UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYBy :Dr Ali Moayid
2020-2021
Department of
Conservative Dentistry
5th YEARs
Endodontic MicrobiologyROUTES OF ROOT CANAL INFECTION
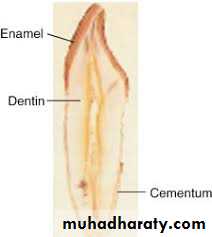
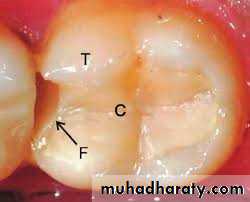
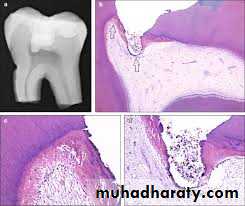
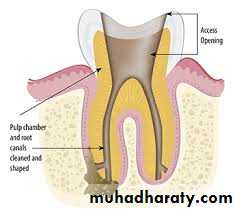
Under normal conditions, the pulpodentin complex is sterile and isolated from oral microbiota by overlying enamel, dentin and cementum.Whenever dentin is exposed, the pulp is put at risk of infection as a consequence of the permeability of normal dentin
dictated by its tubular structure
In the event that the integrity of these natural layers is breached (e.g., as a result of caries, trauma-induced fractures and cracks, restorative procedures, scaling and root planning, attrition, abrasion) or naturally absent (e.g., because
of gaps in the cemental coating at the cervical root surface) the pulpodentin complex is exposed to the oral environment .
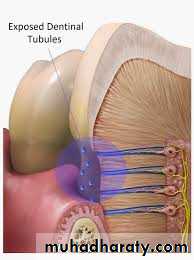
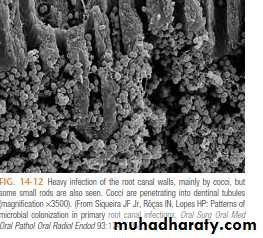
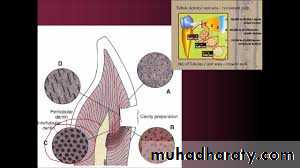
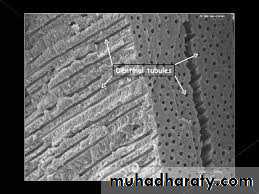
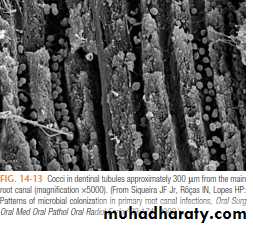
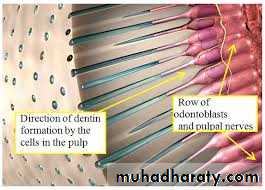
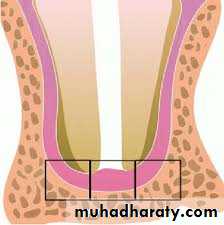
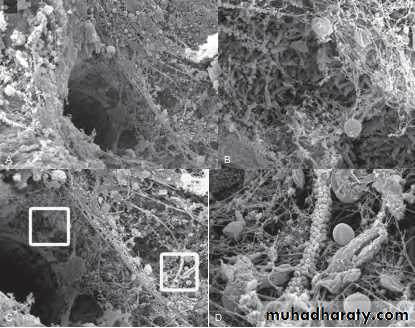
Dentinal tubules traverse the entire width of the dentin and have a conical conformation, with the largest diameter located near the pulp (mean, 2.5 µm) and the smallest diameter in the periphery, near the enamel or cementum (mean, 0.9 µm) The smallest tubule diameter is entirely compatible with the cell diameter of most oral bacterial species, which usually ranges from 0.2 to 0.7 µm.
it has been demonstrated that bacterial invasion of dentinal tubules occurs more rapidly with a non vital
pulp than with a vital pulp
• With a vital pulp, outward movement of dentinal fluid and the tubular contents (including odontoblast processes, collagen fibrils, and the sheath like lamina limitans that lines the tubules) influence dentinal permeability and can conceivably delay intratubular invasion by bacteria.
• Other factors such as dentinal sclerosis beneath a carious lesion, tertiary dentin,
• smear layer,
• and intratubular deposition of fibrinogen also reduce dentin permeability .
• Host defense molecules, such as antibodies and components of the complement system, may also be present in the dentinal
As long as the pulp is vital, dentinal exposure does not represent a significant route of pulpal infection, except when dentin thickness is considerably reduced or when the dentin permeability is significantly Increased Most of the bacteria in the carious process are non motile; they invade dentin by repeated cell division, which pushes cells into tubules. Bacterial cells may also be forced into tubules by hydrostatic pressures developed on dentin during mastication.
