while other showed advanced disease in presence of uniform host response.
Because of ability to isolate p.d. m.o. (improve sampling of subg. Plaque & culturing media).
More acceptance of such hypothesis especially after recognition of A.a. as pathogen in LAP.
One or few m.o. within p. mass constitute the etiological factors
So antimicrobial drug should have potential to eliminate pathogenic m.o. only.
But only few m.o. identified as pathogen & satisfy kochs postulate among more than 300 species of normal inhabitants of oral cavity.
Kochs postulate
Classic criteria by which m.o. can be judged to be a causative agent in human infectionsCausative agent must ;
1- Be routinely isolated
2- Be grown in pure culture
3- produce similar disease when inoculated into susceptible laboratory animals
4- Be recovered from lesions in a diseased animal.
In the P.d.disease the problems are ;
1-inability to culture all organism associated with disease (as many oral spirochetes).2-difficulty inherent in defining & culturing sites of active disease.
3-lack of good animal model system for study of p.d.
Roll of p. control measures in prevention of gingivitis & its conversion to p.dontitis
• Complete elimination by chemical & mechanical means.• or
• Reduction below certain threshold levels at which health is maintained.
• or
• Alteration of microbial composition by introduction of non-virulent antagonist to subg. pathogen thereby replace virulent strain.
• or
• Prevent adhesion of bacteria to tooth sur. through change in chemistry of tooth sur.( interference with pellicle formation & initial adherence to tooth surface).
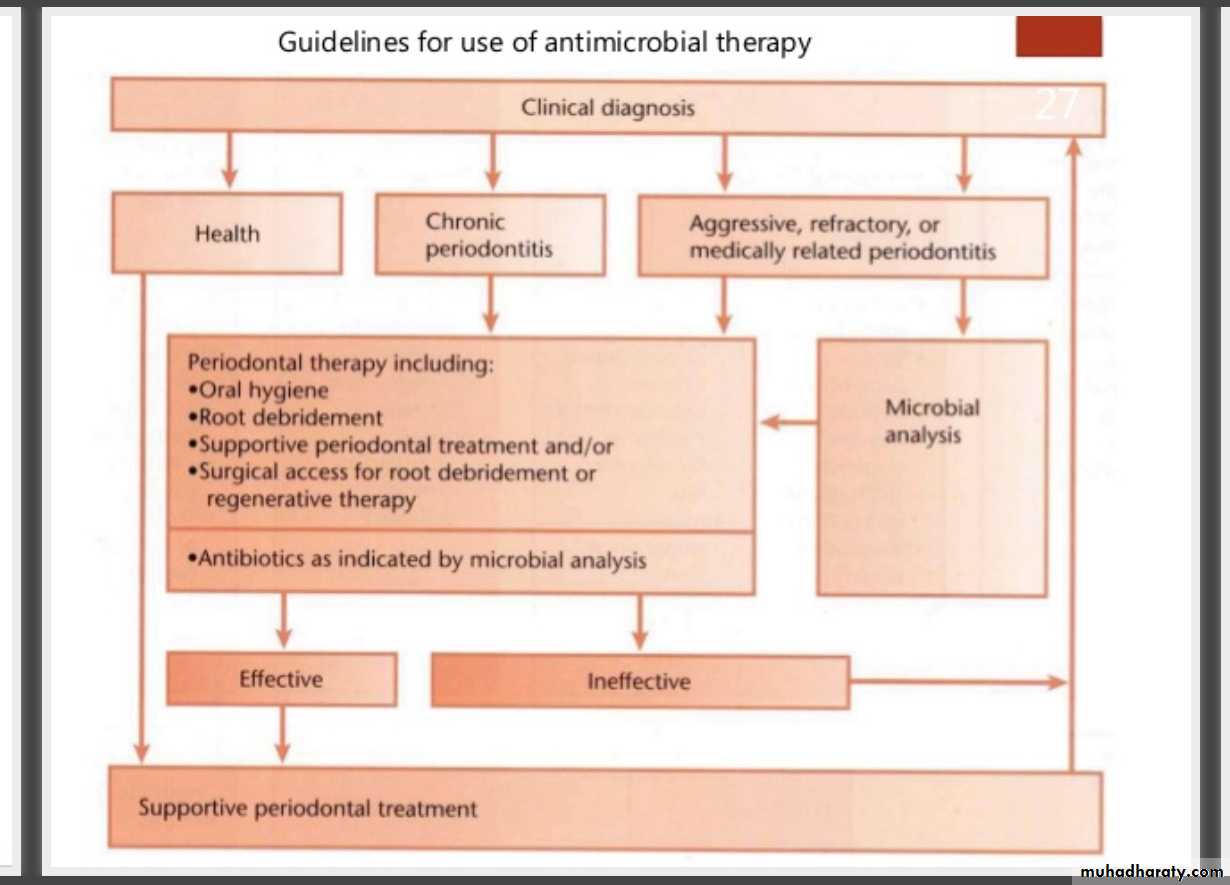
Antibiotics
Antibiotics are drugs that kill or stop the multiplication of bacterial cells at concentrations that are relatively harmless to host tissues, and therefore can be used to treat infections caused by bacteria.
