بسم الله الرحمن الرحيم
السلام عليكم ورحمة الله وبركاتهIN THE NAME OF GOD THE MOST MERCIFULL
3/2/2021Tumors of the lungs &bronchial tree
Dr Majeed Mohan AlhamamiObjectives
To know theepidemiology ,
etiology,
pathogenesis ,
clinical presentation,
investigation ,
diagnosis ,
treatment ,
complication ,
prognosis
TUMOURS OF THE BRONCHUS AND LUNG
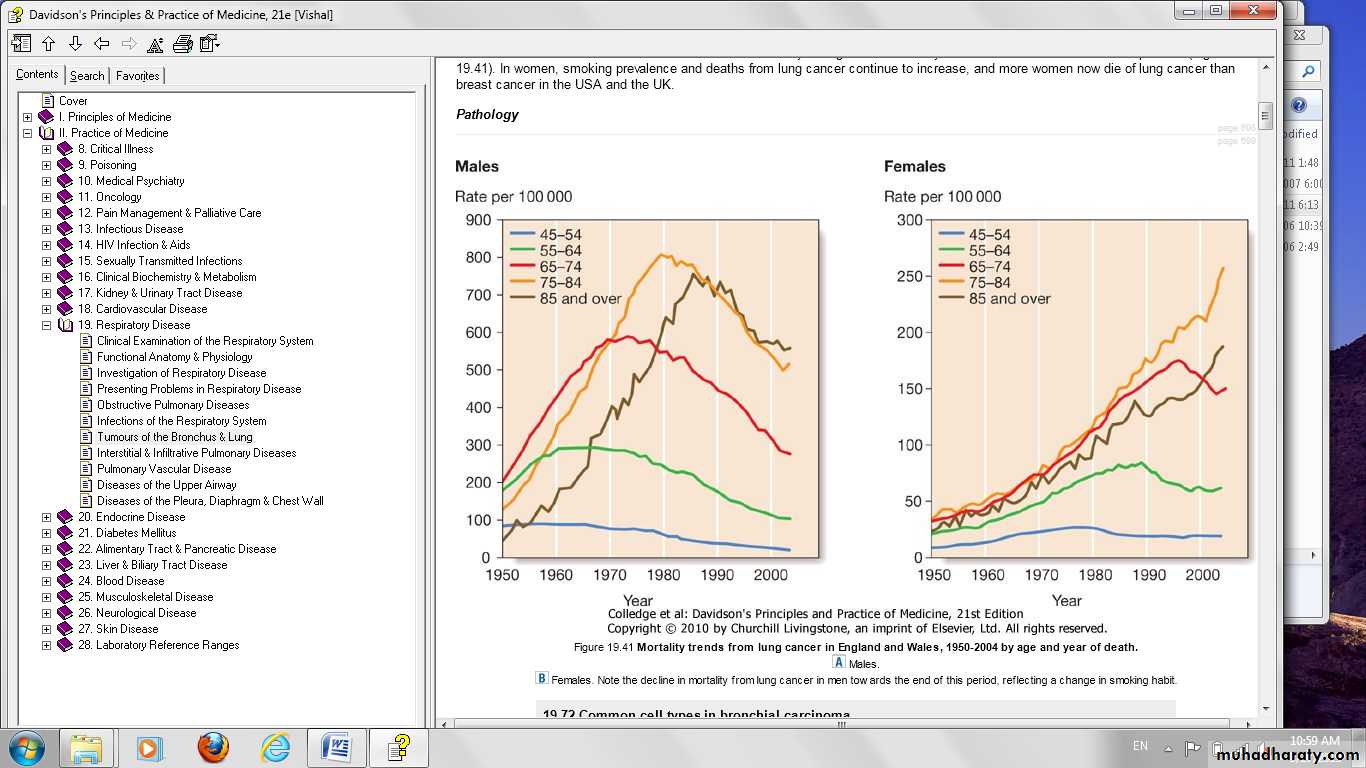
1.8 million new cases worldwide each year
Most common cancer in men
Rates rising in women:
More than 50% of cases have metastatic disease at diagnosis
Lung cancer kills more than 120,000 Americans each year .
Accounts for 18% of all cancer deaths
Primary tumours of the lung
AetiologyCigarette smoking
Exposure to radon
industrial materials (e.g. asbestos, silica, beryllium, cadmium and chromium)
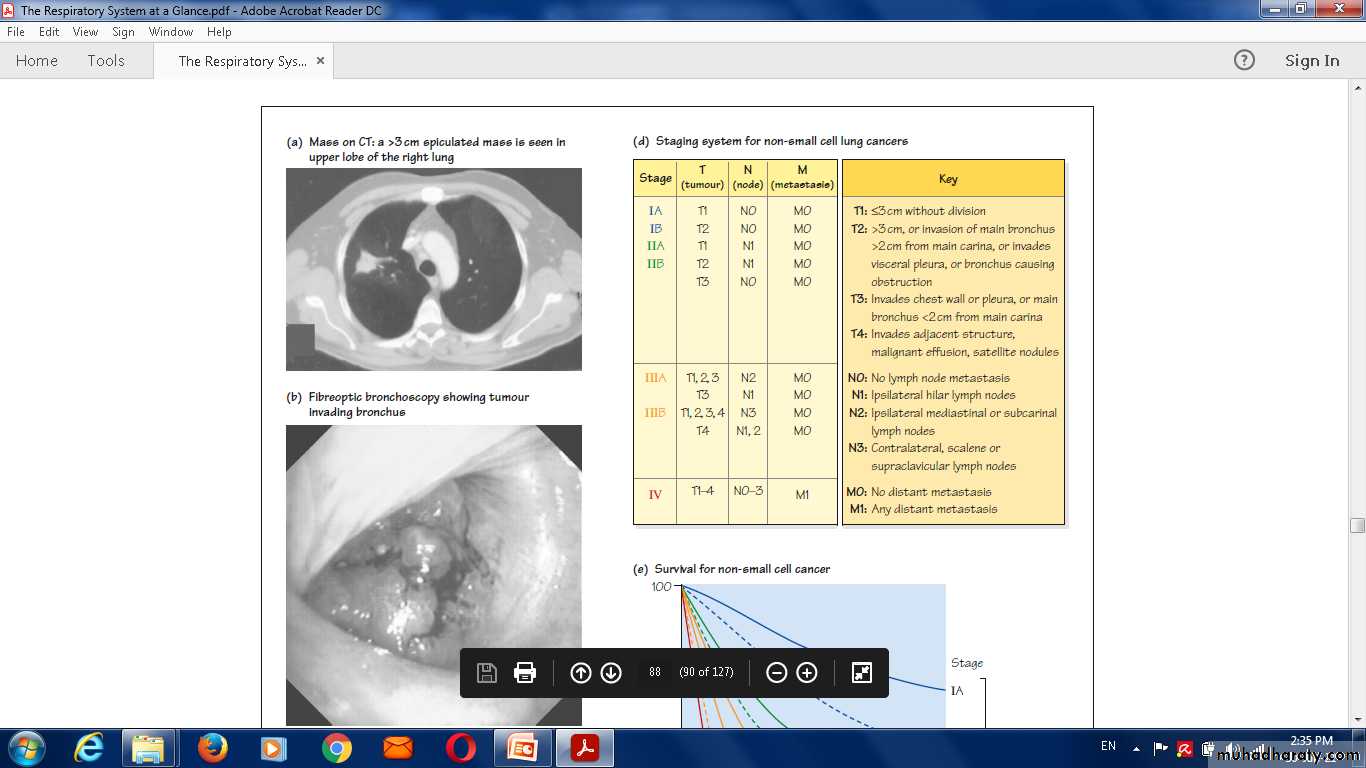
Common cell types in lung cancer updated 2017
Cell type %Adenocarcinoma 35–40
Squamous 25–30
Small-cell 15
Large-cell 10–15
Bronchial carcinoma
The incidence of bronchial carcinoma increased
Bronchial carcinomas arise from the bronchial epithelium or mucous glands.
