بسم الله الرحمن الرحيم
IN THE NAME OF ALLAH THE MOST MERCIFULL.
7/2/2021
Pulmonary vascular disease
1- Pulmonary hypertension.2-Pulmonary venous thromboembolism.
3-Pulmonary vasculitis.
Pulmonary hypertension
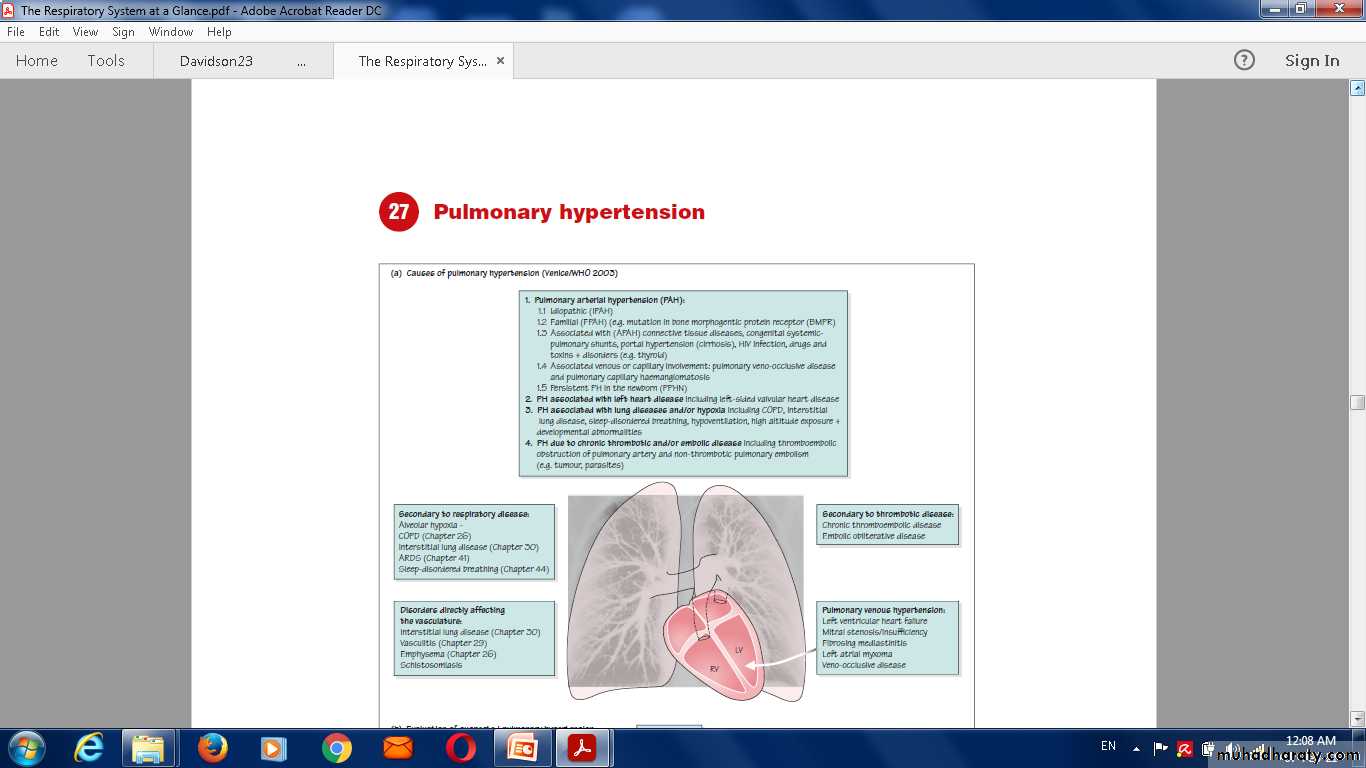
Objectives:Causes of pulmonary hypertension
1-Pulmonary vascular disordersAcute pulmonary thromboembolism (rarely tumour emboli)
Primary pulmonary hypertension
2-Diseases of the lung and parenchyma
COPD
3-Musculoskeletal disorders (causing chronic underventilation)
Kyphoscoliosis
4-Disturbance of respiratory control
Obstructive sleep apnoea5-Cardiac disorders
Mitral stenosis
Left ventricular failure
6-Miscellaneous
Appetite-suppressant drugs.
Primary pulmonary hypertension (PPH)
Present spontaneously with no apparent underlying disease
occur in association with other disease processes.
