Functions of the liver :
general metabolic functions :Synthesis of glycogen postprondialy and storage of excess glucose, , during fasting the plasma glucose concentration is maintained by breakdown of stored glycogen or by synthesis of glucose from such substrate as glycerol , lactate and amino acids by gluconeogensis , and also the metabolism of vitamins and minerals.
Synthetic functions : the hepatocyte synthesize : 1- plasma protein except immunoglobulin and complement.
2- most coagulation factors including fibrinogen and factorII (prothrombin), factors V,VII, IX, X, XI, XII, and XIII.
3- lipoproteins: such as VLDL and HDL .
4- primary bile acids.
• Excretion and detoxification function :
• Excretion of bilirubin is very important, other substances which are inactivated and excreted by liver include :• amino acid : which are deaminated in the liver , the ammonia produced by intestinal bacterial action and absorped into the portal vein are converted to urea .
• cholesterol : which is excreted in the bile .
• Steroid hormones : which are metabolized by conjugation with glucuronate and sulphate and are excreted in the urine in these water-soluble forms.
• Many drugs : which are metabolized and inactivated by enzymes of endoplasmic reticulum and some are excreted in the bile .
• Toxins : the reticuloendothelial Kupffer cells in the hepatic sinusoids are well placed to extract toxic substances that have been absorbed from the gastrointestinal tract.
Bilirubin metabolism and jaundice :
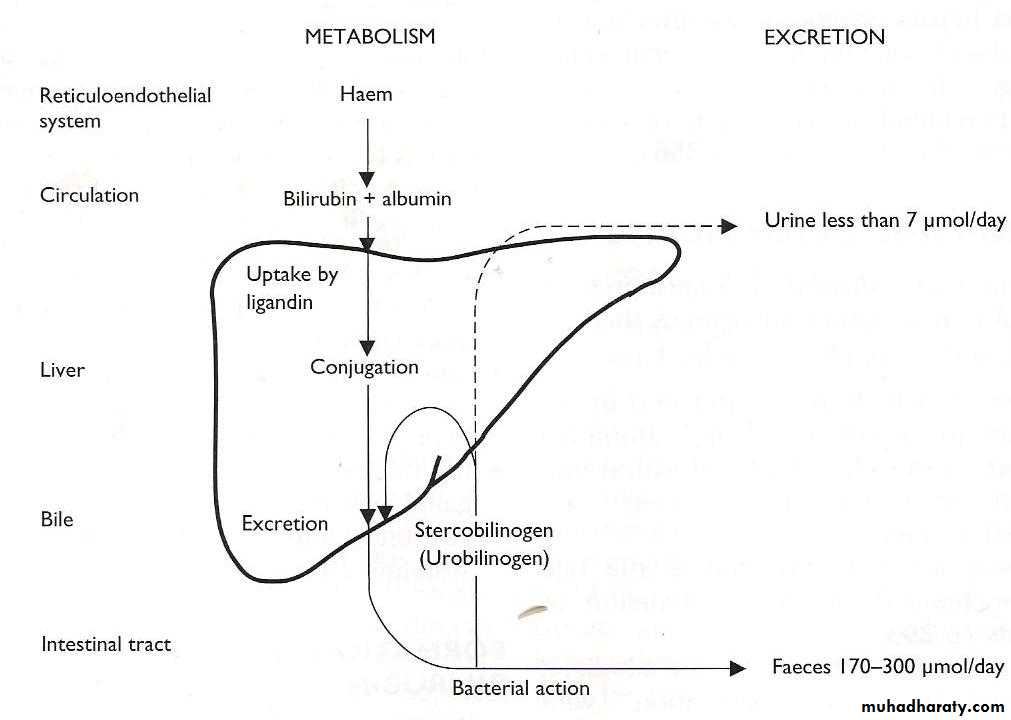
* At the end of their lifespan of RBC which is 120 days are broken down by reticuloendothelial system , mainly in spleen .The released Hb is split into globin and haem .
Haem will converted to bilirubin after removal of iron , the iron reabsorbed and reutilized for B.M. to be used for synthesis of new RBC or to the liver to be stored as ferritin .
About 80 % of bilirubin is derived from the breakdown of haem within the RES , other sources include breakdown of immature RBCs in the bone marrow and compounds chemically related to haemoglobin such as myoglobin and the cytochromes.