Antibiotics are just one group of antimicrobial agents, which also comprise antiviral, antifungal, and antiparasitic chemicals.
Systemic antibiotics were used as adjuncts to scaling and root planing, improvements were observed in the attachment levels of patients with chronic and aggressive periodontitis, although patients with aggressive periodontitis experienced greater benefits.
Penicillin
The first antibiotics used in periodontal therapy were mainly systemically administered penicillins.The choice was initially exclusively based on empirical evidence. Penicillins and cephalosporins act by inhibition of cell wall synthesis.
They have a narrow spectrum of activity and are bactericidal. Among the penicillins, amoxicillin has been favored for treatment of periodontal disease because of its considerable activity against several periodontal pathogens at levels achievable in gingival fluid.
Tetracycline
(Tetracycline–HCl , minocycline, and doxycycline) became popular in the 1970s due to its broad‐spectrum antimicrobial activity and low toxicity.The tetracyclines, clindamycin, and macrolides are inhibitors of protein synthesis. They have a broad spectrum of activity and are bacteriostatic.
Systemic administration of tetracycline cause arrest of bone loss( aid bone regeneration by removal of m.o.) & slight alteration of composition of p. microbiota
In addition to their antimicrobial effect, tetracyclines are capable of inhibiting collagenase. This inhibition may interfere with tissue breakdown in periodontal disease.
Clinical uses:
1-adjunct in treatment of LAP.
2-Arrest bone loss and suppress A. actinomycetemcomitans levels in conjunction with scaling and root planing.
Dose: 250 mg four times daily.
Metronidazole
The nitro‐imidazoles (metronidazole and ornidazole) and the quinolone antibiotics (e.g. ciprofloxacin) act by inhibiting DNA synthesis.
Metronidazole is known to convert into several short lived intermediates after diffusion into an anaerobic organism.
metronidazole is active specifically against the obligatory anaerobic part of the oral flora, including P. gingivalis and other black‐pigmenting Gram‐negative organisms, but not A. actinomycetemcomitans, the latter being a facultative anaerobe.
Metronidazole
Its combination with amoxicillin given for patients with aggressive & advanced chronic p.d.to induce synergistic effect lead to complete elimination of A.a. for long period (50% harbored A.a. after 1y.)Bactericidal effect
cant be used for patient with CNS disorder, blood dyscrasias (prolong prothrombine time) & 1st trimester of pregnancy.
Clindamycin
Effective against anaerobic bacteria ,in situation in which patient allergic to p.Used in refractory p.d.150 mg, twice daily for 10 days or 300 mg twice daily for 8 days.
Side effect; pseudomembranous colitis ,diarrhea or cramping are indication of such problem.
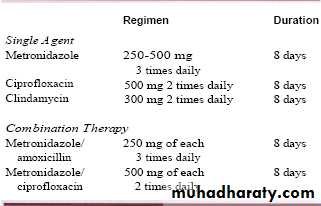
Common AB regimens used in treatment of p.d.disease
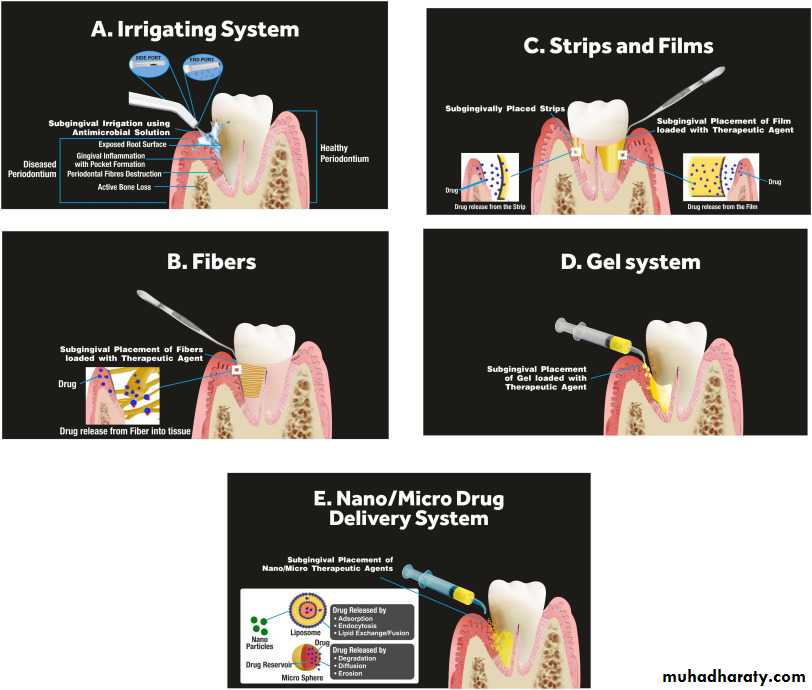
Local delivery of AB
By targeting an antimicrobial to infected sites
& sustaining its localized concentration
at effective levels for sufficient time
while concurrently induce minimal or no
side effects
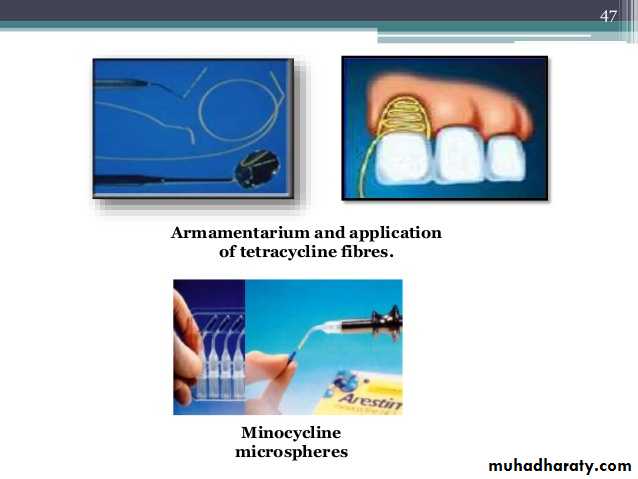
Tetracycline-containing fibers(actisite)
Fiber with diameter 0.5 mm contain tetracycline (12.7mg/9 inches) packed into p.d.p.Its well tolerated by oral tissue & for 10 days it sustains tetracycline conc. exceeding 1300mg/ml
No change in AB resistant to tetracycline was found.