Primary pulmonary hypertension
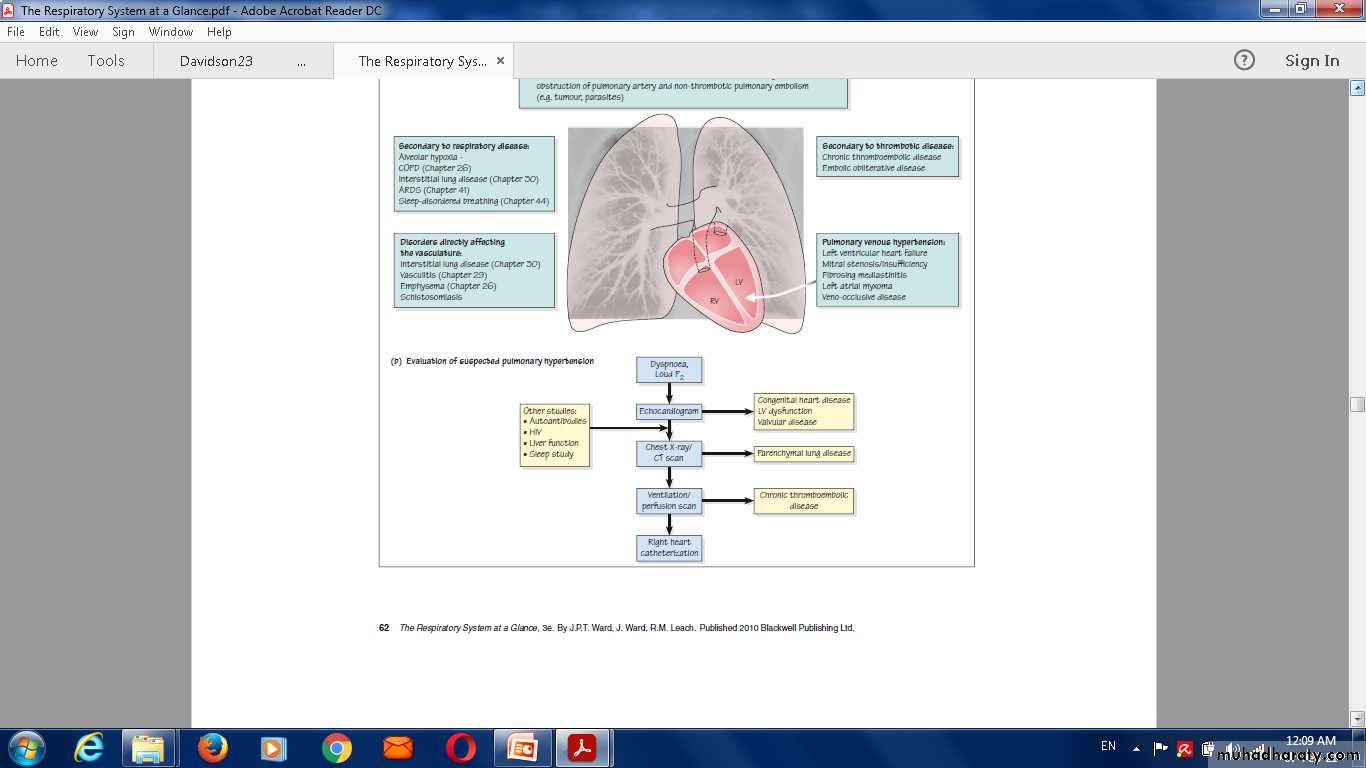
Clinical presentationClinical signs of pulmonary hypertension
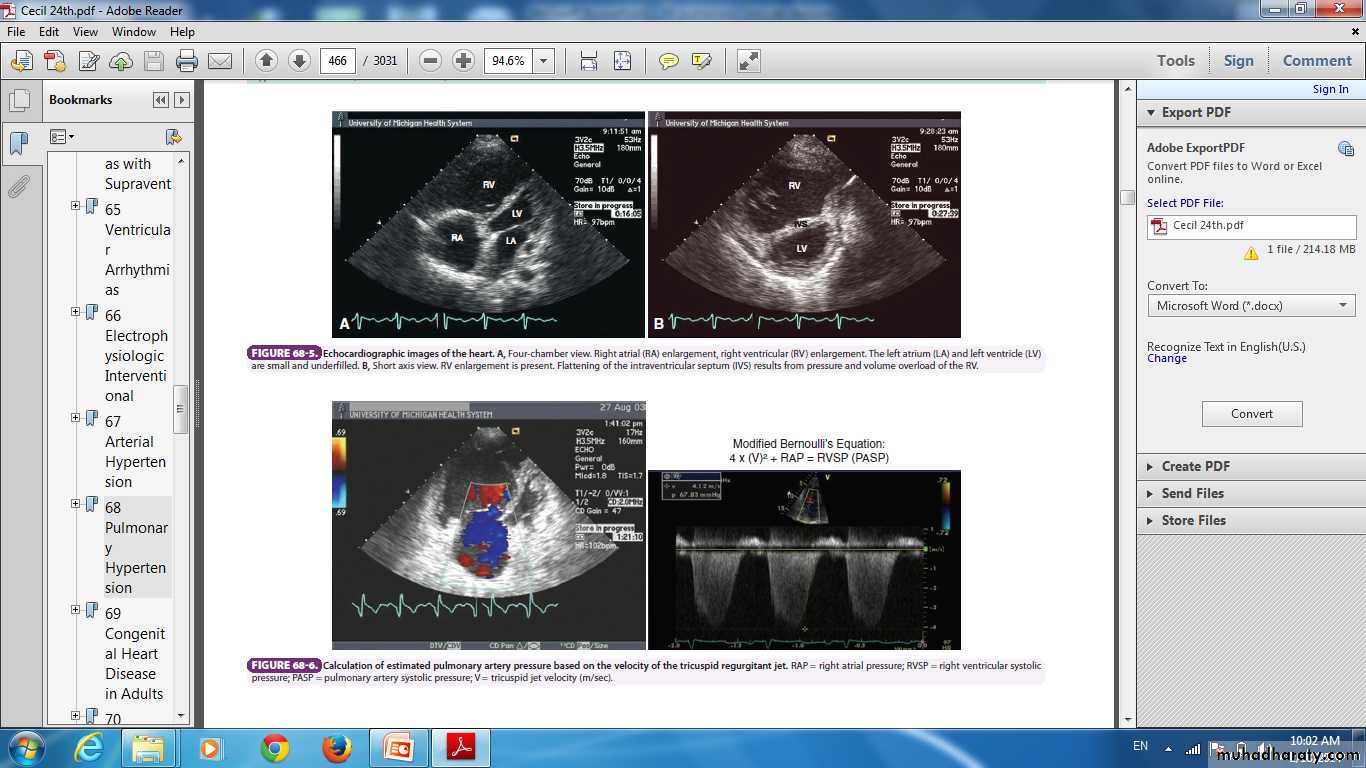
Chest X-ray ,ECG , Echocardiography .
The diagnosis can be confirmed by CT pulmonary angiography.
Treatment
Warfarin and oxygenoral calcium-channel blockers.
oral endothelin receptor antagonists (bosentan).
Prostanoid analogues.
Prognosis
Poor.