* The released bilirubin in the blood will bind with albumin to form protein bound bilirubin or unconjucated (indirect ) which is not water soluble and doesn’t pass in the urine ,
* (Unconjucated bilirubin produced 250-300 ϻmol daily ) from catabolism of haem , while the liver normally able to conjugate up to 1 mmol/ day
Most of unconjucated bilirubin go to the liver and it released from albumin to hepatocyte, it is actively transported to smooth ERC and conjugated by uridyl diphosphate (UDP) glucuronyl transferase , to form conjugated or direct bilirubin (water soluble bilirubin) .
* Most of conjugated bilirubin enter the gut in bile , it is broken down by bacteria in the distal ileum and colon to groups of product known as stercobilinogen (faecal urobilinogen)
* Some is absorbed in portal and most of it is reexcreated within bile (entero-hepatic circulation) , small fraction enters the systemic circulation and excreted in the urine as urobilinogen which can be oxidized to the colored pigment (urobilin) .
• Urinary urobilinogen is increased by (exaggurated of normal phenomena ) of urobilinogen formation :
• haemolysis is sever : large amount of bilirubin enter the bowel lumen and are converted to stercobilinogen an increased amount of urobilinogen is formed .
• liver damage : impair reuptake of normal amount of urobilinogen into the bile.
• Unabsorbed stercobilinogen is oxidized to stercobilin , a pigment which contribute to the brown color of faeces.
• Pale stool may , therefore suggest biliary obstruction.
• Urobilinogen and stercobilinogen are colorless .
• Bilirubin , urobilin and stercobilin are colored (Bile pigment).
.
• Jaundice (icterus):
• It is refer to yellowish discoloration of the skin , sclerae and mucous membrane resulting from increased bilirubin concentration in the body fluid , it is usually detectable clinically when the plasma bilirubin exceed ( 3mg/dl) 50 Mmol/L .• Clinical classification of jaundice :
• prehepatic jaundice : due to increase haemolysis of RBC such as SCA , thalassaemia , hereditary spherocytosis, drugs……etc , in this type mainly increased the indirect bilirubin , increase LDH1 and LDH2 , reticulocytosis and low plama haptoglobin but all the liver function tests are normal . there is common condition which is similar to this type of jaundice by normal LFT with indirect hyperbilirubinemia this condition is called Gilbert disease , but it differentiated from haemolytic jaundice by normal reticulocyte count.
• Hepatocellular jaundice : result from an inability of the liver to transport bilirubin into the bile due to paranchymal liver disease , bilirubin transport across the hepatocyte may be impaired at any point between uptake of unconjugated bilirubin into the cells and transport of conjugated bilirubin into canaliculi .
In hepatocellular jaundice , both conjucated and unconjugated bilirubin increase because disturbance of bilirubin transport across hepatocyte are variable at any point as mention above
Liver enzymes (SGOT and SGPT) which are enzyme from hepatocyte markedly increase in this type of jaundice ,
Alkaline phosphatase also moderately increase due to disturbance of cancliculi ,
The other important investigation which should be measured here is prothrombin time (PT) which is prolonged due to coagulation defect i.e. liver responsible for synthesis of most of coagulation factors , so when it impaired , this will lead to prolong (PT) , so this test is important for diagnosis and prognosis .
When hepatocellular damage prolong more than one month we found that serum albumin concentration also decrease but not in few days due to half life of albumin more than three weeks , so this test important to diagnosis the chronicity of the disease .
• 3 - cholestatic jaundice :
• This type result from obstruction at any site of biliary pathway i.e. from small canaliculi to larger one , hepatic duct , common hepatic duct until common bile duct .• increased bilirubin in this type of jaundice is mainly conjugated type because conjugation occurred in hepatocyte which is normal here.
• increased alkaline phosphatase( ≥ 3 fold) in obstructive jaundice because the enzyme synthesize in the biliary cells , not like SGOT and SGPT in the hepatocytes which are increased here mildly due to biliary back pressure .
• Patients with prolonged and more widespread cholestasis may present with pruritus due to the deposition of retained bile salts in the skin.
• Prothrombine time in this type also prolong with bleeding (but lately) not due to coagulation factors defect, but because of vitamin K deficiency due to malabsorption of vitamin K .
• Cholesterol retention may cause hypercholesterolaemia.
• Dark urine and pale stools suggest biliary retention of conjugated bilirubin.