symptoms arise early, when the tumour occurs in a large bronchus(central)delayed diagnosis tumors originating in a peripheral bronchus.(peripheral)
central necrosis and cavitation, and may resemble a lung abscess on X-ray.(Squamous cell carcinoma)
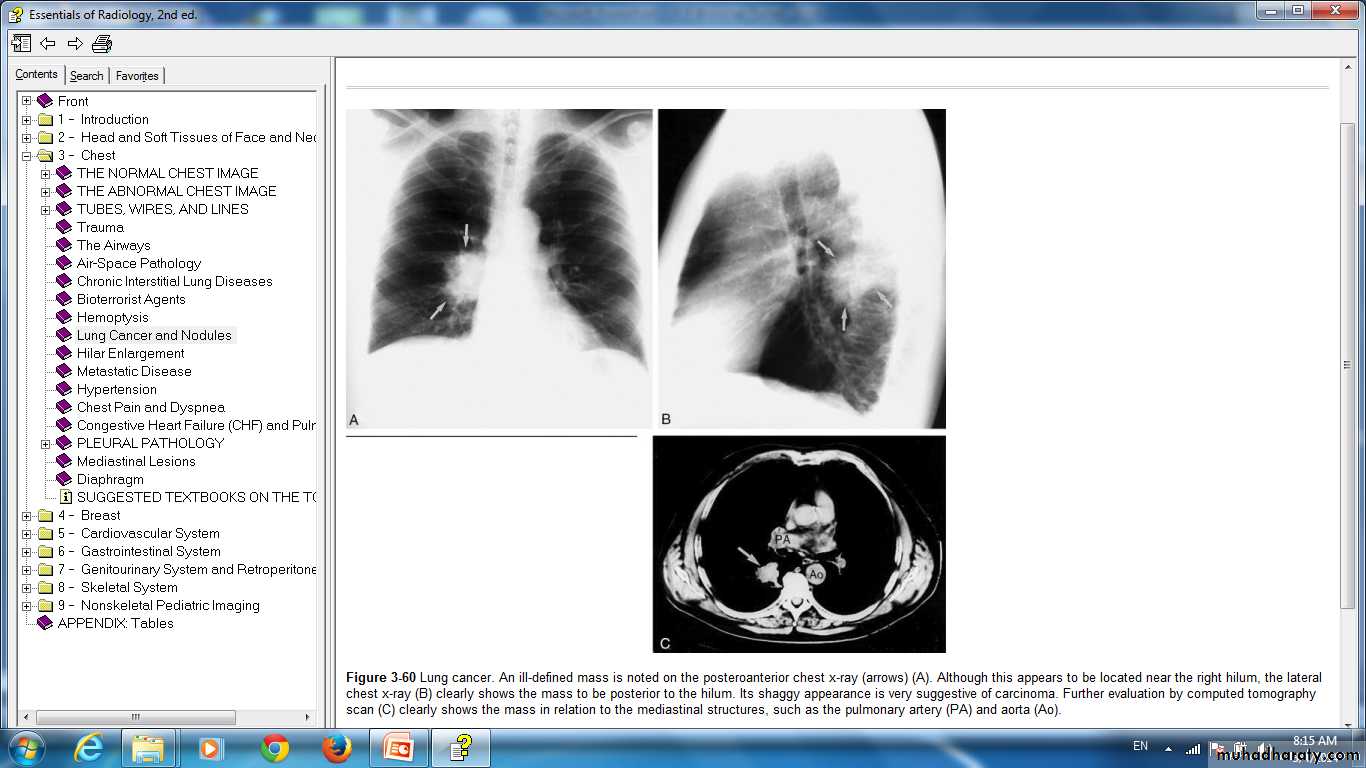
Lung cancer. An ill-defined mass is noted on the posteroanterior chest x-ray (arrows) (A). Although this appears to be located near the right hilum, the lateral chest x-ray (B) clearly shows the mass to be posterior to the hilum. Its shaggy appearance is very suggestive of carcinoma. Further evaluation by computed tomography scan (C) clearly shows the mass in relation to the mediastinal structures, such as the pulmonary artery (PA) and aorta (Ao).