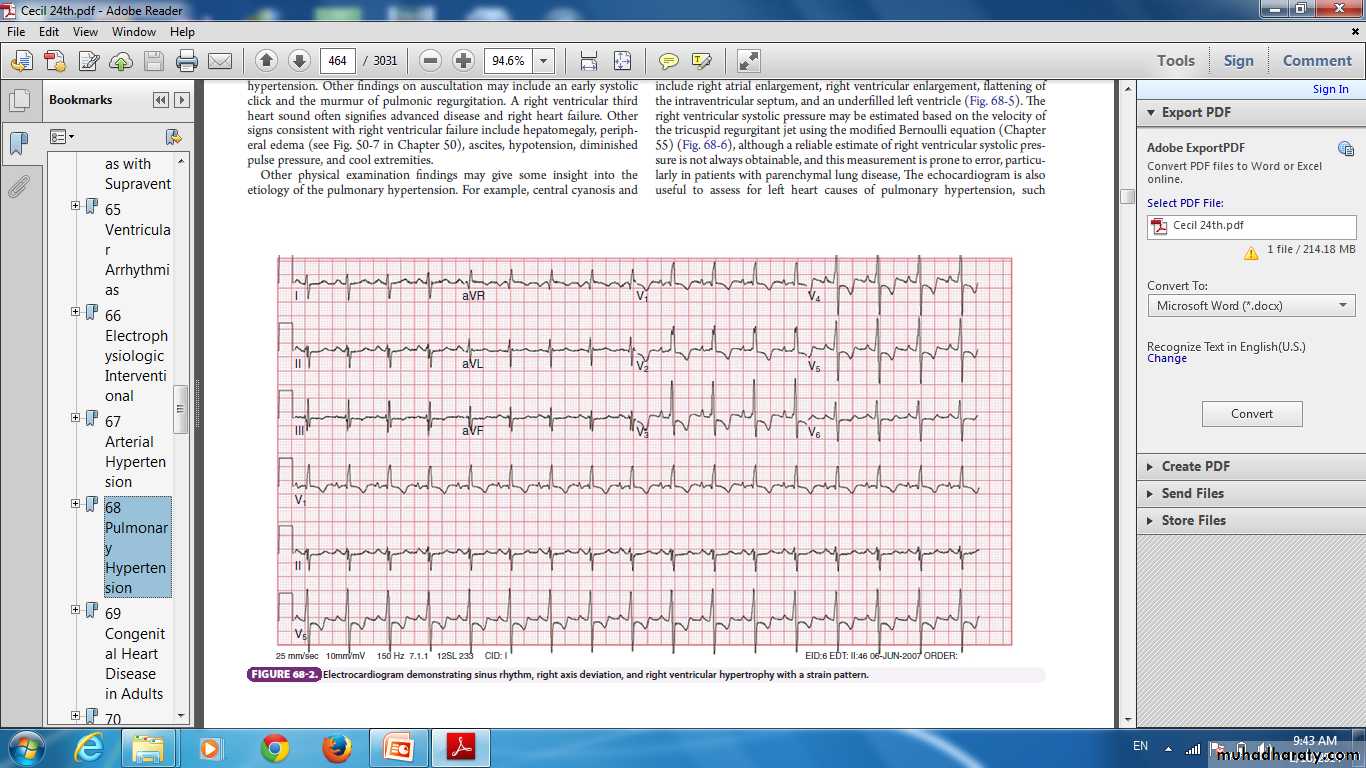
Electrocardiogrm demonstrating sinus rhythm, right axis deviation, and right ventricular hypertrophy with a strain pattern.
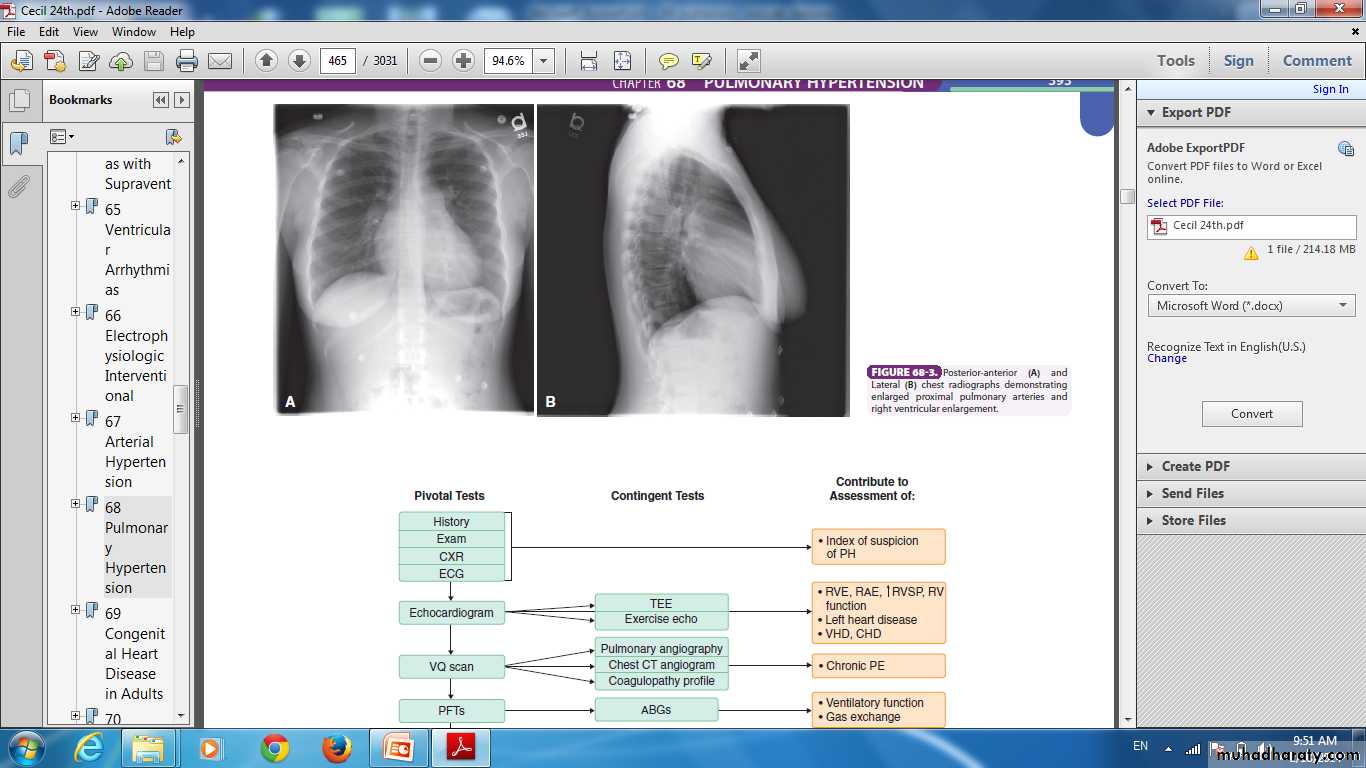
Posterior-anterior (A) andLateral (B) chest radiographs demonstratingenlarged proximal pulmonary arteries andright ventricular enlargement
Chronic Cor Pulmonale
enlargement of the right ventricle because of increase in afterload .Pathophysiology
mechanism varies according to the cause of cor pulmonale.