Disadvantage ;take long time for placement( 10min./tooth) & need for 2nd appointment to remove fiber.
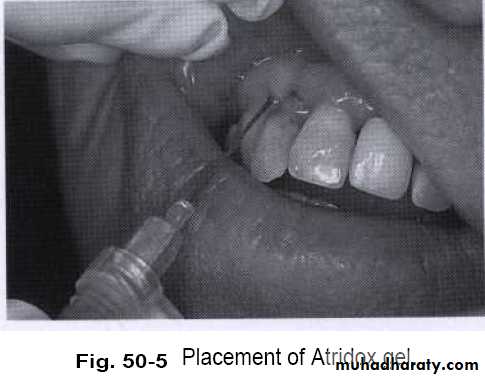
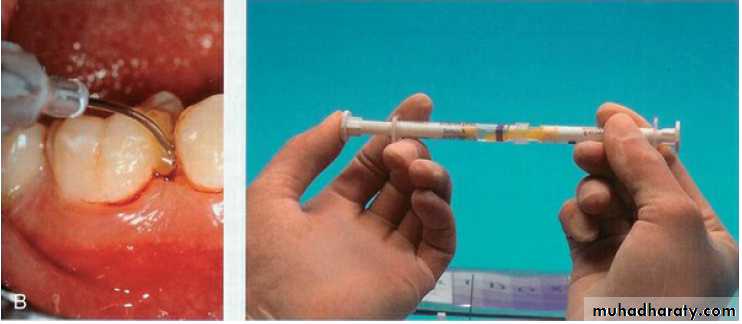
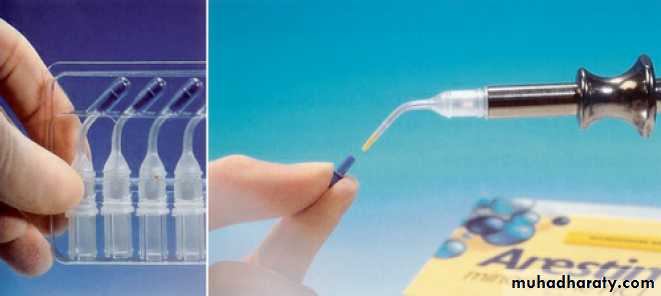
Subg.delivery of doxycycline (Atridox)
Gel system that incorporates
the AB doxycycline(10%)in syringeable gel system.
Accepted by ADA.
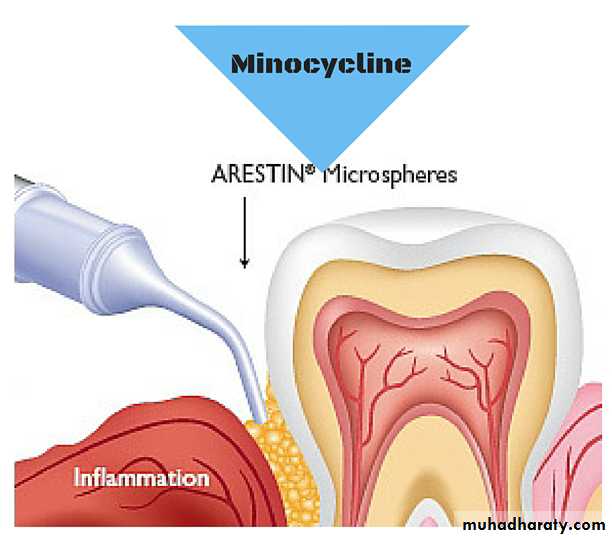
Subgingival delivery system for minocycline(Arestin)
Syringeable gel suspensiondelivery formulation
that deliver 2% minocycline HCL
to p.d.p.
Combination antimicrobial drug therapy
Since the subgingival microbiota in periodontitis often harbors several putative periodontopathic species with different antimicrobial susceptibility, combination antimicrobial drug therapy with a wider spectrum of activity than a single agent may be useful.Some combinations of drugs have a synergistic action against target organisms, allowing lower doses of the single agents to be used. A synergistic effect against A. actinomycetemcomitans has been noted in vitro between metronidazole and its hydroxy metabolite and between these two compounds and amoxicillin.