Cholestasis may be either :
● Intrahepatic: in which bile secretion from the hepatocytes into the canaliculi is impaired, due to:
– viral hepatitis,
– drugs such as chlorpromazine or toxins such as alcohol,
– inflammation of the biliary tract (cholangitis),
– autoimmune disease (primary biliary cirrhosis),
– cystic fibrosis .
● Extrahepatic : due to obstruction to the flow of bile through the biliary tract by:
– biliary stones,
– inflammation of the biliary tract,
– pressure on the tract from outside by malignant tissue, usually of the head of the pancreas,
Bile acids and bile salts :
Four bile acids are produced in human , two of these cholic acid and chenodeoxycholic acid are synthesized in the liver from cholesterol and are called primary bile acids . they are secreted in the bile as sodium salts , conjugated with amino acids glycine or taurine to form primary bile salts.These are converted by bacterial action within the intestinal lumen to secondary bile salts (deoxycholate and lithocholate) respectively.
Secondary bile salts are actively absorped from terminal ileum and are reexcreted with bile by the liver (enterohepatic circulation of bile salts).
Bile therefore contain mixture of primary and secondary bile salts .
During absorption of meal , the conjugated bile salts must be present in small intestine in sufficient concentration for formation of micelles. The monoglyceride and free fatty acid aggregate with bile salts to form water-miscible micelles, the micelles also contain free cholesterol (liberated from hydrolysis of cholesterol ester in the lumen) and phospholipids, as well as the fat soluble vitamin. The diameter of the negative charge micelles is small that allow it to pass through the microvillous spaces.
Deficiency of conjugated bile salts in the intestinal lumen lead to impaired micelle formation and malabsorption of fat , and can occur in the following circumstances :
• insufficient synthesis of bile salts in the liver (e.g. liver cirrhosis).
• Obstruction to the outflow of bile (e.g. gall stone).• Interruption of enterohepatic circulation :
• failure of bile salt absorption from intestine (e.g. ileal disease or resection).
• abnormal bacterial colonization of the upper small intestine , some colonizing bacteria split the bile salts conjugates reducing their effective concentration at the site of fat absorption
Liver function tests :
• bilirubin.
• Aminotransferase ALT and AST .
• Alkaline phosphatase.
• ∂-glutamyl transferase GGT.
• Protein (total protein and albumin)
• Coagulation tests.
Bilirubin :
two type conjugated and unconjugated , the conjugated increasemore than unconjugated in hepatocellular jaundice and obstructive jaundice while in prehepatic type (haemolysis or Gilbert diseases) there is increase in uncojugated type while the conjugated bilirubin is normal.
2- Aminotransferase:
These are alanine aminotransaminase ALT (GPT) and aspartate aminotransferase AST (GOT)
Both ALT and AST are located in cytoplasm of the hepatocyte ,
an alternative form of AST is also located in the hepatocyte mitochondria , although both transaminase enzyme are widely distributed in the other tissue of the body. The activities of ALT out side the liver are low (skeletal muscles, kidney and heart) and therefore thisenzyme is consider more specific for hepatocellular damage.
1
* Liver cells contain more AST than ALT , but ALT is confined to cytoplasm in which its concentration is higher than of AST.
* Raised plasma transaminase are indicative for hepatocellular damage,
* In inflammatory or infective conditions, such as viral hepatitis, the cytoplasmic membrane sustains the main damage , leakage of cytoplasmic contents causes a relatively greater increase in plasma ALT than AST activities.
* In infiltrative disorders in which there is damage to both mitochondrial and cytoplasmic membranes, there is a proportionally greater increase in plasma AST than ALT activity.
• alkaline phosphatase (ALP) :
The ALP are group of enzymes which hydrolyse phosphate at high PH , it is widely distributed in the body , with significant activities in the liver , GIT , bone and placenta.
In the liver they are localized in the sinusoidal and biliary canalicular mem.
It is most sensitive test for intra or extrahepatic cholestasis ,
A raised ALP concentration in the presence of a raised g-glutamyl transferase (GGT) concentration implies that the ALP is of hepatic origin.
• ∂- glutamyl transferase (GGT) :
originated from ERC of the cells of hepatobiliary tract .As this reticulum proliferates, for example in response to the prolonged intake of alcohol and of drugs such as phenobarbital and phenytoin, synthesis of the enzyme is induced and plasma GGT activity increases.
plasma GGT higher in men than women , raised plasma activities do not necessarily indicate hepatocellular damage, but may reflect enzyme induction or cholestasis. en. It is mainly increased in alcoholic liver disease or enzyme inducer drugs like (phenytoin and rifampicin) .