Hypoxia impairs right ventricular function and, as it develops, left ventricular function is also depressed.Clinical features
Chest pain.exertional dyspnoea.
syncope .
fatigue .
sudden death .
symptoms due the pulmonary hypertension.
physical examination :
signs of pulmonary hypertension.
signs right ventricular enlargement and failure.
Treatment
Diuretic .
oxygen therapy.
Pulmonary Venous Thromboembolism
Essentials of Diagnosisvenous thrombosis, usually of the lower extremities.
dyspnea, chest pain, hemoptysis, syncope.
Tachypnea.
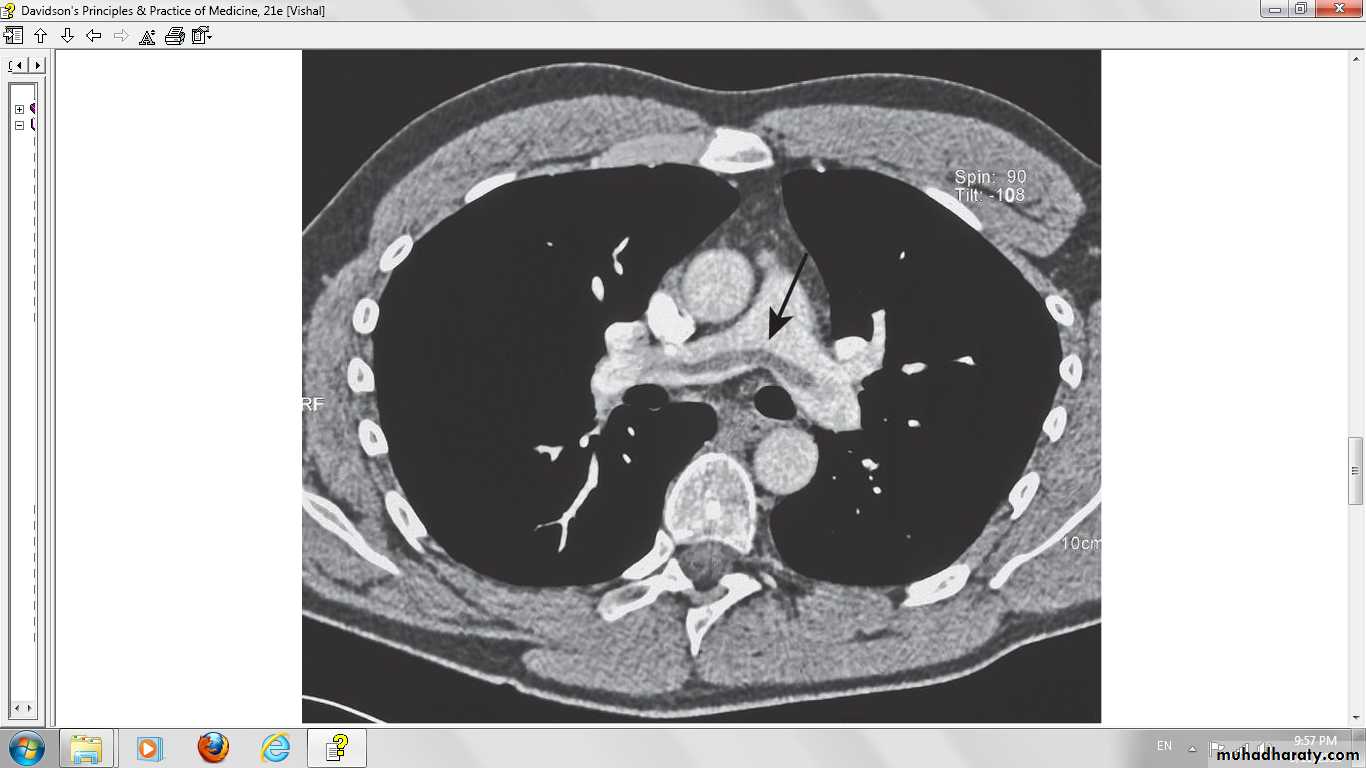
CT scan of the chest.
pulmonary angiogram is diagnostic.
General Considerations
pulmonary embolism (PE), is a common, serious, and potentially fatal.( Massive)200,000 deaths each year in the U.S.A.
The third leading cause of death among hospitalized patients.
Cause of death in PE.
Substances that embolize to the pulmonary circulation:
Air (during neurosurgery, from central venous catheters),
Amniotic fluid (during active labor),Fat (long bone fractures),
Foreign bodies (talc in injection drug users),
Parasite eggs (schistosomiasis),
Septic emboli (acute infectious endocarditis),
Tumor cells (renal cell carcinoma).
The most common embolus is thrombus, which may arise anywhere in the venous circulation or heart but most often originates in the deep veins of the lower extremities.
PE and DVT are two manifestations of the same disease.