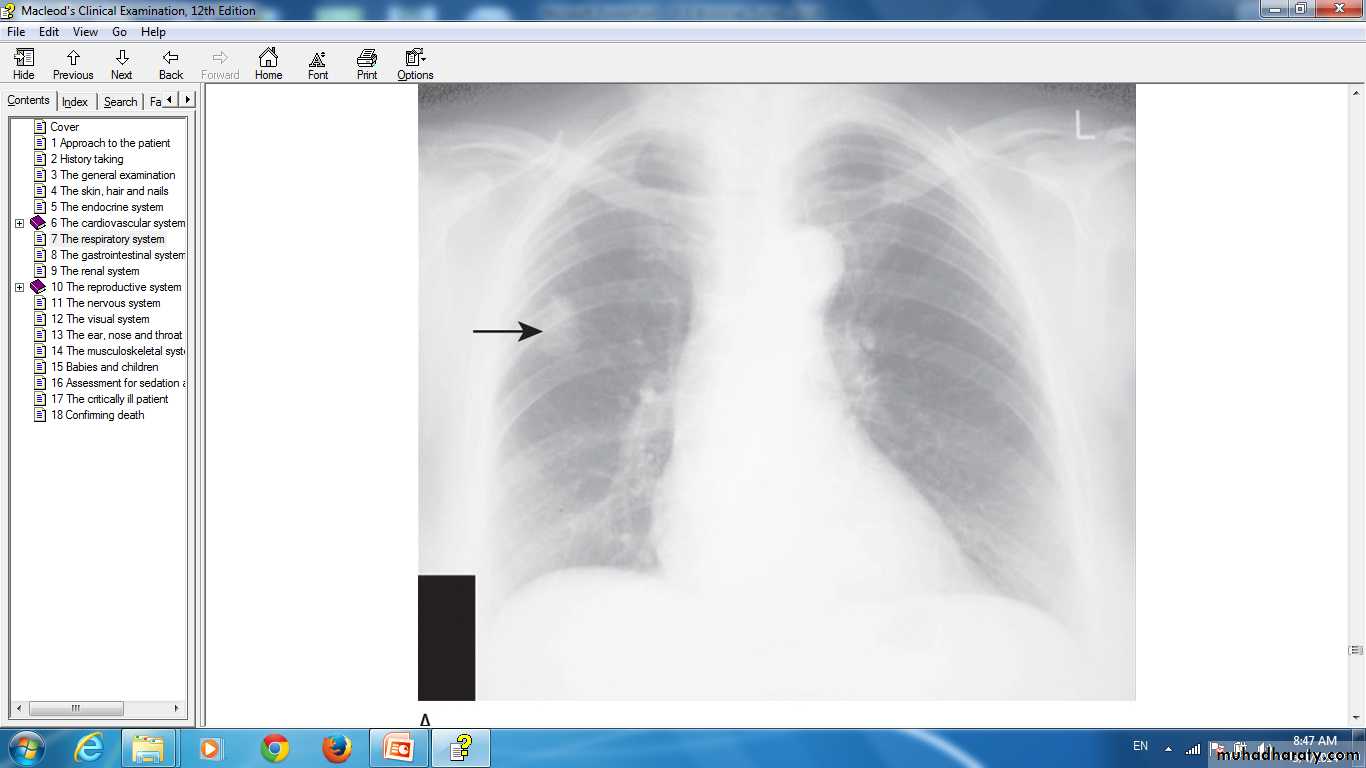
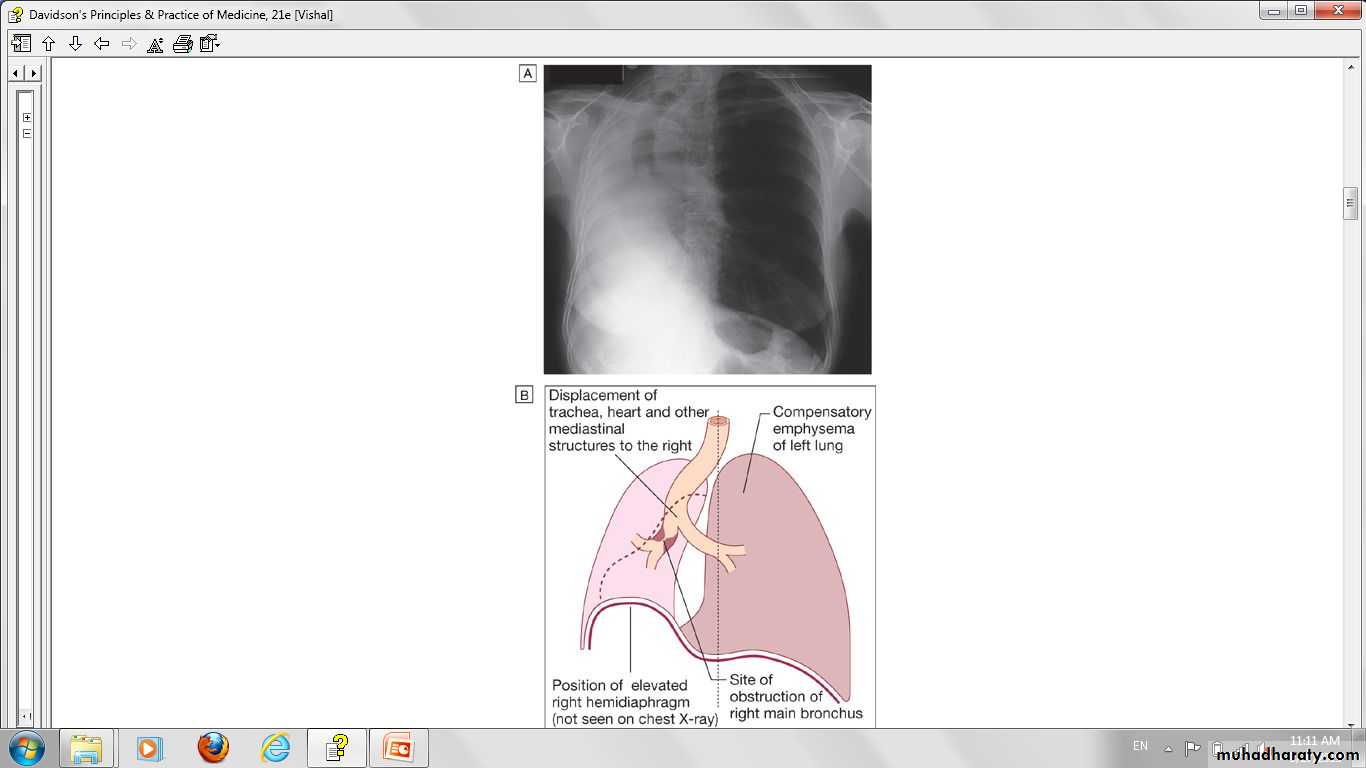
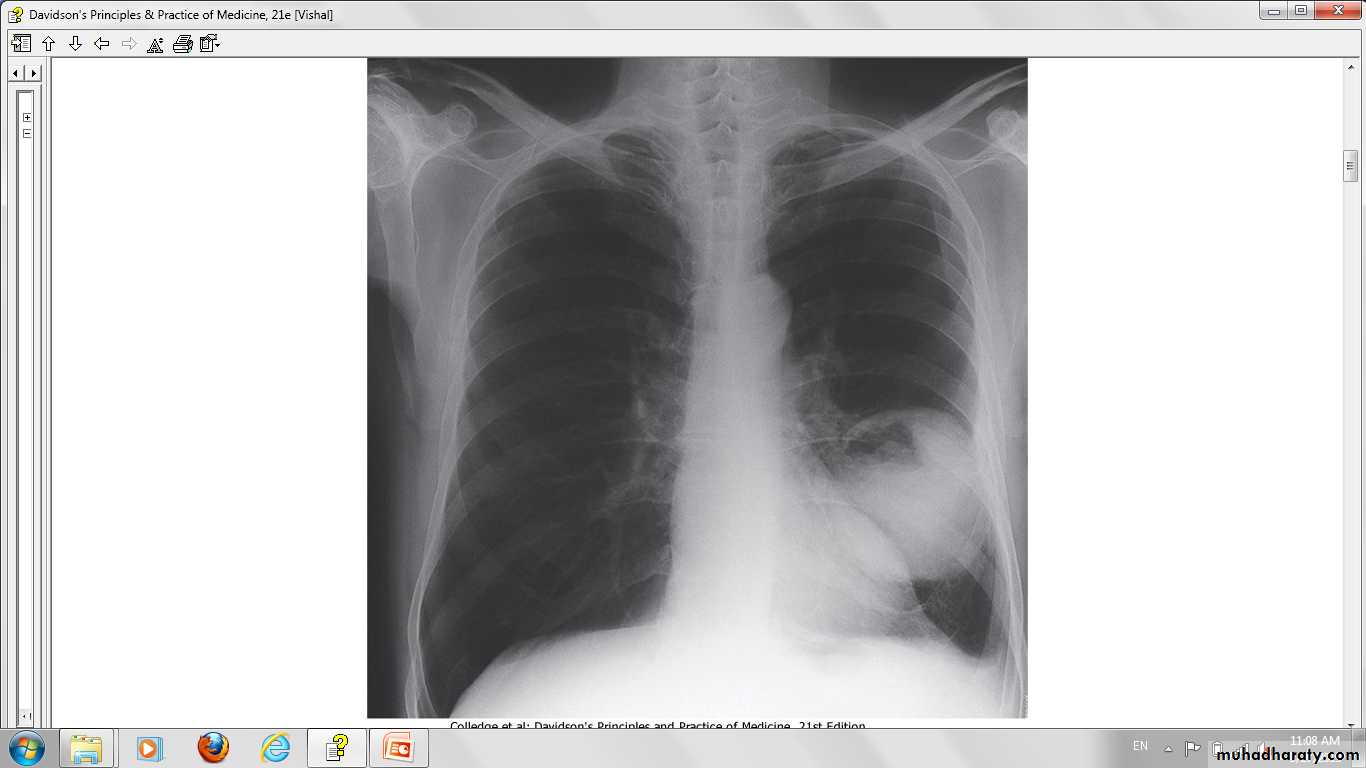
Lung cancer in right lung Chest X-ray.
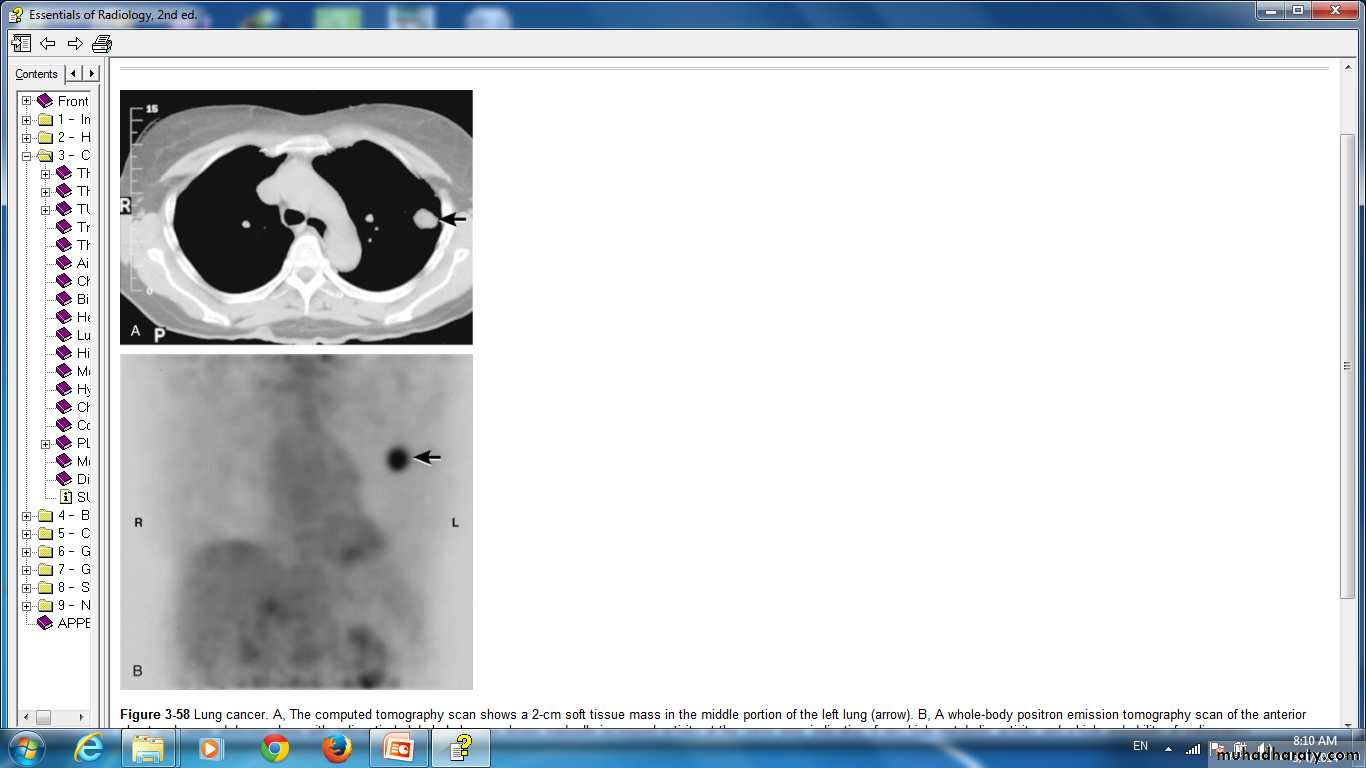
Lung cancer. A, The computed tomography scan shows a 2-cm soft tissue mass in the middle portion of the left lung (arrow). B, A whole-body positron emission tomography scan of the anterior chest and upper abdomen done with radioactively labeled glucose shows markedly increased activity at the same area, indicative of very high metabolic activity and a high probability of malignancy.
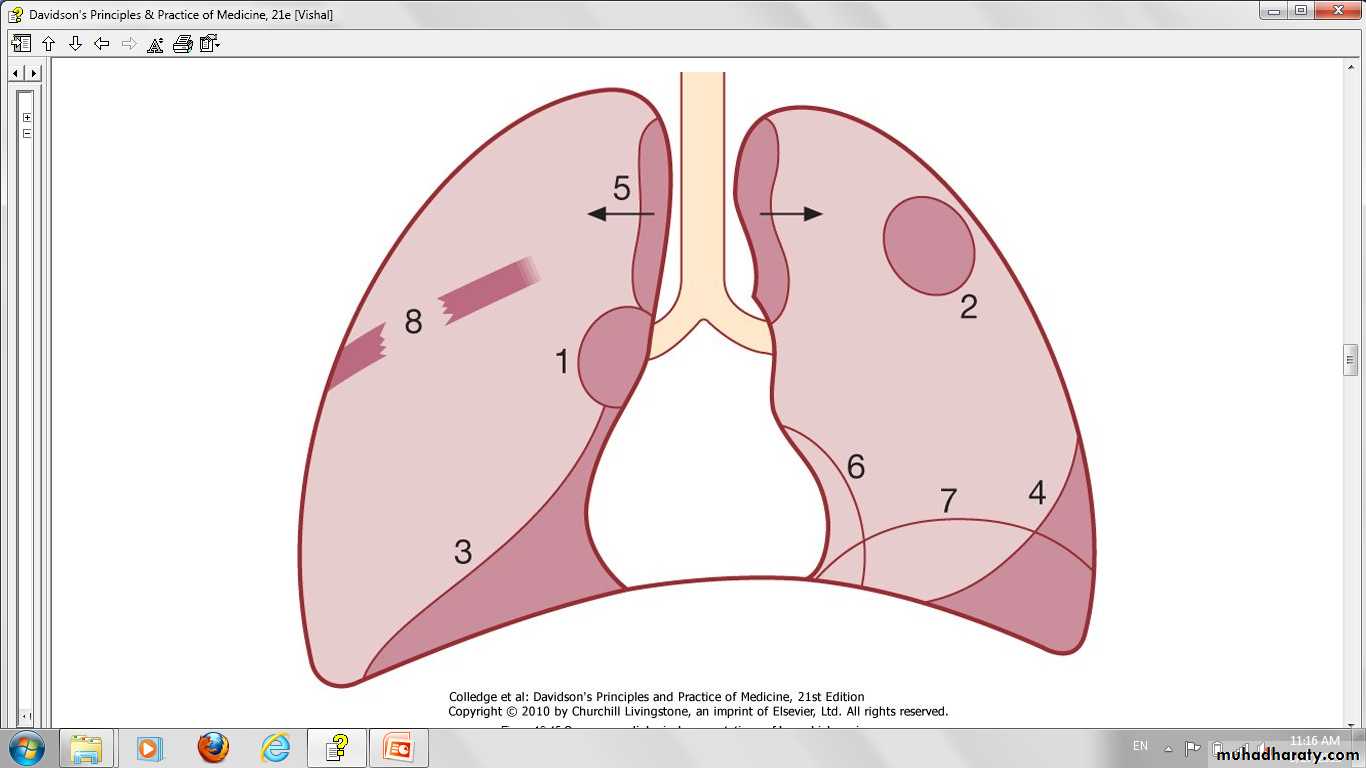
Bronchial carcinoma may involve
1-Direct invasionthe pleura
the chest wall,
invading the intercostal nerves
the brachial plexus and causing pain.