Bacteria inside tubules under a deep carious lesion can reach the pulp even before frank pulpal exposure. As mentioned, it has been assumed that the pulp will not be infected if it is still vital. The few bacteria that reach the pulp may not
be significant, because the vital pulp can eliminate such a transient infection and rapidly clear or remove bacterial products.
On the other hand, if the vitality of the pulp is compromised and the defense mechanisms are impaired, even a small amount of bacteria may initiate infection.
Direct exposure of the dental pulp to the oral cavity is the most obvious route of endodontic infection. Caries is the most common cause of pulp exposure, but bacteria may also reach the pulp via direct pulp exposure as a result of iatrogenic restorative procedures or trauma
to pathologic changes in these tissues It has been claimed that microorganisms can reach the pulp by anachoresis . Theoretically, microorganisms can be transported in the blood or lymph to an area of tissue damage, where they leave the vessel, enter the damaged tissue, and establish an infection
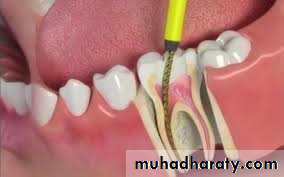
Microbial penetration in the canal treatment schedule can occur :
during treatment,between appointments,
or even after root canal obturation.The main causes of microbial introduction into the canal during treatment include:
• remnants of dental biofilm,• or caries on the tooth crown;
• leaking rubber dam;
• contamination of endodontic instruments (e.g., after touching with the fingers);
• and contamination of irrigant solutions or other solutions of intracanal use (e.g., saline solution, distilled water, citric acid).
Microorganisms can also enter the root canal system between appointments by:
leakage through the temporary restorative materialand or breakdown, fracture,
or loss of the temporary restoration
fracture of the tooth structure
and in teeth left open for drainage.Microorganisms can penetrate the root canal system even after completion of the root canal obturation by:
leakage through the temporary or permanent restorative material;
breakdown, fracture, or loss of the temporary/permanent restoration;fracture of the tooth structure;
recurrent decay contaminating the root canal obturation;or delay in the placement of permanent restorations
TYPES OF ENDODONTIC INFECTIONS
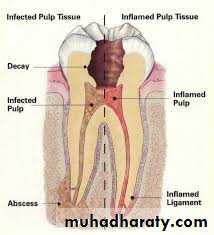
Endodontic infections can be classified according to the anatomic location as intraradicular or extraradicular infection.Intraradicular infection is caused by microorganisms colonizing the root canal system and can be subdivided into three categories according to the time microorganisms entered the root canal system: primary infection, caused by microorganisms
that initially invade and colonize the necrotic pulp tissue (primary or initial or “virgin” infection);
secondary infection, caused by microorganisms not present in the primary infection but introduced in the root canal at some time after professional intervention (i.e., secondary to intervention);
and persistent infection, caused by microorganisms that were members of a primary or secondary infection and in some way resisted intracanal antimicrobial procedures and were able to endure periods of nutrient deprivation in treated canals
Endodontic infection
Intraradicular infection
extraradicular infection
primary infection
secondary infection
persistant infection
Endodontic infections develop in a previously sterile place that does not contain a normal microbiota. Any species found has the potential to be an endodontic pathogen or at least play
a role in the ecology of the endodontic microbial community.
The oral cavity harbors one of the highest accumulations of microorganisms in the body .There are an estimated 10 billion bacterial cells in the oral cavity More than 1000 bacterial species/phylotypes have been found in the human oral cavity
PRIMARY INTRARADICULAR INFECTIONMicrobial Composition and Diversity
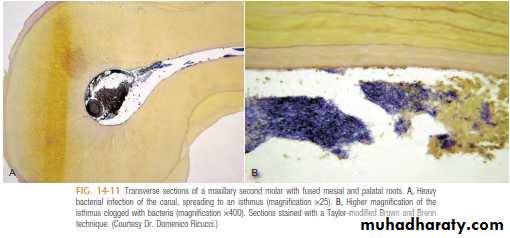
Primary infections are characterized by a mixed (multispecies) community conspicuously dominated by anaerobic bacteria. The number of bacterial cells may vary from 10³ to 10⁸ per root canal with a mean of 10 to 20 species/phylotypes per infected canalThe size of apical periodontitis lesion has been shown to be proportional to the number of bacterial species and cells in
the root canal the number of taxa per canal (is a group of one or more populations of an organism) was clearly in direct proportion to the lesion size: small lesions ( < 5 mm) harbored about 12 taxa, lesions from 5 to less than 10 mm harbored 16 taxa, and lesions over 10 mm harbored about 20 species. Some canals associated with large lesions may harbor even more than 40 taxa
The root canal flora is dominated by anaerobic bacteria , of which a restricted group is present in infected root canals.