Anti-bacterial Agents
Chlorhexidine digluconate (chx)Mouthrinsing with 10 ml of 0.2% solution of chx twice daily produced a plaque reduction of 45-61% & can safely be used for extended period of time with no reduction of bacteria sensitivity to chx
0.12% chx effective also as anti plaque agent.
Substantivity & mechanism of action
Chx adsorb to surface of oral tissue including teeth & slowly released in active form ,about 30% of 10ml will bind (70% spiting)Cationic chx molecule bind to anionic component like free sulfates, carboxyl & phosphate groups of pellicle thereby reduce adsorption of protein to tooth required for formation of D.P.
Coating salivary bacteria with chx molecules also alter mechanism of adsorption to tooth
Chx molecules bound to Surface proteins will be released in active form in 8-12h.with low conc. of chx can still be recovered after 24h.
Side effects
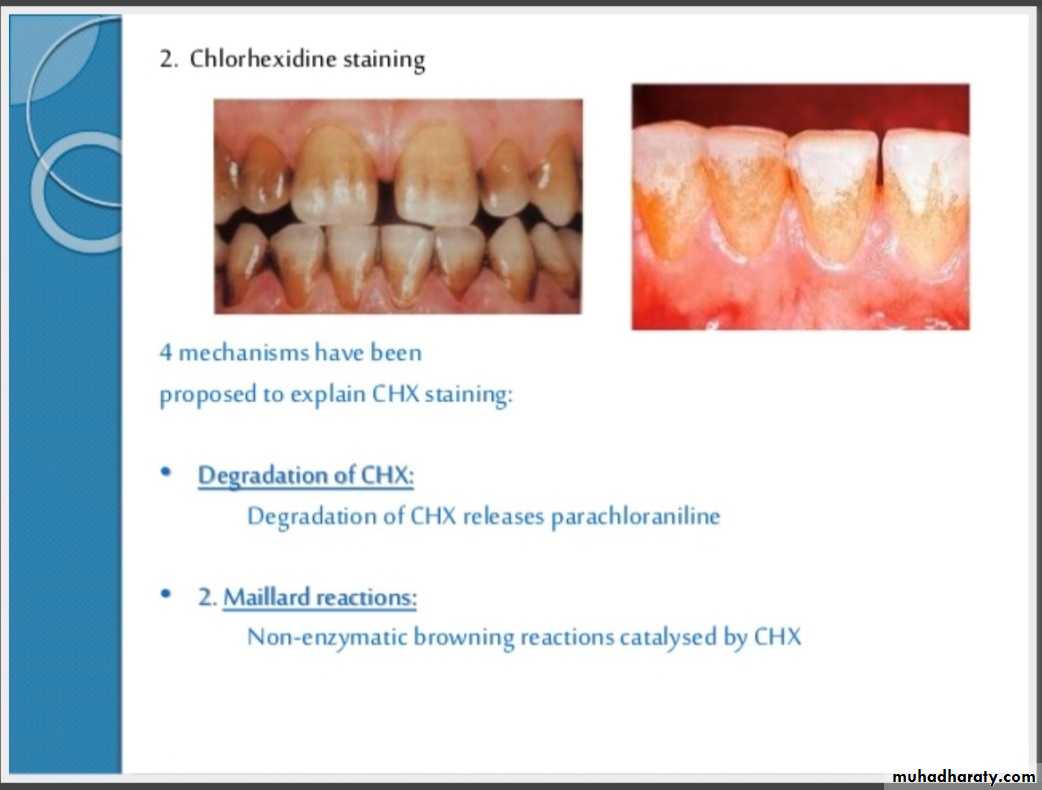
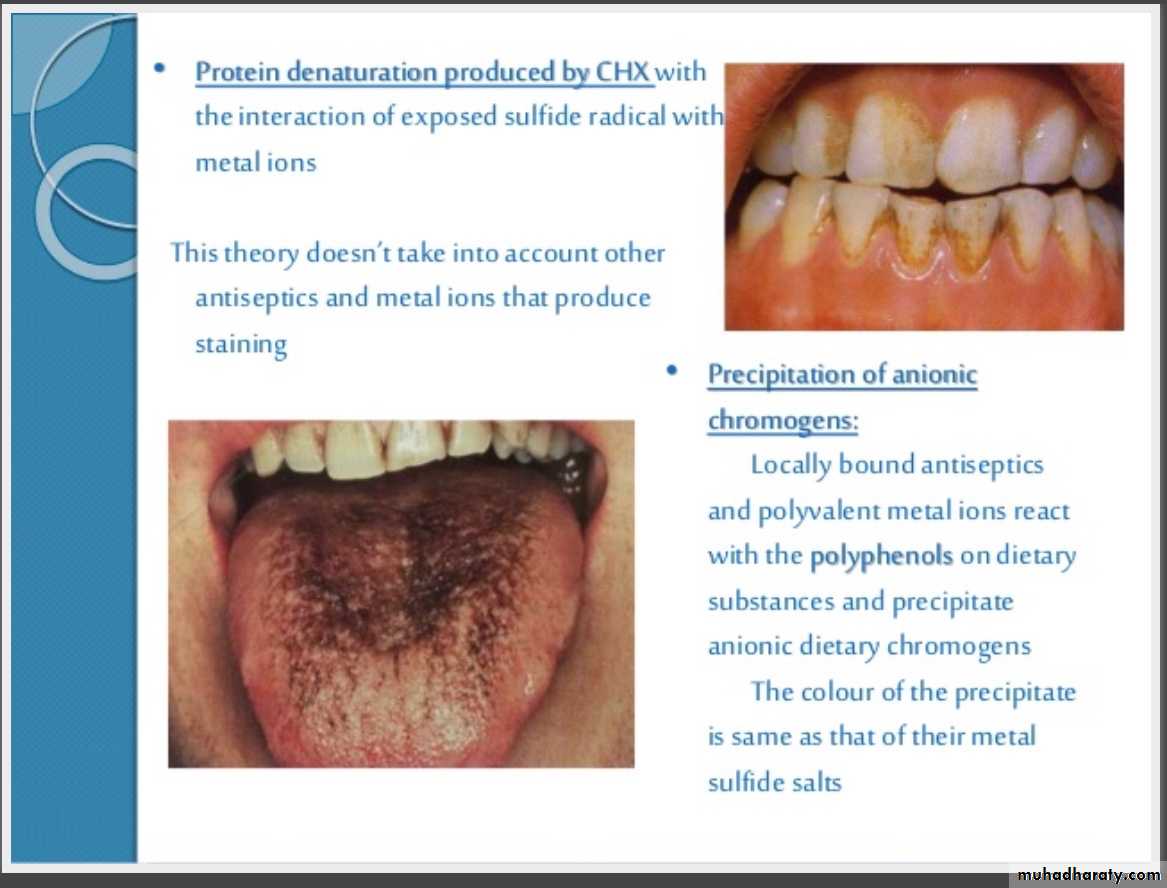
1- formation of extrinsic yellow-brown stain (vary from individual to other & depend on conc.)
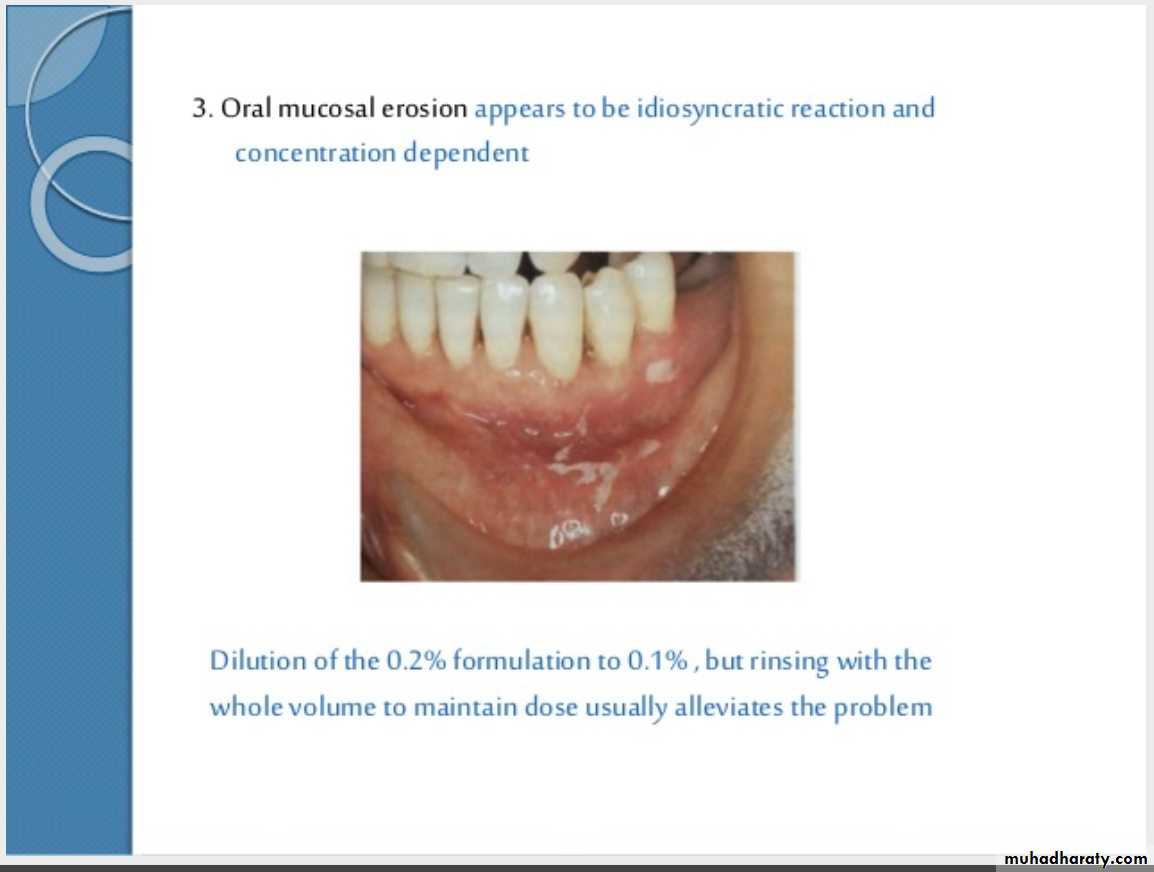
2- desquamation & painful mucosal lesions (high conc.)