Lymphatic spread
mediastinalsupraclavicular lymph nodes.
Blood-borne metastases
Liver.Bone.
Brain.
Adrenals.
Skin.
Even a small primary tumour may cause widespread metastatic deposits and this is a particular characteristic of small-cell lung cancers
Symptom
CoughChest pain
Cough and pain
Coughing blood
Malaise
Weight lossShortness of breath
Hoarseness
Distant spread
No symptoms
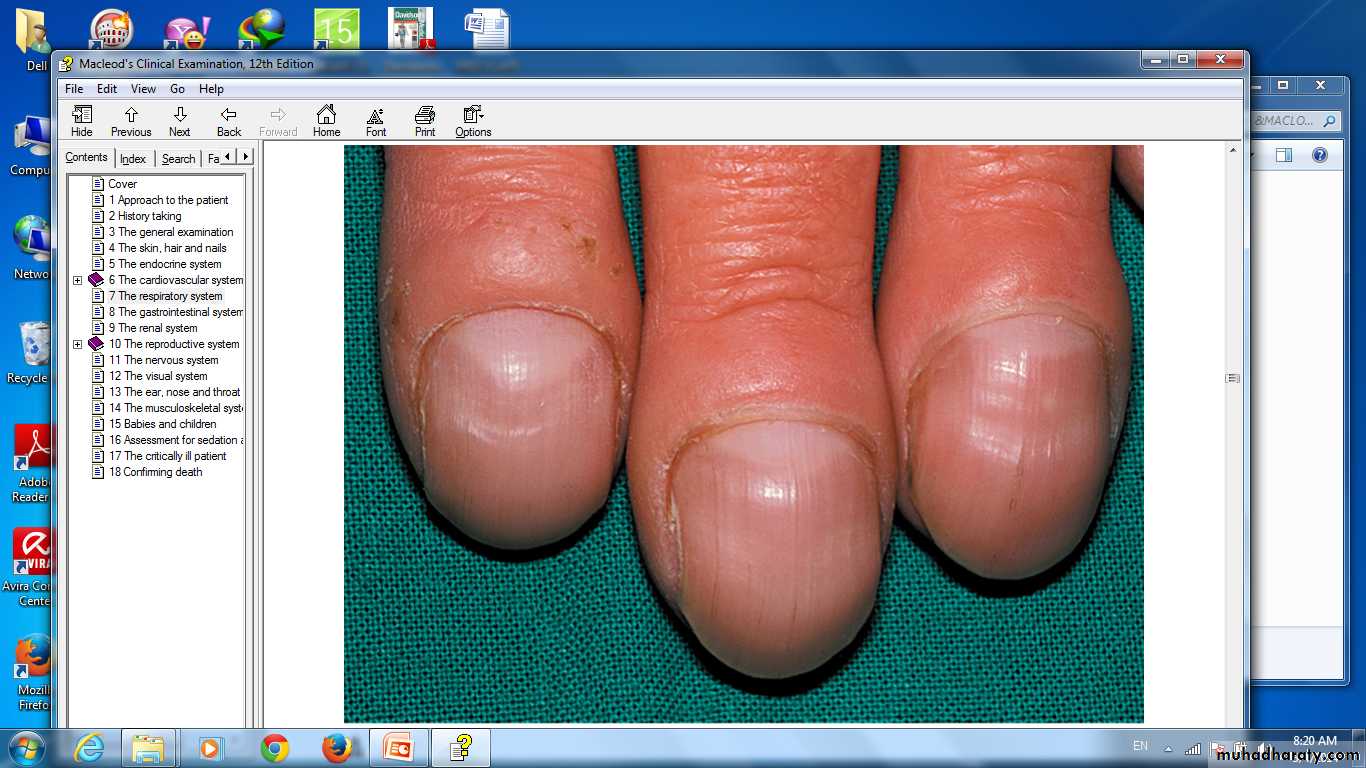
Tobacco 'tar'-stained fingers
clubb
X-ray of the lower legs in hypertrophic pulmonary osteoarthropathy. Arrows show periosteal reaction
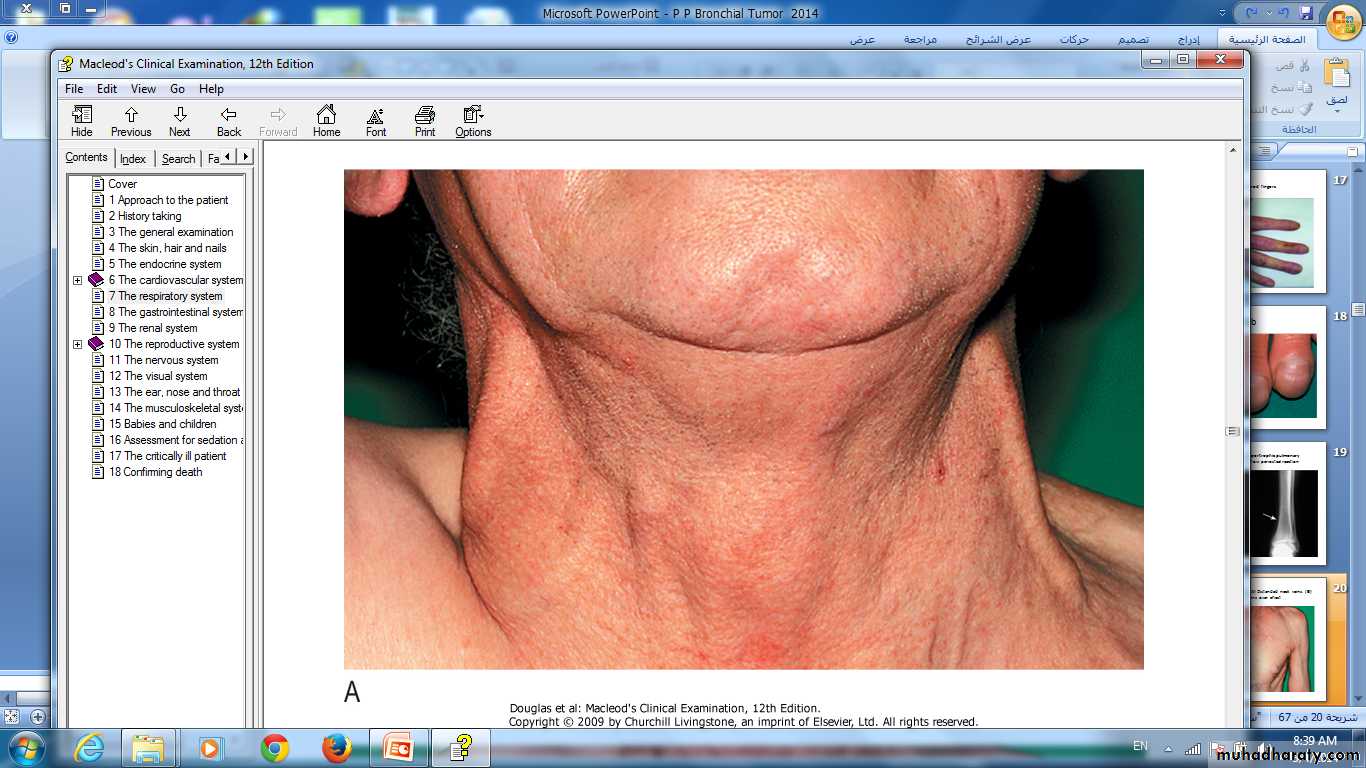
Superior vena caval obstruction Distended neck veins.