• Protein (serum albumin):
liver produce (8-14) gm/day of albumin but the reduction in serum albumin observed with liver diseases involve changes in the volume of distribution of albumin in addition to reduction in the synthesis. Reduction in serum albumin in case of liver disease Indicate chronicity due to the long half life of albumin (28 days).• Coagulation test :
the liver synthesize most coagulation factors and required vitamin K to activate factor X, IX, VII and II . sever liver damage and prolong biliary obstruction (the later reduce vitamin K absorption) are associated with reduce plasma fibrinogen concentration and prolong PT. the half life of vitamin K depedant coagulation factor are short (5-72) hrs , therefore change in the PT occur quickly following liver damage and provide prognostic information in patient with acute and chronic liver failure.The prothrombin time may be prolonged by cholestasis: fat-soluble vitamin K cannot be absorbed normally if fat absorption is impaired due to intestinal bile salt deficiency.
Jaundice in the newborn infant :
Red cell destruction, together with immature hepatic processing of bilirubin, may cause a high plasma level of unconjugated bilirubin in the newborn infant; so called physiological jaundice is common.Normal fullterm babies may show jaundice between days 2 and 8 of life. Physiological jaundice rarely exceeds 100 µmol/L. Jaundice on the first day of life is invariably pathological, as are levels of bilirubin exceeding 100 mmol/L or if the hyperbilirubinaemia is conjugated.
As a result of haemolytic disease, the plasma concentration of unconjugated bilirubin may be as high as 500 µmol/L and may exceed the plasma protein-binding capacity; free unconjugated bilirubin may be deposited in the brain, causing kernicterus. Proportionally more unconjugated bilirubin reaches the liver in the newborn infant than in the adult due to The RBC half-life is shorter; the blood haemoglobin concentration falls rapidly during the first week of life, even in normal infants , and also delayed clamping of the umbilical cord may significantly increase red cell mass.
.
Physiological jaundice (indirect hyperbilirubinaemia) is defined as mild jaundice which is not present at birth but which develops during the first few days and continues during the first 10 days of life, and for which there is no obvious pathological reason. Such jaundice is very common in normal newborn infants (about 50 per cent of normal babies develop this after 48 h) , The plasma total bilirubin rarely exceeds 200 µmol/L, with the conjugated bilirubin unlikely to be greater than 40 µmol/L , Physiological jaundice can be aggravated by prematurity, infections, dehydration, hypoxia and poor nutrition .
Kernicterus is a serious complication which may result in permanent brain damage or death. The risk of kernicterus is increased :
● the more premature the infant,
● if theplasma indirect bilirubin concentration is rising rapidly(sever haemolysis)
● if the bilirubin-binding capacity is low, due to :
– hypoalbuminaemia,
– displacement of bilirubin from albumin by some drugs,
– displacement of bilirubin from albumin by hydrogen ions in acidosis due to hypoxia or other serious illness.
\
Jaundice during the first 24 h of life is more likely to be pathological than physiological. It may have the following causes :
● ABO blood group incompatibility .
● Inherited erythrocyte abnormalities associated with haemolysis, such as glucose-6-phosphate dehydrogenase deficiency, pyruvate kinase deficiency or hereditary spherocytosis.● Intrauterine infections that affect the liver, such as syphilis, rubella or toxoplasmosis.
Unconjugated hyperbilirubinaemia
Gilbert’s syndrome :This is a relatively common (3–7 per cent of the population) familial condition, which may be present at any age but usually develops after the second decade. Plasma unconjugated bilirubin concentrations are usually between 20 µmol/L and 40 µmol/L and rarely exceed 80 µmol/L. They fluctuate, and may rise during intercurrent illness, dehydration, menstruation and fasting. The condition is probably harmless but must be differentiated from haemolysis and liver disease.
Mutations in the hepatic uridine diphosphate glucuronyl transferase (UGT) gene are present with decreased activity to approximately 30 per cent of normal
It should be remembered that sometimes thyrotoxicosis can cause raised unconjugated bilirubin due to reduced UGT activity , and so can reabsorption of a large haematoma due to haemoglobin breakdown .
Crigler–Najjar syndrome :
This is due to a rare deficiency of hepatic UGT, and is a more serious condition. It usually presents at birth.