3- impairment of salty taste perception (transient)
4- ascending parotitis (rare)
5- disturbance of wound healing (high conc.)
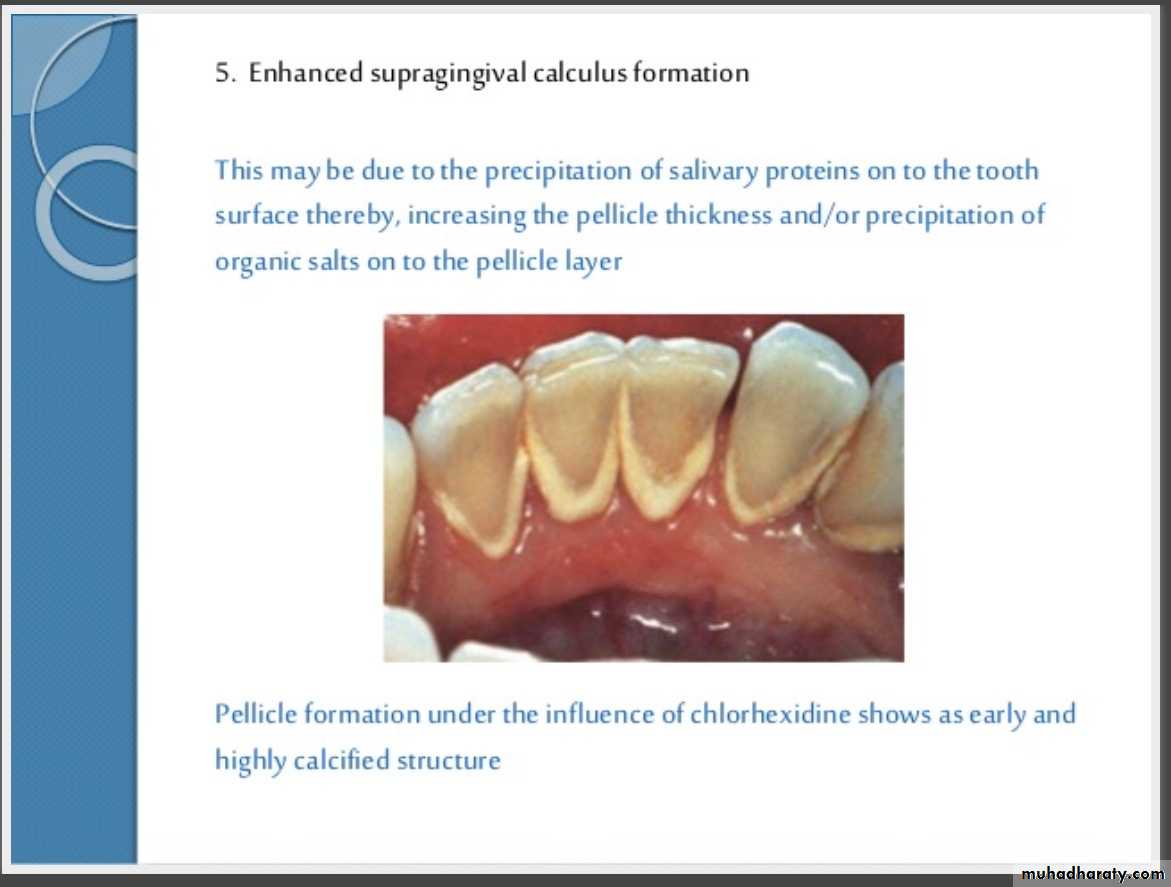
6-Enhanced supragingival calculus formation.