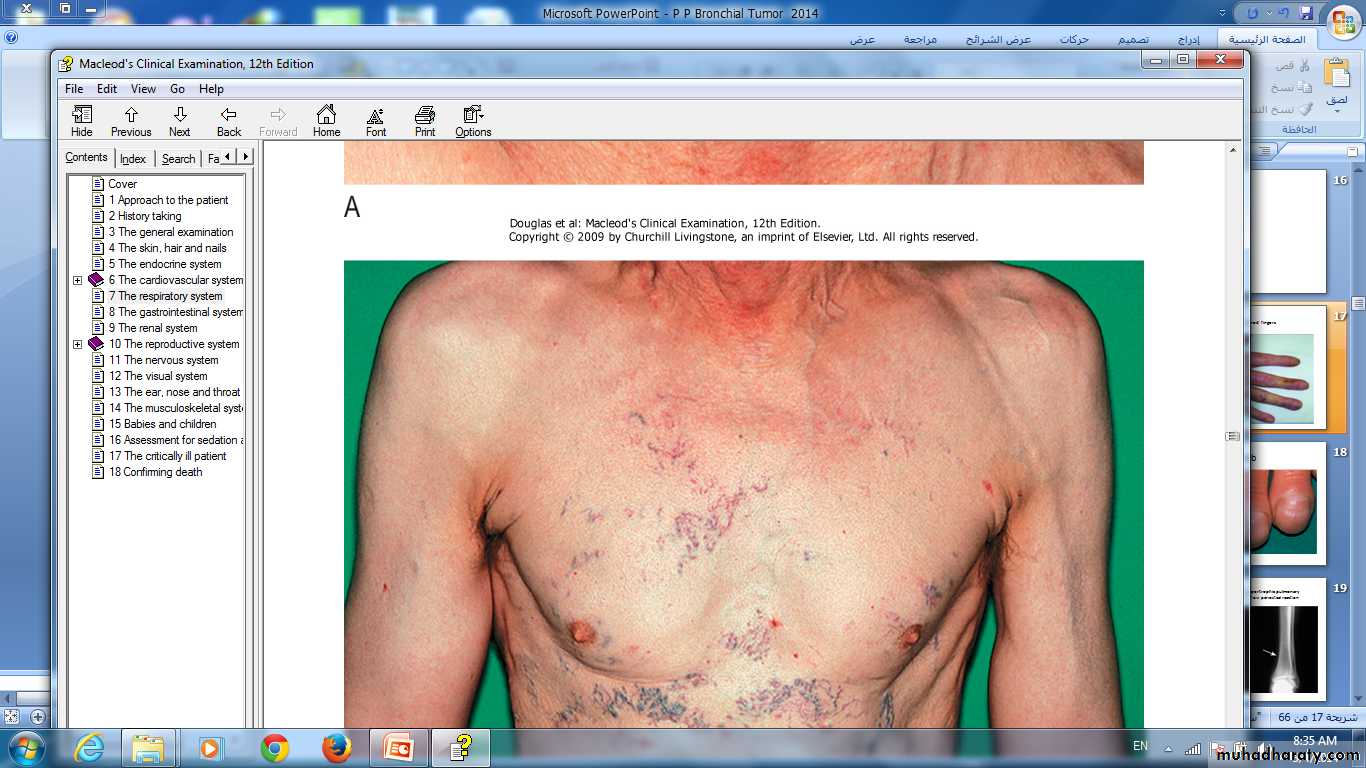
Superior vena caval obstruction. Dilated superficial veins over chest
local
Cough.Haemoptysis.
Breathlessness .
Bronchial obstruction.
collapse of a lobe or lung .
cause pneumonia or lung abscess.
Recurnt Pneumonia at the same site.
Stridor (a harsh inspiratory noise) .
a large pleural effusion
compressing a phrenic nerve causing diaphragmatic paralysis.
Pain and nerve entrapment.
Pleural pain.pain in the distribution of a thoracic dermatome.
Horner's syndrome .(1)
Pancoast's syndrome (2).
_______________________________________________
(1)ipsilateral partial ptosis, enophthalmos, miosis and hypohidrosis of the face.(2)pain in the shoulder and inner aspect of the arm, sometimes with small muscle wasting in the hand
Mediastinal spread.
Dysphagia If the oesophagus is involved.Invasion of the pericardium, lead to arrhythmia or pericardial effusion .
Superior vena cava obstruction.
left recurrent laryngeal nerve --- causes vocal cord paralysis, voice alteration and a 'bovine' cough (lacking the normal explosive character).
Supraclavicular lymph nodes -----enlarged.
Metastatic spread.
Brainfocal neurological defects,
epileptic seizures,
personality change,
Liver : jaundice,
Bone : bone pain
Skin :skin nodules.
Lassitude, anorexia and weight loss.
Digital clubbing.
Non-metastatic extrapulmonary manifestations of bronchial carcinoma
Endocrine
Inappropriate antidiuretic hormone secretion causing hyponatraemia
Ectopic adrenocorticotrophic hormone secretion
Hypercalcaemia due to secretion of parathyroid hormone-related peptides
Carcinoid syndrome
Gynaecomastia
Neurological
Polyneuropathy
Myelopathy
Cerebellar degeneration
Myasthenia (Lambert-Eaton syndrome,)
Digital clubbing
Hypertrophic pulmonary osteoarthropathyNephrotic syndrome
Polymyositis and dermatomyositis
Eosinophilia
Investigations
confirm the diagnosis .establish the histological cell type.
define the extent of the disease.
Imaging
plain X-raysSpiral CT
Lung cancer in right lung Chest X-ray.
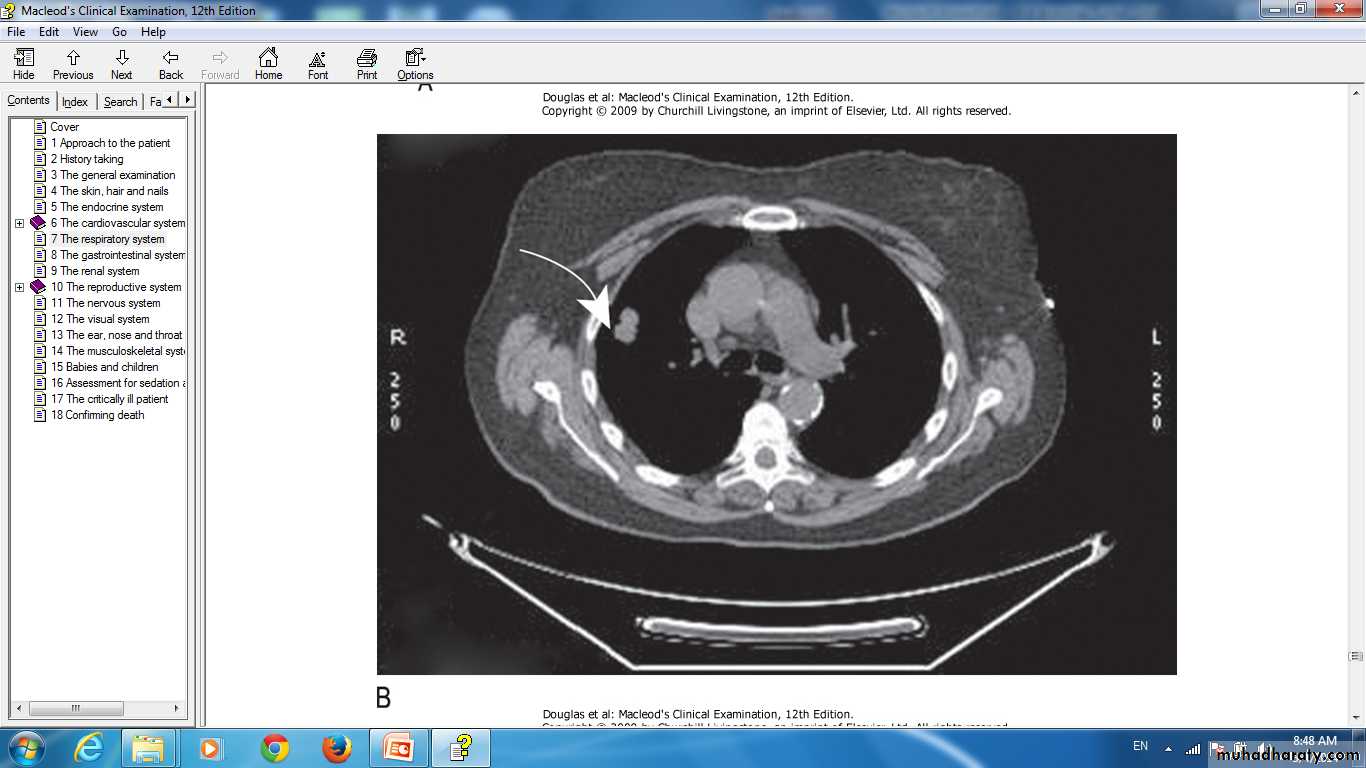
Lung cancer in right lung CT scan of thorax.