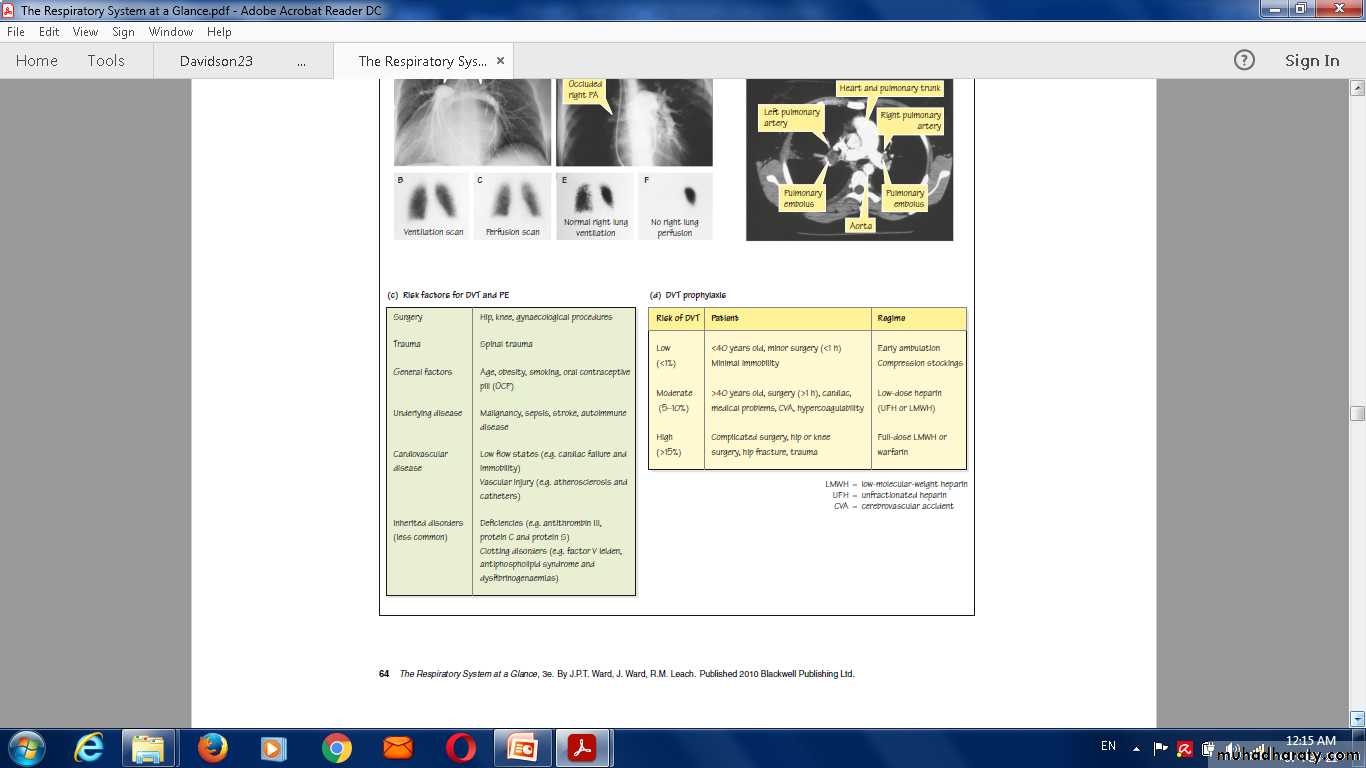
The risk factors for PE and DVT : (Virchow's triad).1-venous stasis.
2- injury to the vessel wall.
3- hypercoagulability.
1-Venous stasis increases
immobility (bed rest—especially postoperative—obesity, stroke).hyperviscosity (polycythemia).
increased central venous pressures (low cardiac output states, pregnancy)
2-Vessels may be damaged by
prior episodes of thrombosis.
orthopedic surgery.
trauma.
3-Hypercoagulability can be caused by
medications (oral contraceptives, hormonal replacement therapy)disease (malignancy, surgery)
pregnancy.
inherited gene defects.
• 1-activated protein C, also known as factor V Leiden.
• 2-deficiencies or dysfunction of
• - protein C.
-protein S.
-antithrombin III.
CATEGORISATION OF PULMONARY THROMBOEMBOLI
AM- Acute Massive PE
SM-Acute small/medium PE
C- Chronic PE
Pathophysiology
AM-Major haemodynamic effects: ↓ cardiac output; acute right heart failureSM-Occlusion of segmental pulmonary artery → infarction ± effusion
C-Chronic occlusion of pulmonary microvasculature, right heart failure
Symptoms
AM-Faintness or collapse, central chest pain, apprehension, severe dyspnoeaSM-Pleuritic chest pain, restricted breathing, haemoptysis
C- Exertional dyspnoea. Late symptoms of pulmonary hypertension or right heart failure