Clinical applications
Mouth rinses;2 daily rinses for 30-45 sec. with 10ml of 0.2% chx & advise subject not to rinse ,eat or drink for 1/2h. & rinsing sh.be done 1/2h after brushing
Irregators;
400ml of 0.02% one daily as adjunctive to mechanical p. control
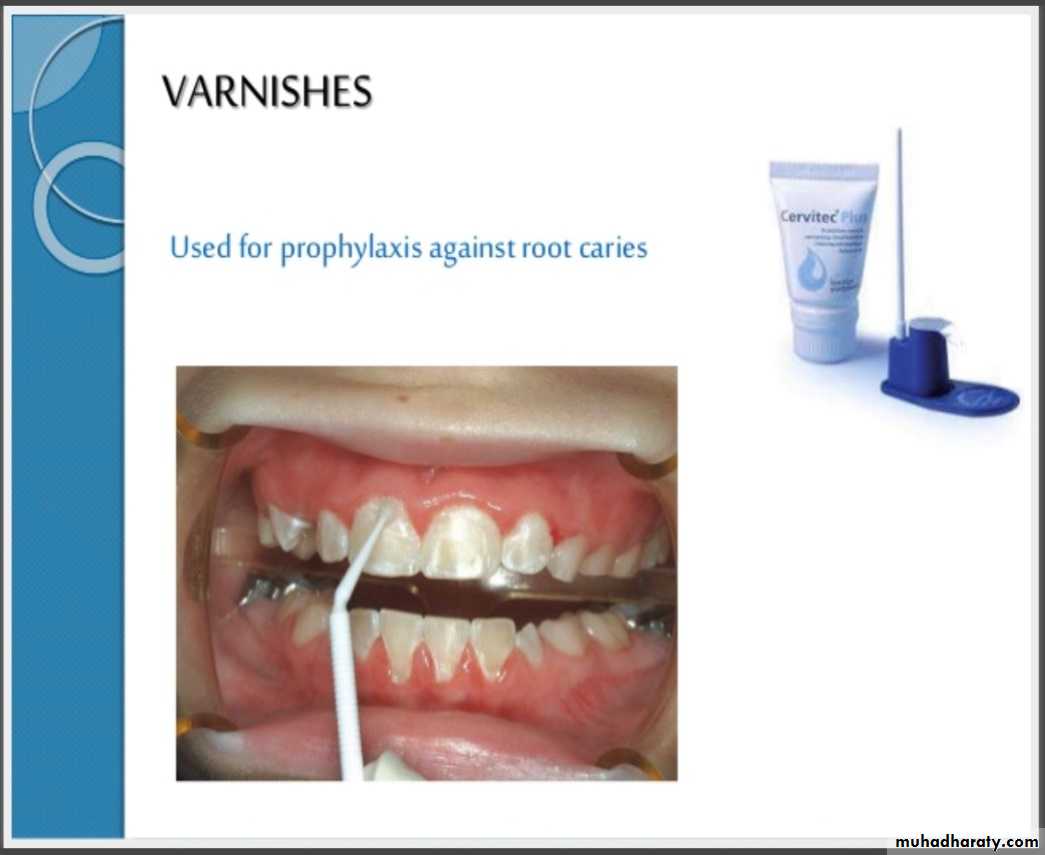
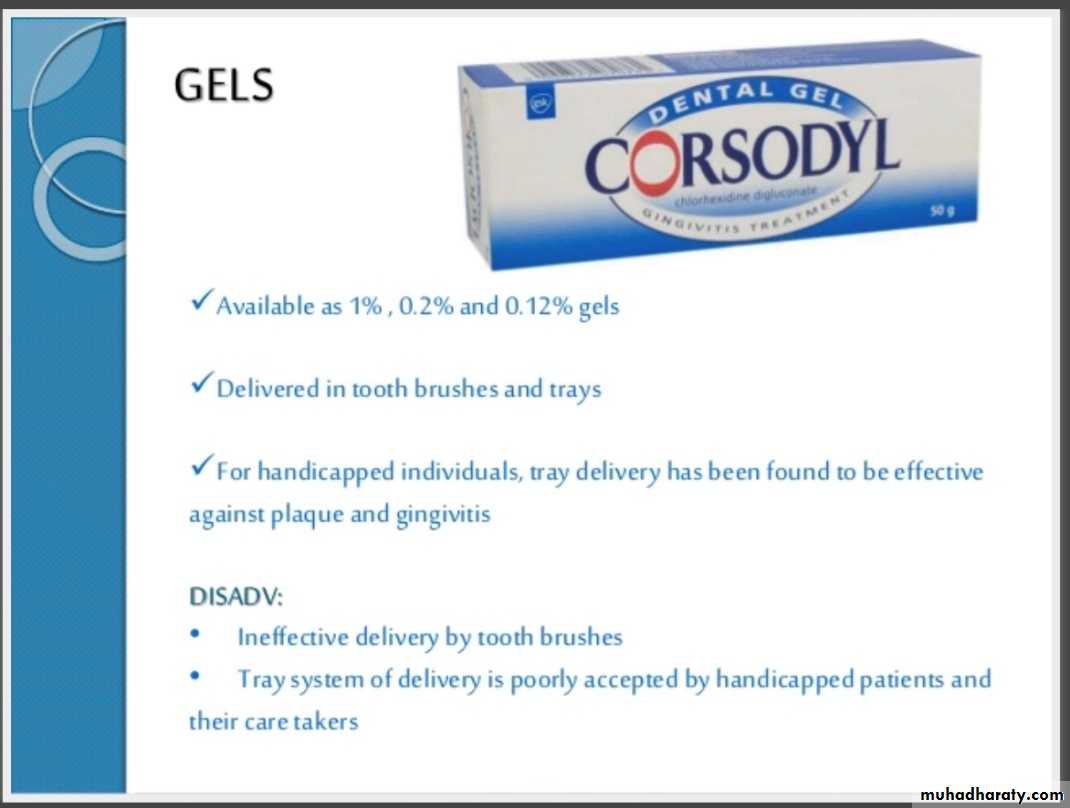
Gels
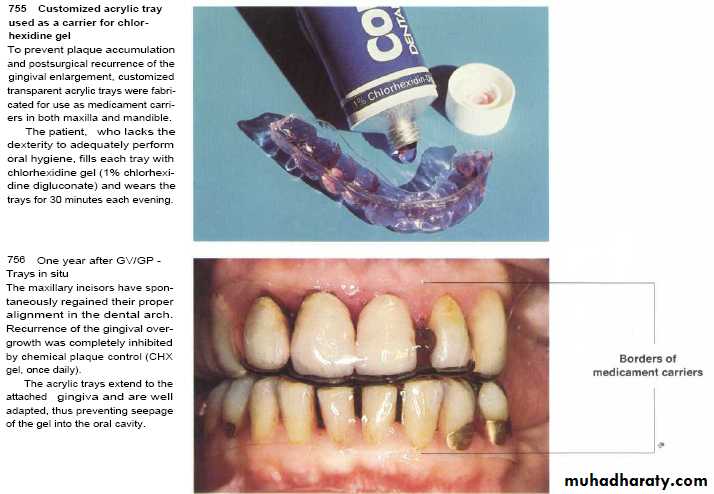
applied for 5min.once or twice daily on tray or stint effective in denture stomatitis & oral candidiasis & for handicapped3 daily application of 1% gel for several weeks reduce severity & duration of aphthus ulceration
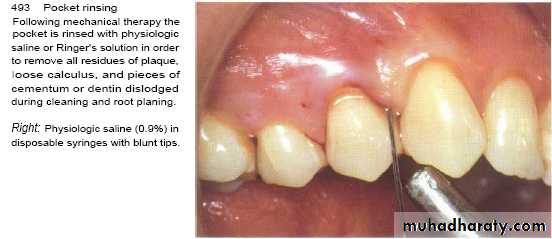
Professional irrigation
by using syringe with blunt needle to enhance result obtained with S & RP each recall visit.
Its effect is by washout only irrigation combined with RP induce no adjunctive benefit.
Chlorhexidine gluconate in a gelatin chipSeveral attempts have been made to develop local delivery devices for the subgingival application. PerioChip , a degradable gelatin chip containing 2.5 mg chlorhexidine, is the most extensively tested delivery device of this category .
Chlorhexidine Chip
The chlorhexidine chip is a small chip (4.0 × 5.0 × 0.35 mm) that contains 2.5 mg of the active ingredient chlorhexidine gluconate in a resorbable, biodegradable matrix of hydrolyzed gelatin that is cross-linked with glutaraldehyde and packaged in individual foil containers.
The chlorhexidine chip is placed into the pocket directly from the foil container using a forceps.
The chip is biodegradable and does not require removal, but dental floss should be avoided for 10 days to avoid dislodging it.
Doxycycline Gel