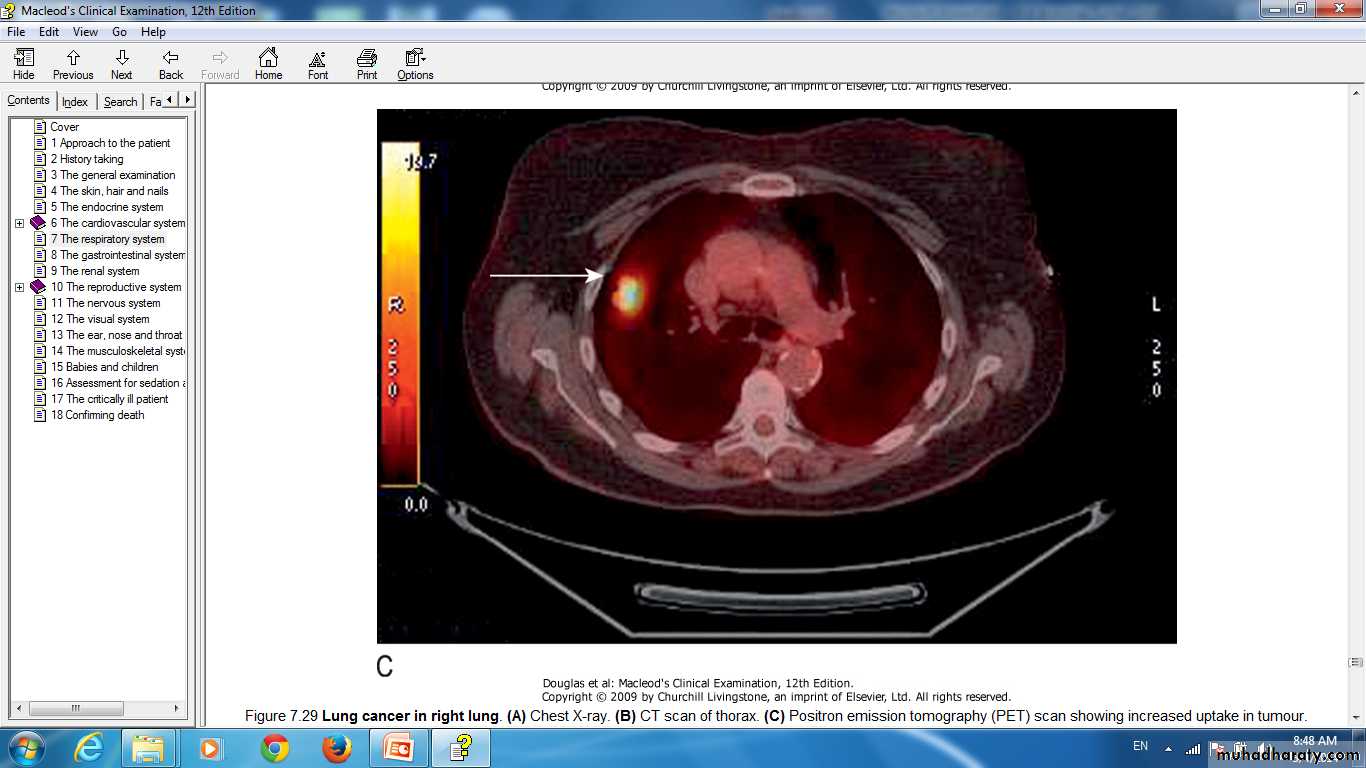
Lung cancer in right lung Positron emission tomography (PET) scan showing increased uptake in tumour
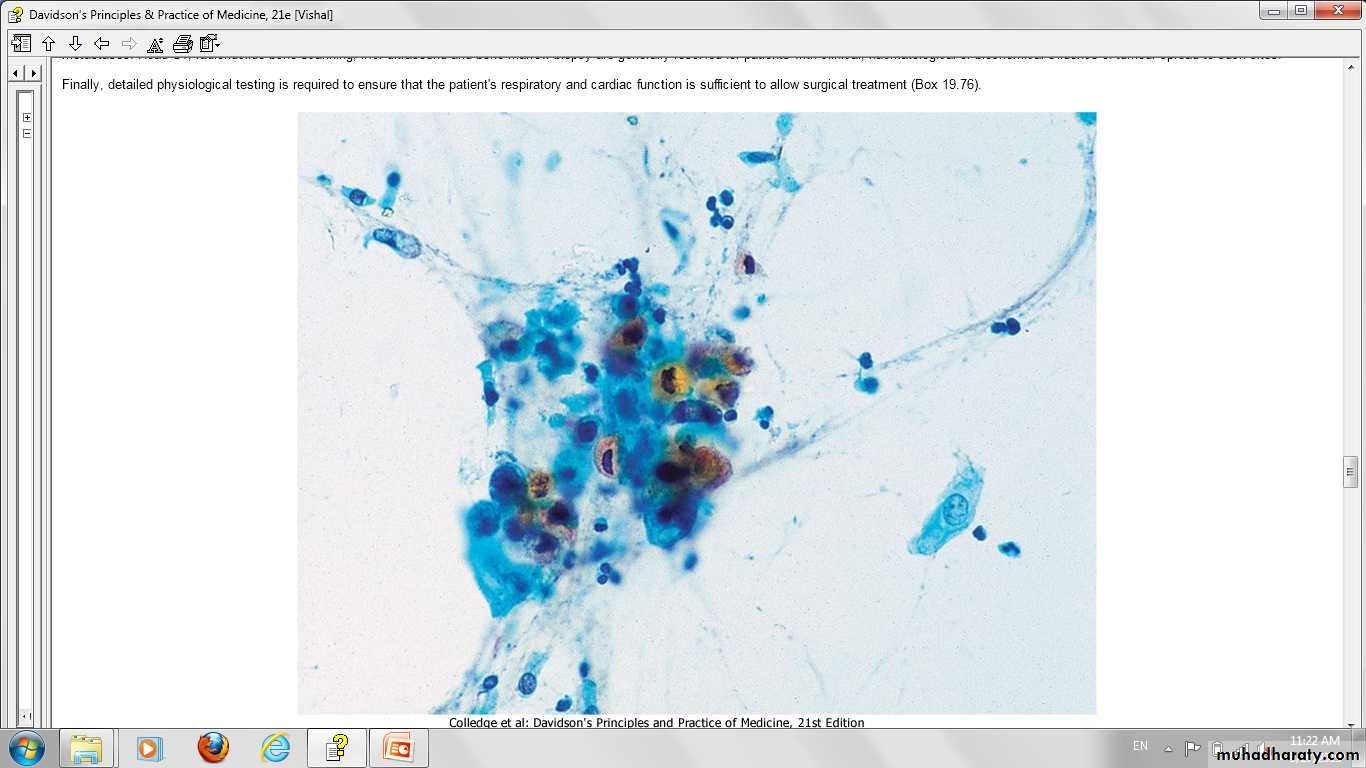
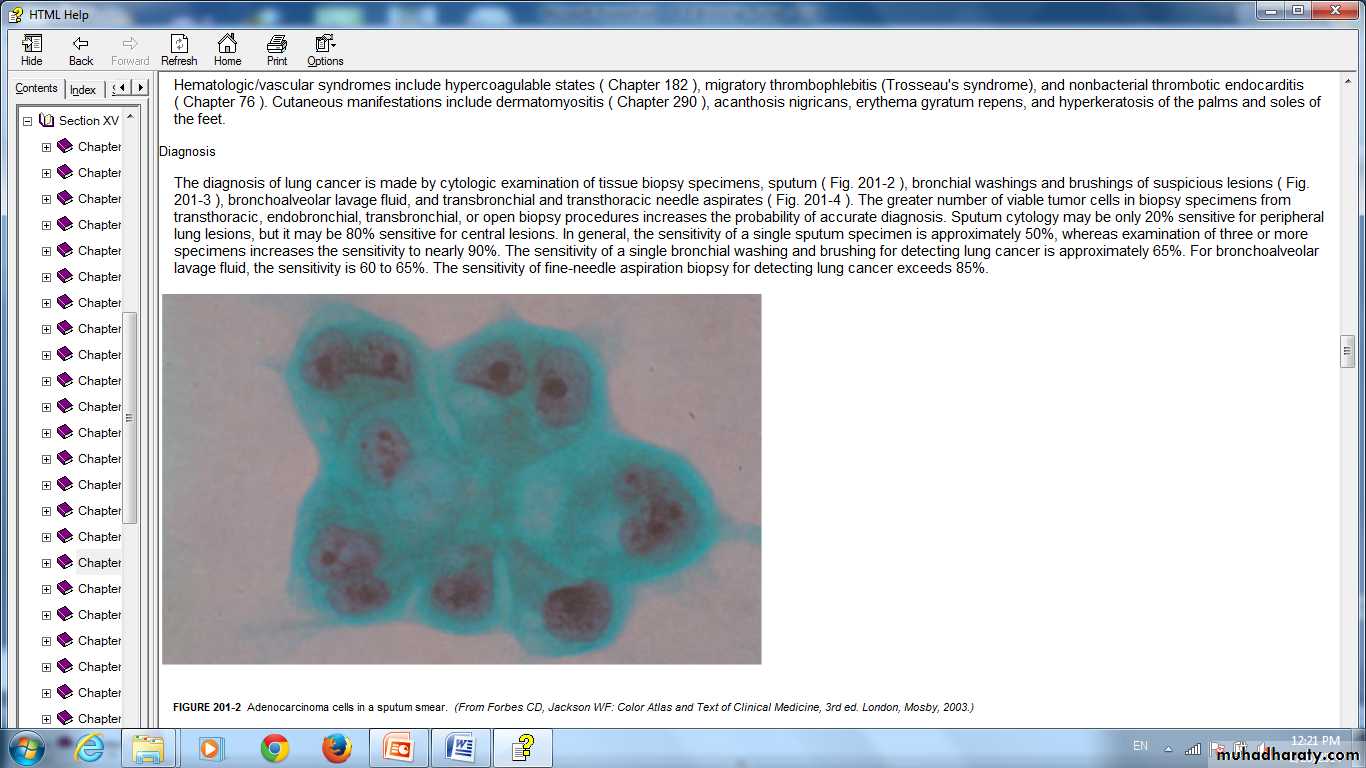
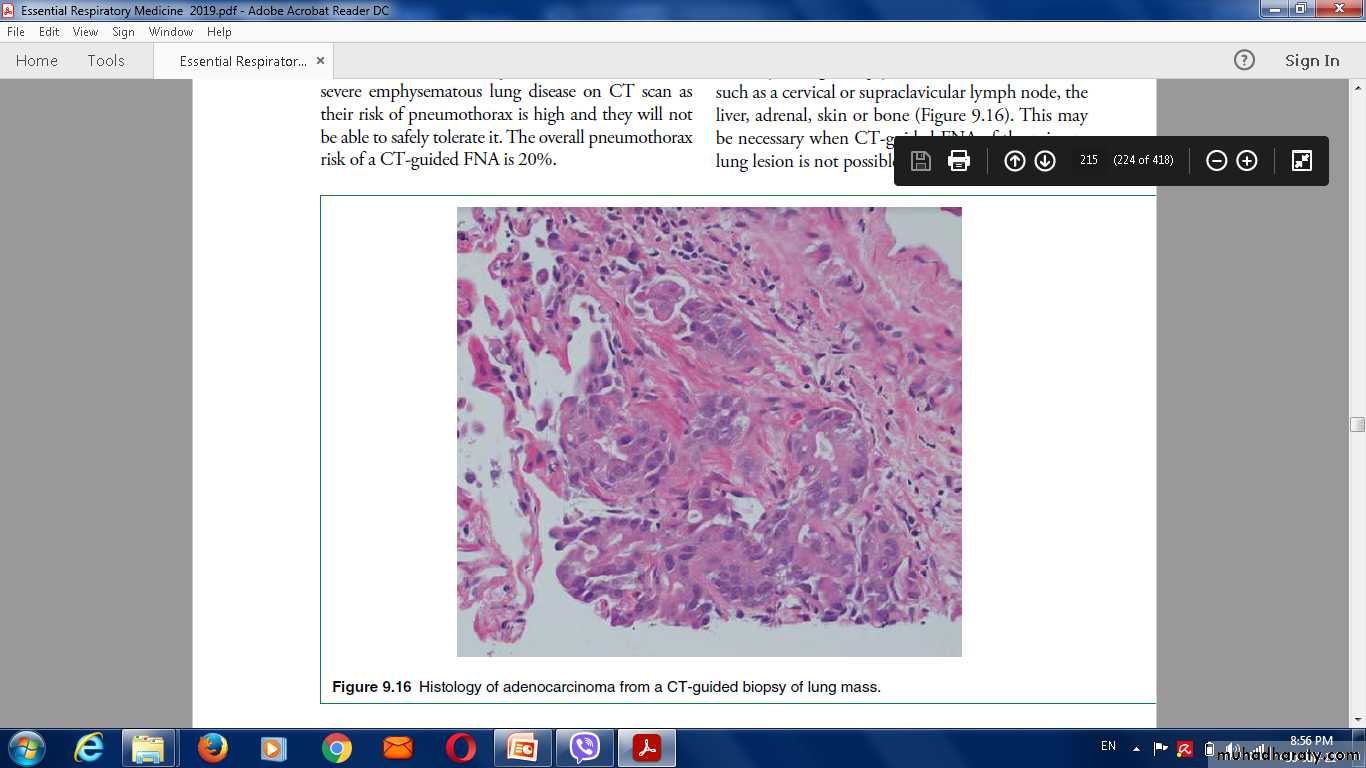
Histological characterisation
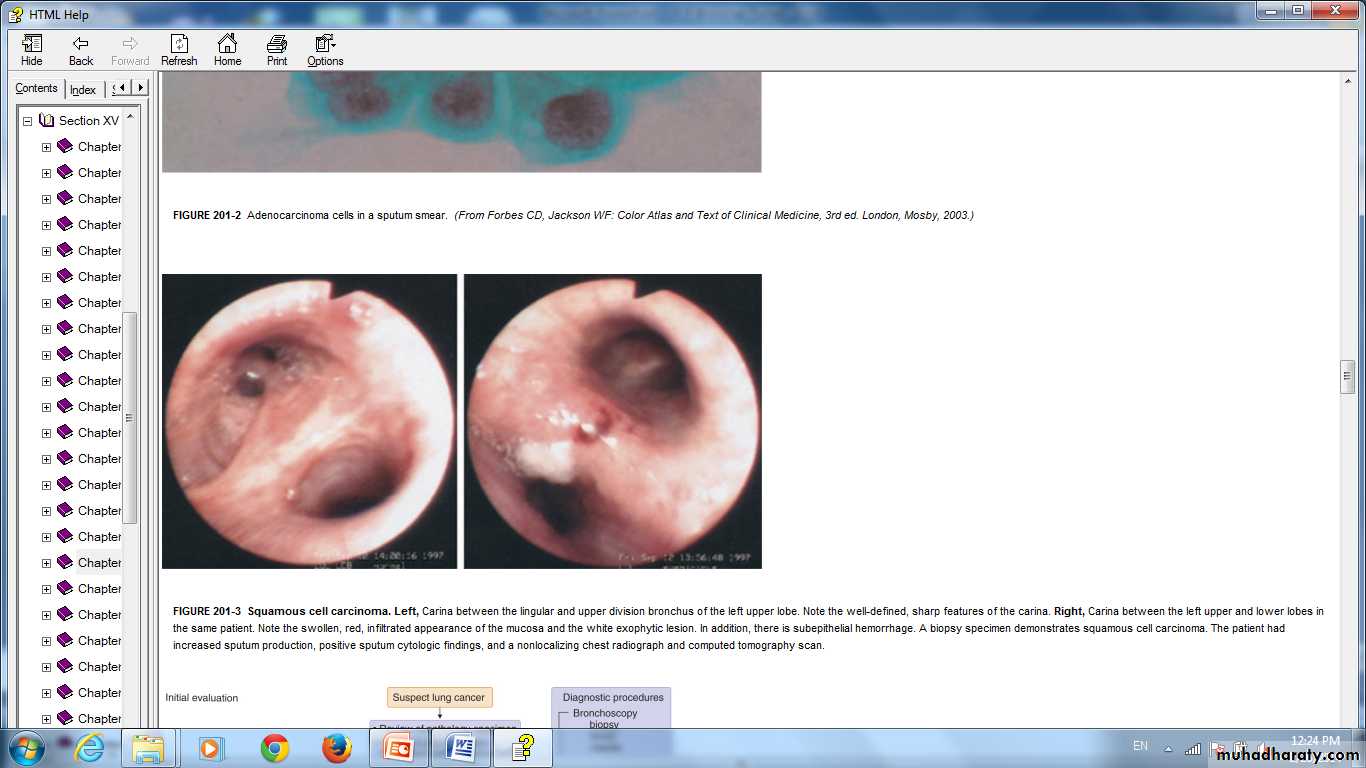
flexible bronchoscope.'blind' bronchoscopic washings and brushings
percutaneous needle biopsy under CT or ultrasound guidance .
Squamous cell carcinoma.
Adenocarcinoma cells in a sputum smear
Three sputum samples should be obtained for cytology
pleural effusions, pleural aspiration and biopsythoracoscopy.
needle aspiration or biopsy of affected
lymph nodes,
skin lesions,
liver