Signs
AM- Major circulatory collapse: tachycardia, hypotension, ↑ JVP, right ventricular gallop rhythm, split P2 Severe cyanosis ↓ Urinary output
SM- TachycardiaPleural rub, raised hemidiaphragm, crackles, effusion (often blood-stained)Low-grade fever
C- May be minimal early in diseaseLater-RV heave, loud, split P2Terminal-right heart failure
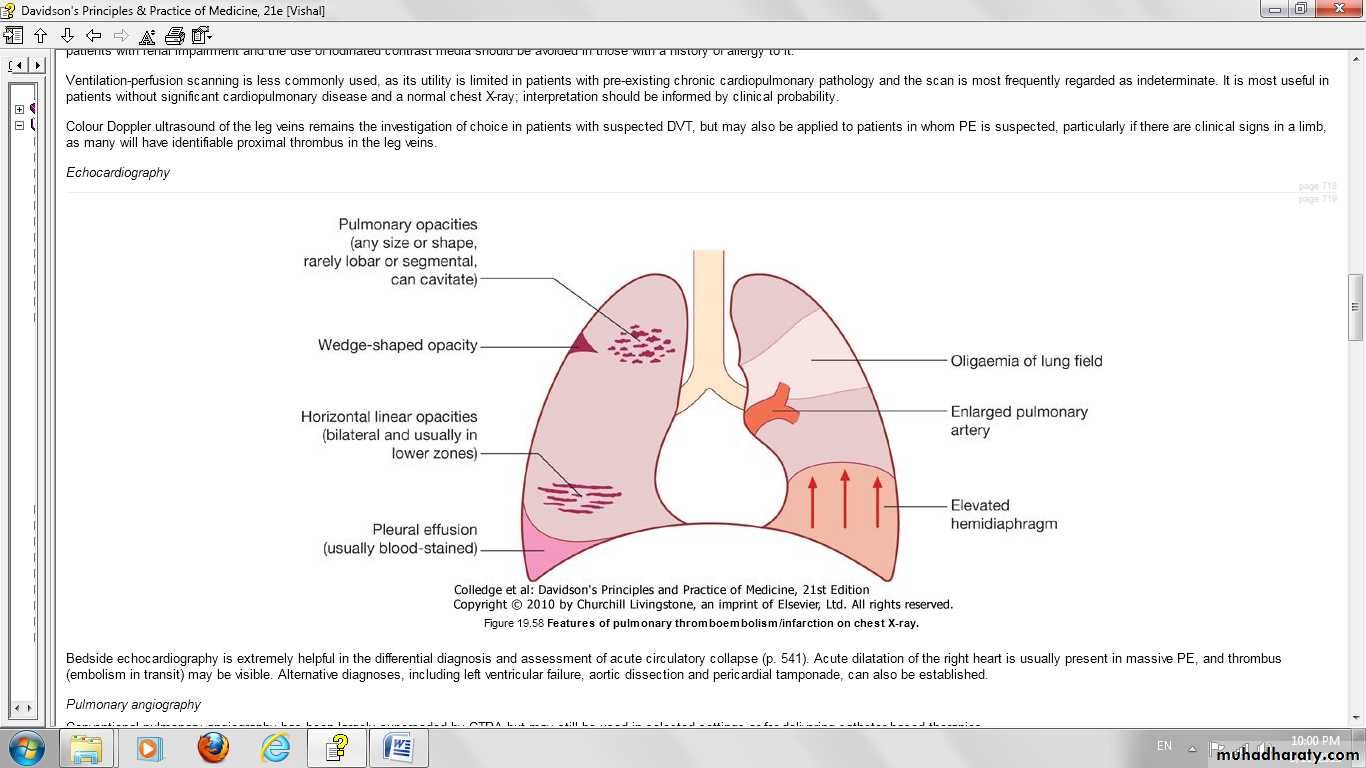
Chest X-ray
AM-Usually normal.
May be subtle
oligaemia
SM-Pleuropulmonary opacities, pleural effusion, linear shadows, raised hemidiaphragm
C-Enlarged pulmonary artery trunk, enlarged heart, prominent RV
ECG
AM- S1 Q3 T3 anterior T-wave inversion Right bundle branch block (RBBB).
SM- Sinus tachycardia.
C- RV hypertrophy and strain.
Arterial blood gasesAM-Markedly abnormal with ↓ PaO2 and
↓ PaCO2. Metabolic acidosisSM- May be normal or ↓ PaCO2
C-Exertional ↓ PaO2 or desaturation on formal exercise testing
Alternative diagnoses
AM-Myocardial infarction; pericardial tamponade; aortic dissection
SM-Pneumonia, pneumothorax, musculoskeletal chest painC-Other causes of pulmonary hypertension
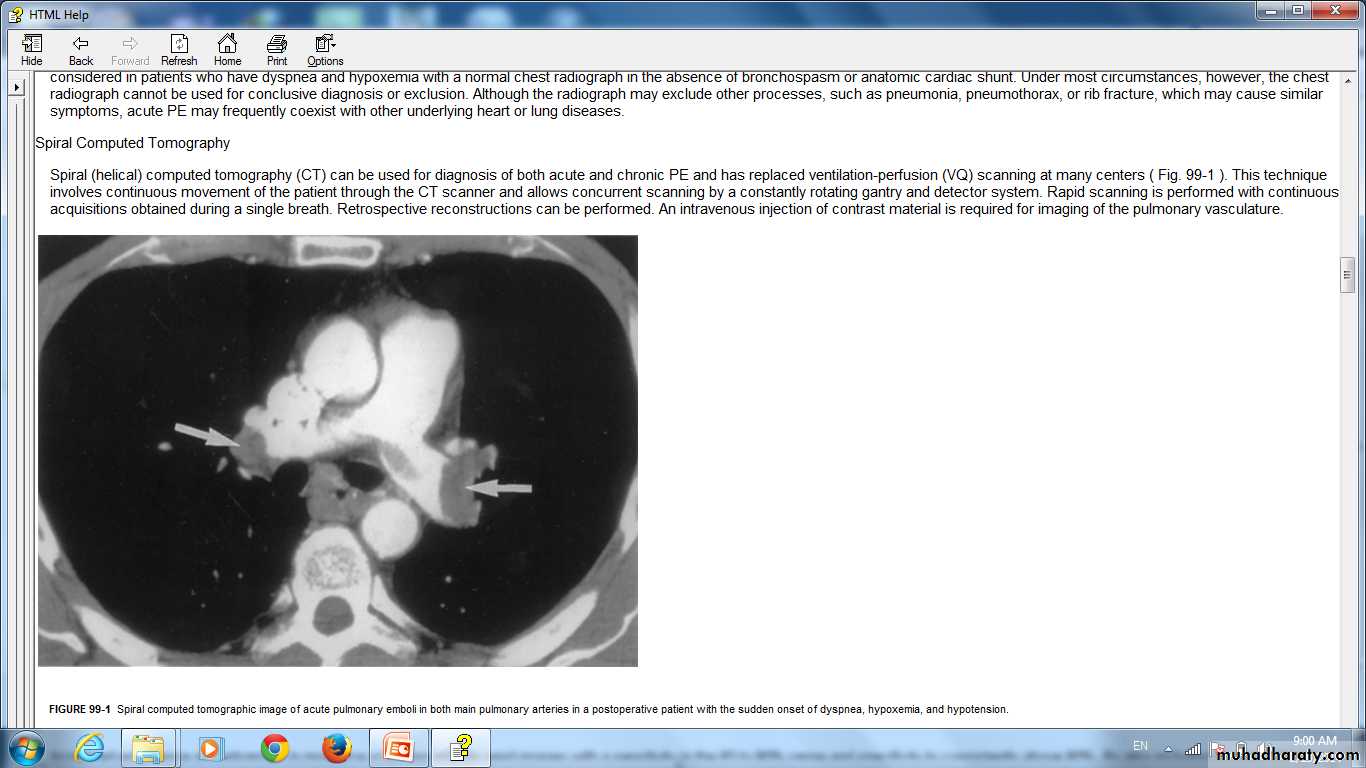
Spiral computed tomographic image of acute pulmonary emboli in both main pulmonary arteries in a postoperative patient with the sudden onset of dyspnea, hypoxemia, and hypotension.