Gram-positive organisms (75%) with most predominant being streptococci (28%), staphylococci (15%), corynebacteria (10–25%), yeasts (12%), and others.
Gram-negative bacteria (24%) include spirochetes (9–12%), Neisseriae (4%), Bacteroides (7%), fusobacteria (3%), pseudomonas (2%), coliform bacteria (1%), and others.
Researchers have confirmed that Tannerella forsythia is a common member of microbiota associated with endodontic infections including abscesses.
Fusobacterium nucleatum has also been identified as a commonly encountered gram-negative
organism with five subspecies, namely fusiforme , nucleatum , polymorphum , vincentii , and animalis .
About 40% to 66% of the endodontic microbiota in primary infections is composed of species still uncultivated ḷ ḷ ḷ
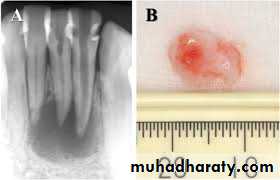
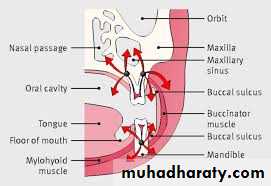
Symptomatic apical periodontitis and acute apical abscesses
Symptomatic apical periodontitis and acute apical abscesses are typical examples of endodontic infections causing severe symptoms. In these cases, the infection is located in the canal, but it has also reached the periradicular tissues and, in abscessed cases, can spread to other anatomic spaces The microbiota involved in endodontic abscesses is mixed and dominated by anaerobic bacteria.Direct comparisons using molecular technology reveal an average of 12 to 18 taxa per abscess case, compared with 7 to 12 taxa present in root canals of teeth with asymptomatic lesions
Whereas microbial causation of apical periodontitis is well established, there is no strong evidence disclosing
specific involvement of a single species with any particular signor symptom of apical periodontitis.
Some gram-negative anaerobic bacteria have been suggested to be involved with symptomatic lesions but the same species may also be present in some what similar frequencies in asymptomatic cases
so factors other than the mere presence of a given putative pathogenic species may play a role in the etiology of symptomatic endodontic infections. These factors include :
• differences in virulence ability among strains of the same species,
• bacterial interactions resulting in additive or synergistic effects among species in mixed infections,
• number of bacterial cells (infectious load),
• environmental cues regulating expression of virulence factors,
• host resistance;
• And concomitant herpesvirus infection.
• Association of some or all of these factors (instead of an isolated event) is likely to determine the occurrence and intensity of symptoms
Microbial Ecology and the Root Canal Ecosystem
The necrotic root canal might be considered a fertile environment for bacterial growth.• A root canal with necrotic pulp provides a space for bacterial colonization and affords bacteria a moist, warm, nutritious,and anaerobic environment
• protected from the host defenses because of lack of active blood circulation in the necrotic pulp tissue.
• Also, the root canal walls are nonshedding surfaces conducive to persistent colonization and formation of complex communities
The major ecologic factors that determine the composition of the root canal microbiota include oxygen tension, type and amount of available nutrients, and bacterial interactions
The root canal infection is a dynamic process, and different bacterial species apparently dominate at different stages
In the initial phases of the pulpal infectious process, facultative bacteria predominate After a few days or weeks, oxygen is depleted within the root canal as a result of pulp necrosis and consumption by facultative bacteria. Further oxygen supply is interrupted with loss of blood circulation in the necrotic pulp. An anaerobic milieu develops and is highly conducive to the survival and growth of obligate anaerobic bacteria With the passage of time, anaerobic conditions become even more pronounced, particularly in the apical third of the root canal; as a consequence, anaerobes will dominate the microbiota.
The main sources of nutrients for bacteria colonizing
the root canal system include:(1) the necrotic pulp tissue,
(2) proteins and glycoproteins from tissue fluids and exudate
that seep into the root canal system via apical and lateral
foramina,
(3) components of saliva that may coronally pene-
trate into the root canal,
(4) products of the metabolism of other bacteria.