bone marrow.
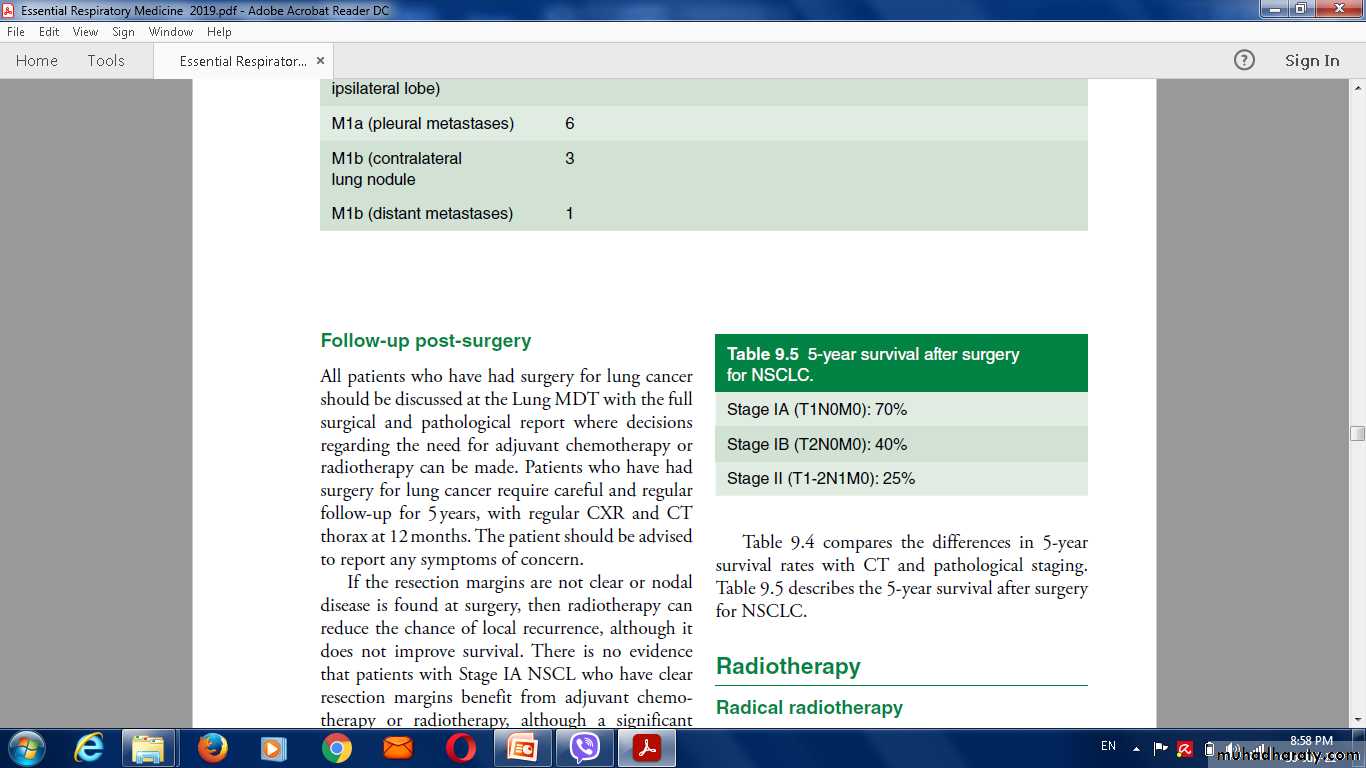
Management
Surgical resection carries the best hope of long-term survival.some patients treated with
radiotherapy
Chemotherapy.
over 75% of cases,NO treatment curative treatment .
Radiotherapy, chemotherapy, can relieve distressing symptoms.
Contraindications to surgical resection in bronchial carcinoma (important)
• Distant metastasis .
• Invasion of central mediastinal structures including heart, great vessels, trachea and oesophagus .• Malignant pleural effusion .
• Contralateral mediastinal nodes .
• FEV1 < 0.8 L .
• Severe or unstable cardiac or other medical condition
Laser therapy and stenting
major airway obstructionGeneral aspects of management .