The plasma unconjugated bilirubin may increase to concentrations that exceed the binding capacity of albumin and so cause kernicterus.
The defect may be
complete (type I), and inherited as an autosomal recessive condition,
or partial (type II), and inherited as an autosomal dominant condition.
:Acute hepatitis
1-Viral hepatitis● Hepatitis A (‘infectious hepatitis’)
● Hepatitis B (‘serum hepatitis’)
● Hepatitis C (non-A, non-B hepatitis)
In all types there may be a 3- to 4-day history of anorexia, nausea and tenderness or discomfort over the liver before the onset of jaundice. Some patients remain anicteric. Plasma aminotransferase activities are very high from the onset of symptoms; they peak about 4 days later, when jaundice becomes detectable, but may remain elevated for several months. Once jaundice appears, some of the initial symptoms improve.
Plasma bilirubin concentrations is elevated , and the plasma ALP moderately raised, or even normal. If hepatocellular damage is severe and extensive, the prothrombin time may be increased .
2- Alcoholic hepatitis
Alcoholic hepatitis occurs in heavy drinkers, often after a period of increased alcohol intake. Although the clinical features may mimic acute viral hepatitis, the plasma aminotransferase activities and bilirubin concentration are not usually as markedly elevated, although GGT may be.A raised (MCV), hypertriglyceridaemia , hyperuricaemia and elevated plasma GGT
3-Drugs and other toxins
Various drugs and other toxins are hepatotoxic, sometimes directly and sometimes due to a hypersensitivity reaction . The clinical picture may resemble that of acute viral hepatitis or cholestasis.
A drug history is an essential part of the assessment of a patient presenting with liver disease such as paracetol, cytotoxic drugs , aspirin , phenytoin …etc
INVESTIGATION OF SUSPECTED LIVER DISEASE
The commonly available biochemical laboratory tests for the diagnosis of liver disease involve the measurement of plasma levels of :● bilirubin – excretory function,
● aminotransferases (ALT and/or AST) – hepatocellular damage,
● alkaline phosphatase – cholestasis,
● albumin and/or prothrombin time – synthetic function,
● ɤ-glutamyl transferase – enzyme induction, cholestasis or hepatocellular damage.
● Measure plasma bilirubin and unconjugated/ conjugated bilirubin fractions: Predominantly unconjugated hyperbilirubinaemia with plasma conjugated bilirubin levels less than about 10 per cent of the total, and with little or no bilirubinuria, may suggest haemolysis as a cause.
Haemolysis is supported by a raised reticulocyte count and diagnostic blood film, reduced plasma haptoglobin and raised plasma lactate dehydrogenase concentrations.
.
If haemolysis is excluded, consider Gilbert’s syndrome provided other liver tests are normal and other hepatic disorders have been excluded.
● A fresh urine sample should be examined. This test may show the presence of bilirubin if conjugated hyperbilirubinaemia is present. Dark-yellow or brown urine suggests biliary obstruction ,
An absence of urinary urobilinogen is seen in biliary obstruction.
Reagent strips are available for testing for bilirubin and urobilinogen in urine.
● Pale stools suggest biliary obstruction as a cause of jaundice.
plasma aminotransferase, ALP and GGT assays:
– In hepatitis, there is a predominant increase in the concentrations of plasma aminotransferases; usually the plasma ALT activity is higher than the AST activity.
– In cholestasis, there is predominant elevation of the plasma ALP and GGT activities. Bile duct dilatation should be sought using ultrasound or other radiological tests:
if the plasma ALP activity is high but dilated ducts are not demonstrated, there is probably intrahepatic cholestasis.
.
● If acute alcoholic hepatitis is suspected, there may be the finding of high plasma GGT activity compared with those of the aminotransferases. There may also be macrocytosis, hypertriglyceridaemia and hyperuricaemia.
● In obstructive jaundice (biliary obstruction), the plasma ALP is usually more than four to five times and GGT more than 10 times normal .
● Check hepatitis serology, for example A, B and C.
● Plasma protein electrophoresis and immunoglobulin assay may help in the diagnosis of:
– cirrhosis – high plasma IgG and IgA concentrations causing β–ɤ fusion on the electrophoretic strip,
– alcoholic cirrhosis – may present with raised IgA concentration,
– chronic active hepatitis – a high plasma IgG concentration and normal IgA,
– primary biliary cirrhosis – a high plasma IgM concentration .