Doxycycline gel is a subgingival, controlled-release delivery product composed of a two-syringe mixing system.When mixed, the product is a viscous liquid of 500 mg, which contains 50 mg (10%) of doxycycline hyclate.
Doxycycline gel is indicated for the treatment of chronic adult periodontitis for a gain in clinical attachment, reduction in probing depth, and reduction of bleeding on probing.
The gel has been reported to release doxycycline in the GCF over 7 days. The doxycycline gel is biodegradable and does not require removal.
The pocket contents are then covered with a periodontal dressing or a cyanoacrylate dental adhesive.
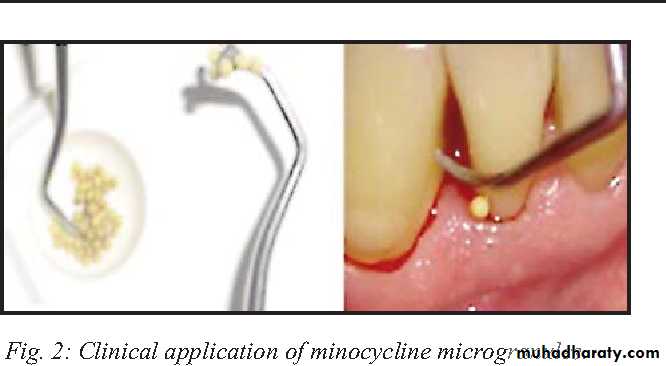
Minocycline Microspheres
The minocycline microspheres product is a subgingival, controlled release delivery system containing the antibiotic minocycline hydrochloride incorporated into a bioresorbable poly(glycolide-co- D,L-lactide) polymer in unit-dose cartridges.Minocycline microspheres are indicated as an adjunct to SRP for the reduction of pocket depth in patients with adult periodontitis and as part of a periodontal maintenance program, which includes good oral hygiene and SRP
Patients should avoid hard or sticky foods at the treated teeth for 1 week and interproximal cleaning devices for about 10 days.
Neither a periodontal dressing nor an adhesive is needed.
Other Anti-bacterial Agents
H2o2
Oxidizing agent induce 28% reduction as it consider O2 liberating agent that affect growth of anaerobic m.o.
3-10% solution for topical application used to clean wound
0.3-0.5% rinsing solution for p.d. pocket rinsing & initial therapy for NUG
Side effect; tissue damage with long term use ,emphysema if applied under pressure, hairy tongue
- Enzymes.
- Fluoride.- Essential oil mouth rinse and phenolic compound.
- Herbal extract.
- Other antiseptics like: Povidone iodine 1% and Hexetidine 0.1%.