The management in specialist centres by multidisciplinary teams including
oncologists,
thoracic surgeons,
respiratory physicians
specialist nurses;
Treatment include:
effective communication.pain relief .
attention to diet .
depression and anxiety, need specific therapy.
drain the pleural cavity.
pleurodesis with a sclerosing agent.
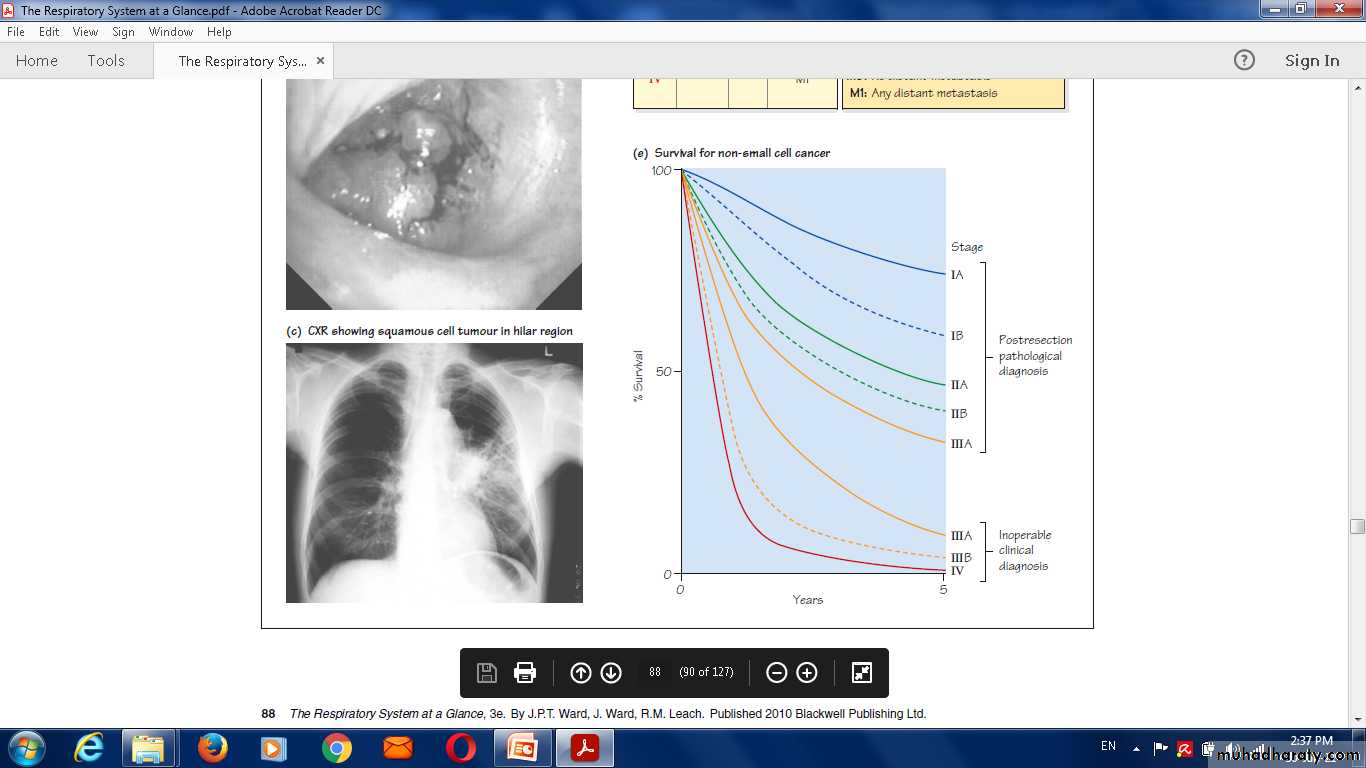
Prognosis
Very poor .
70% of patients dying within a year .Only 6-8% of patients surviving 5 years after diagnosis.
The best prognosis is with well-differentiated squamous cell tumours .
Secondary tumours of the lung
Blood-borne metastaticfrom many primary tumours :
breast,
kidney,
uterus,
ovary,
Testes
thyroid.
Diagnosis
No symptomsBreathlessness .
haemoptysis.
radiological examination
Multiple bilateral cannon balls.
lobar collapse
Lymphangitic spread of carcinoma in the lung
Lymphatic infiltration may develop in patients with carcinoma of the
breast,stomach,
bowel,
pancreas
bronchus.
This grave condition causes severe and rapidly progressive breathlessness associated with marked hypoxaemia.
The chest X-ray
shows diffuse pulmonary shadowing radiating from the hilar regions, with septal lines.CT scans characteristic.
Palliative treatment of breathlessness with opiates may help.
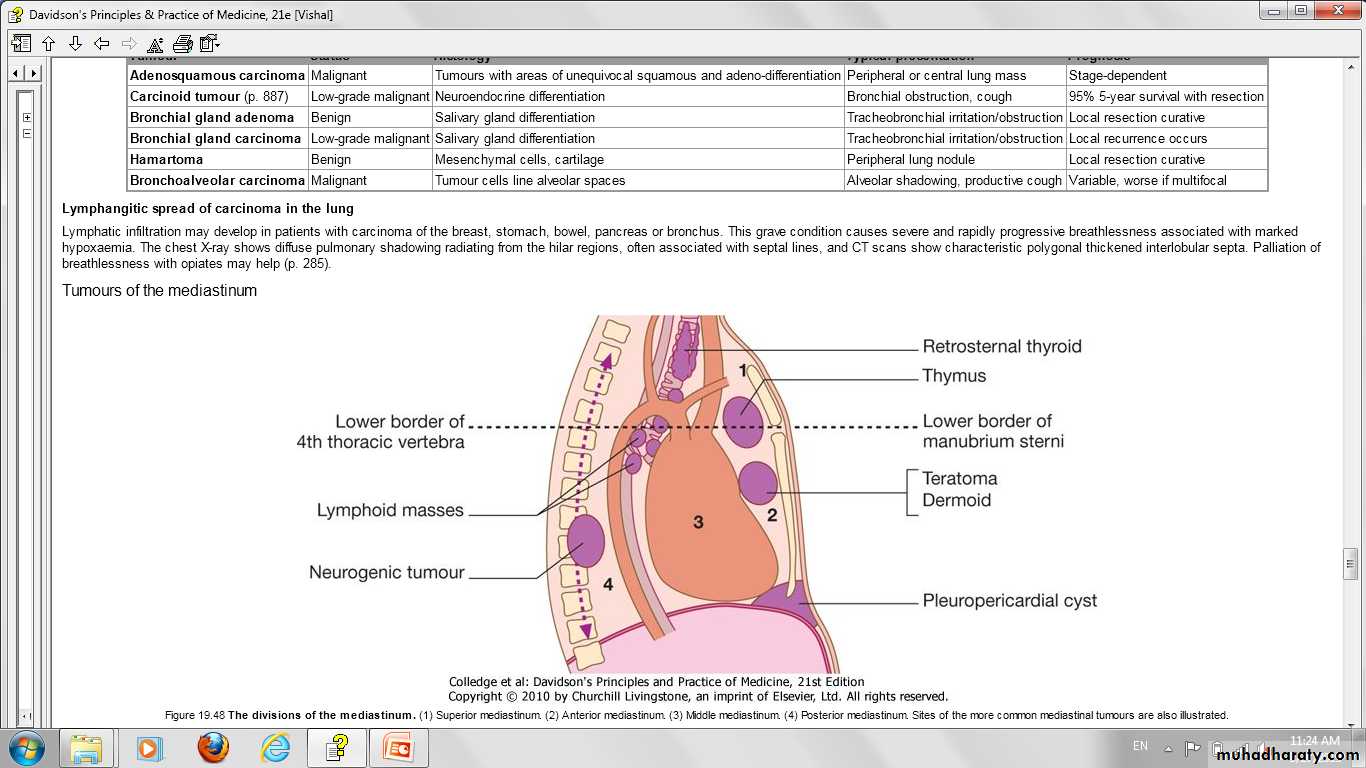
Tumours of the mediastinumpresent radiologically as a mediastinal mass .
Benign tumours and cysts
symptoms by compressing
the trachea
the superior vena cava.
rupture into a bronchus.
Malignant mediastinal tumours
InvasionCompress surrounding structures.
The most common cause is mediastinal lymph node
metastases from bronchogenic carcinoma
lymphomas,
leukaemia,
malignant thymic tumours
germ-cell tumours
Aortic and innominate aneurysms have destructive features resembling those of malignant mediastinal
Causes of a mediastinal mass
Superior mediastinum
Retrosternal goitre
Persistent left superior vena cava
Prominent left subclavian artery
Thymic tumour
Dermoid cystLymphoma
Aortic aneurysm
Anterior mediastinum
Retrosternal goitreDermoid cyst
Thymic tumour
Lymphoma
Aortic aneurysm
Germ cell tumour
Pericardial cystHiatus hernia through the diaphragmatic foramen of Morgagni
Posterior mediastinum
Neurogenic tumour
Paravertebral abscess
Oesophageal lesion
Aortic aneurysm
Foregut duplicationMiddle mediastinum
Bronchial carcinomaLymphoma
Sarcoidosis
Bronchogenic cyst
Hiatus hernia
Radiological examination
CT (or MRI) is the investigation of choice for mediastinal tumours .Large mass (intrathoracic goitre-arrows) extending from right upper mediastinum.
Endoscopic investigationBronchoscopy.
Surgical exploration
Mediastinoscopy to visualise and biopsy masses.Management
Benign mediastinal tumours should be removed surgicallyneural tumours, have the potential to undergo malignant transformation.