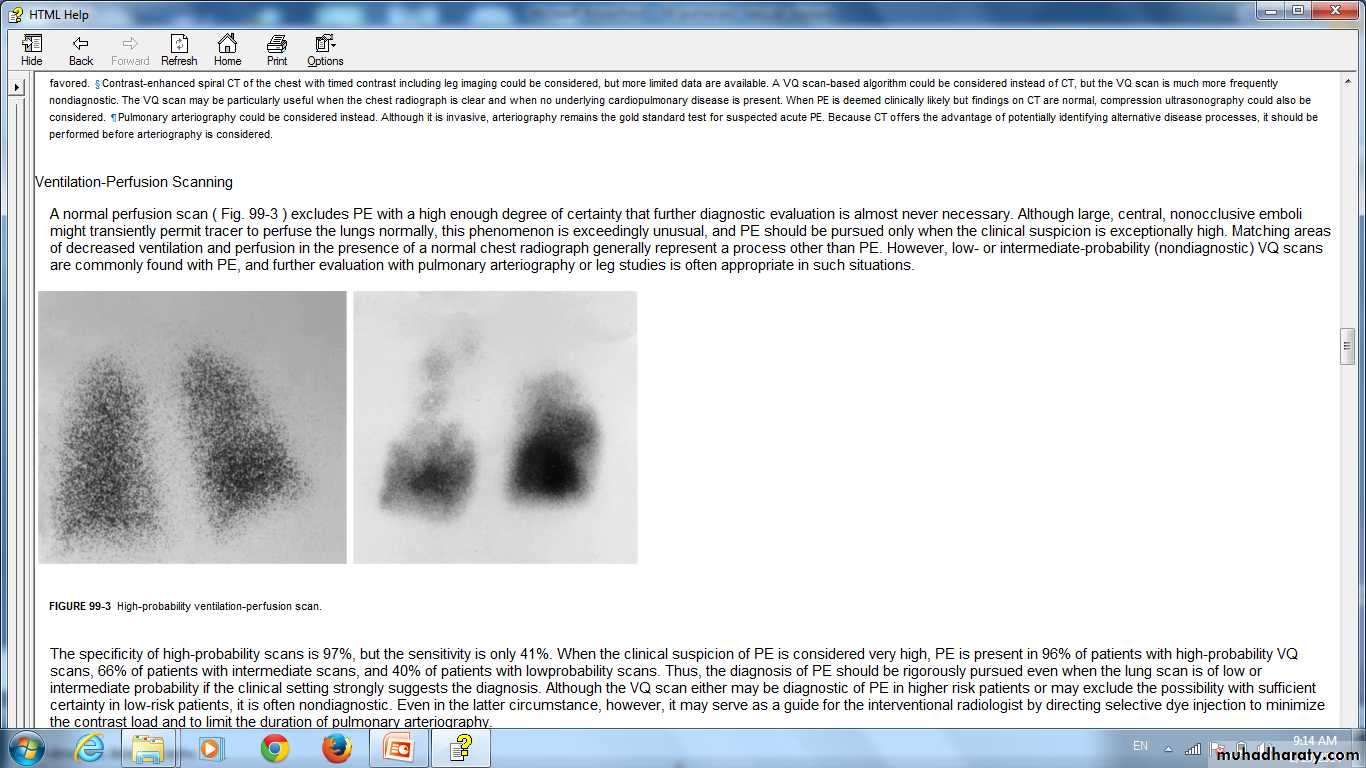
High-probability ventilation-perfusion scan.
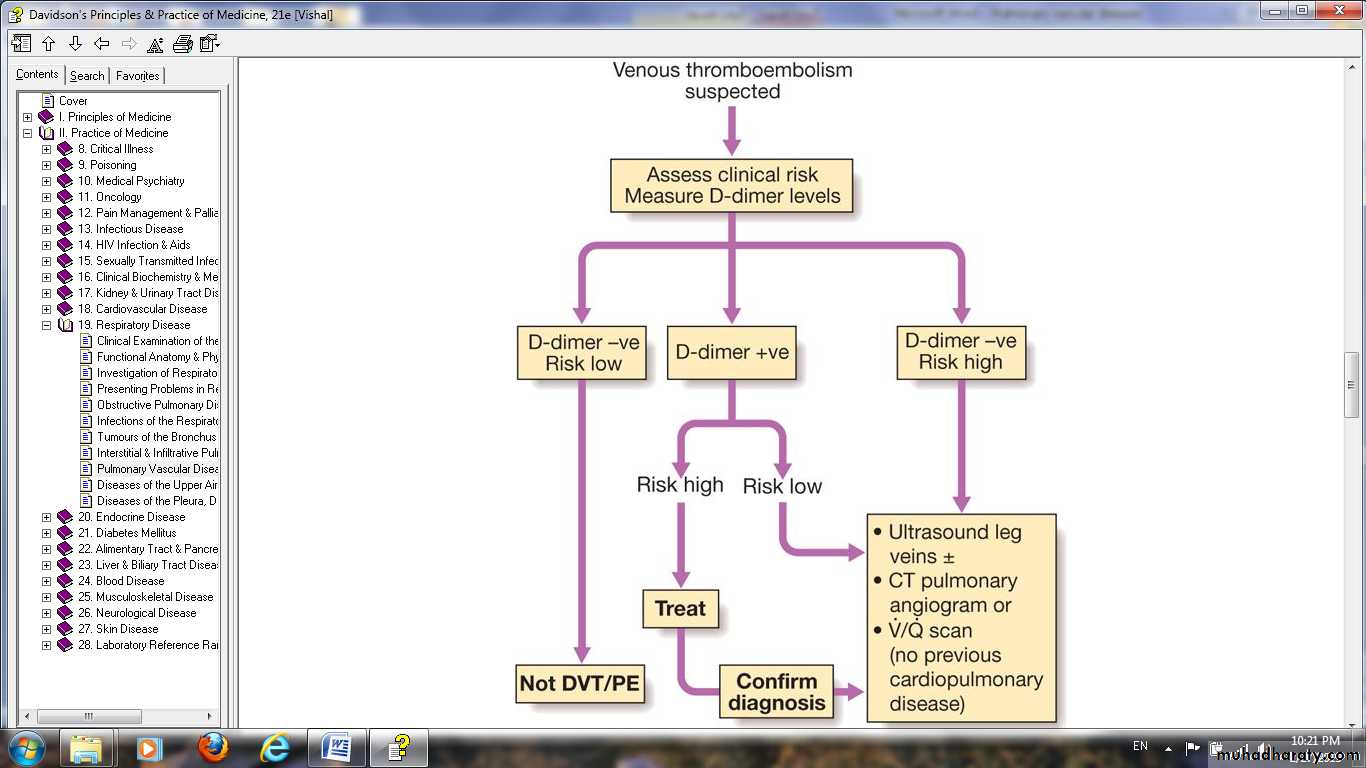
Laboratory Findings
Arterial blood gases.Plasma D-dimer, .