Because the largest amount of nutrients is
available in the main canal, the most voluminous part of theroot canal system, most of the infecting microbiota (particu-
larly fastidious anaerobic species) is expected to be located
in this region
Bacterial species that can best utilize and compete for nutrients in the root canal system will succeed in
colonization
Even though the necrotic pulp tissue can be regarded
as a finite source of nutrients to bacteria (given the smallvolume of tissue that is progressively degraded), induction of
periradicular inflammation guarantees a sustainable source
of nutrients, particularly in the form of proteins and glyco-
proteins present in the exudate that seep into the canal
At this stage of the infectious process, bacteria that have a proteolytic
capacity or establish a cooperative interaction with those thatcan utilize this substrate in the metabolism, start to dominate.
Therefore, as the infectious process reaches the stage of
induction of periradicular inflammation, proteins become the
principal nutrient source, particularly in the apical part of
the canal, favoring the establishment of anaerobic species
that utilize peptides or amino acids in their metabolism
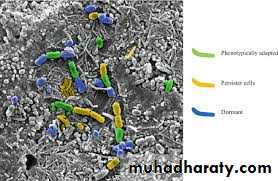
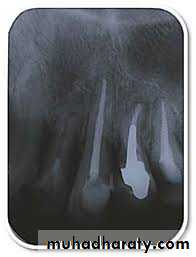
PERSISTENT/SECONDARY ENDODONTIC INFECTIONS
persistent intraradicular infections are caused by microorganisms that resisted intracanal antimicrobial procedures and survived in the treated canal.Involved microorganisms are remnants of a primary or secondary infection. The latter, in turn, is caused by microorganisms
that at some time entered the root canal system secondary to clinical intervention .The moment can be during treatment,
between appointments, or even after root canal filling. In any circumstance, if penetrating microorganisms manage to adapt
themselves to the new environment, surviving and flourishing, a secondary infection is established. Species involved can be
oral microorganisms or not, depending on the source of secondary infection
Bacteria at the Root Obturation Stage
Bacteria persisting in the root canal after chemomechanical procedures or intracanal medication will not always maintainan infectious process. This statement is supported by evidence that some apical periodontitis lesions healed even after bacteria were isolated from the canal at the obturation stage. There are some possible explanations :
♦ Residual bacteria may die after obturation because of toxic effects of the filling material or sealer, access denied to
nutrients, or disruption of bacterial ecology.
♦ Residual bacteria may be present in quantities and virulence subcritical to sustaining periradicular inflammation.
♦ Residual bacteria remain in locations where access to periradicular tissues is denied
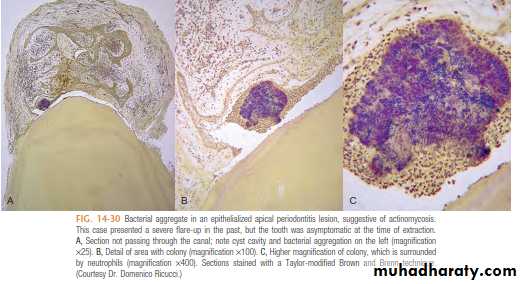
EXTRARADICULAR INFECTIONSExtraradicular infection in turn is characterized by microbial invasion of the inflamed periradicular tissues and is a sequel to the intraradicular infection. Extraradicular infections can be dependent on or independent of the intraradicular infection
In most situations, apical periodontitis inflammatory lesions succeed in preventing microorganisms from invading the periradicular tissues
Nevertheless, in some specific circumstances, microorganisms can overcome this defense barrier and establish an extraradicular infection. The most common form of extraradicular infection is the acute apical abscess, characterized by purulent inflammation in the periradicular tissues in response to a massive egress of virulent bacteria from the root canal
There are, however, other forms of extraradicular infection either by adherence to the apical
external root surface in the form of extraradicular biofilm structures or by formation of cohesive actinomycotic colonies within the body of the inflammatory lesion
Microbes seeking to establish in the root canal must leave the nutritionally rich and diverse environment of the oral cavity, breach enamel, invade dentine, overwhelm the immune response of the pulp and settle in the remaining necrotic tissue within the root canal.
During that time they have to compete in a limited space with other microbes for the available nutrition. It is no accident that microbes berth in a particular environment there are ecological advantages for them to establish and flourish if conditions are favorable. Through genetic exchange and mutation, microbes have developed specialized systems that facilitate their ability to find, compete and survive in these very specific environments
Life is not easy for an endodontic pathogen
THANK YOU
UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYTHE END
2020-2021Hope to you life without apical pathosis