Serum troponin I, troponin T, and plasma beta-natriuretic peptide (BNP) levels.
Lung scanning
CT
Helical CT pulmonary angiography sensitive and very specific.
Venous thrombosis studies
venous ultrasonography, the test of choice to detect proximal DVTimpedance plethysmography.
contrast venography.
Pulmonary angiography
MRI
Prevention
ManagementManagment
General measures
Oxygen should be given to all hypoxaemic patientsOpiates may be necessary to relieve pain and distress
hypotension should be treated by giving intravenous fluid or plasma expander.
Resuscitation by external cardiac massage .
Anticoagulation
'Low molecular weight heparins.'Continued using oral warfarin.
The international normalised ratio (INR) is greater than 2.
Duration of warfarin therapy :variable 3 months- for life.
Thrombolytic therapy …INDICATIONS
Caval filters : INDICATIONS.Plmonary Vasculitis
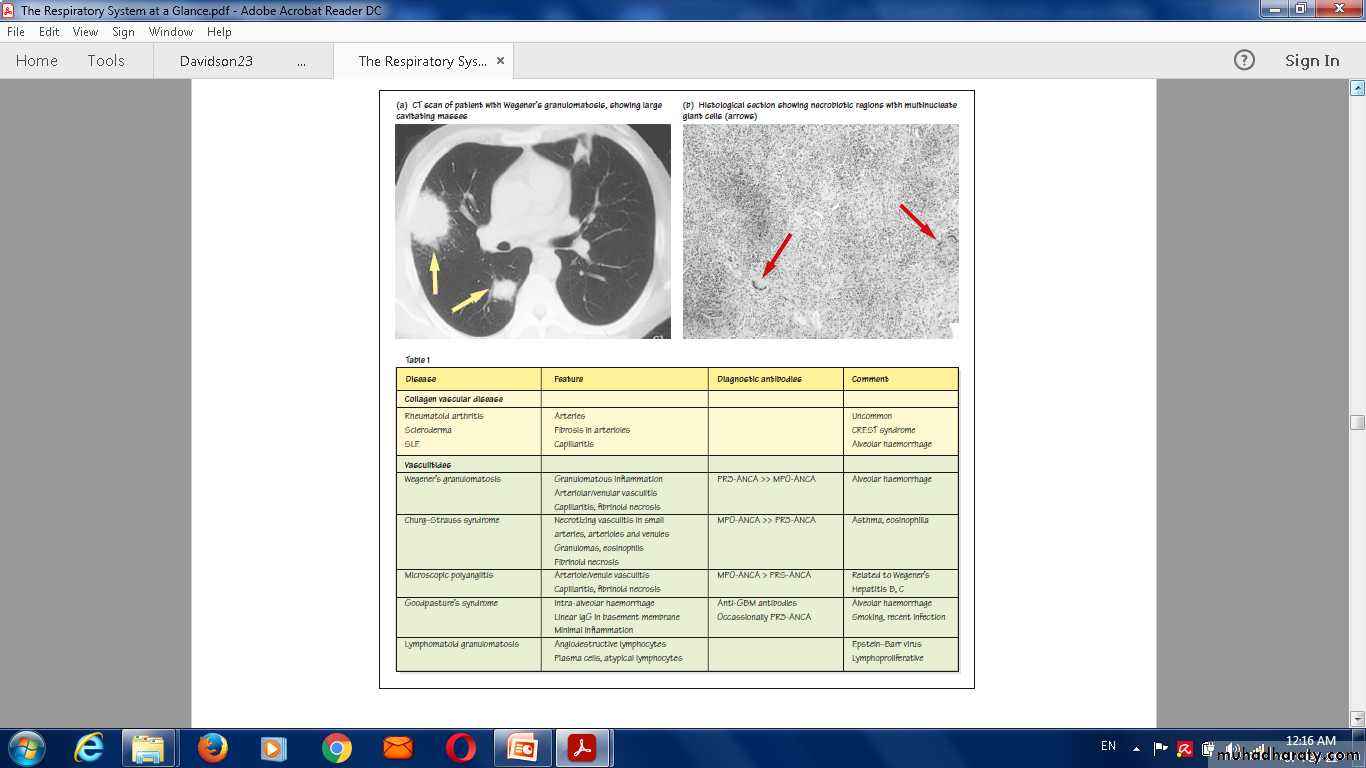
Wegener's granulomatosisdiagnosis
serologic testing and biopsy of lung .
Allergic angiitis and granulomatosis (Churg-Strauss syndrome)
an idiopathic multisystem vasculitis of small and medium-sized arteries that occurs in patients with asthma.
Treatment : corticosteroids and cyclophosphamide.
Alveolar Hemorrhage Syndromes
immune and nonimmune disorders.
Hemoptysis, alveolar infiltrates on chest radiograph, anemia, dyspnea, and occasionally fever are characteristic.
immune alveolar hemorrhage
Nonimmune causes diffuse hemorrhage
coagulopathy.
mitral stenosis.
Idiopathic pulmonary hemosiderosis .
Q