Physical factors & the skin
Dr. Hadaf AljunaiyehProfessor dermatology
College of medicine/ thi qar university
objectives
By the end of this lecture, the student should be able to:Classify the main physical factors in the environment
Describe the skin changes induced by these factors
Recognize the main preventive measures for these conditions
& their best treatment modalities.
Physical factors in the environment
HeatCold
Sun
Physical pressure
Radiation
heat
Burn
Miliaria
Erythema ab igne
burn
ThermalElectrical
burn1st degree: only erythema + sometimes desquamation & constitutional symptoms if a large area is involved
2nd degree: A- superficial B- deep
superficial deep
causing vesicles & bullae causing pallor
heal without scarring delayed healing with scarring
3rd degree: full thickness loss of tissue with scarring
miliaria
Occlusion of eccrine sweat gland leading to retention of sweat with failure of delivery of sweat to the skin surfaceEventually backed-up pressure causes rupture of sweat gland or duct at different levels
Escape of sweat into adjacent tissue produces miliaria
Common in hot, humid climates
Different forms of miliaria occur depending on the level of injury to the sweat gland
1- Miliaria crystallina
Small, clear, superficial vesicles without inflammationAppears in bedridden patients and bundled children
Lesions are asymptomatic and rupture at the slightest trauma.
Self-limited; no treatment is required.
2-Miliarai rubra
Discrete, extremely pruritic, erythematous papulovesicles with sensation of prickling, burning, or tingling.Site of injury is prickle cell layer.
3-Miliaria profunda
Occlusion is in the papillary dermisOnly seen in tropics
Rare in our country
Deep seated flesh colored papules
asymptomatic
treatment
Mild cases respond to cooling of skinPlace patient in a cool environment
Use dusting powder as talcum
Cooling baths of menthol & corn starch
Emollients & steroid ointment to dissolve keratin plugs
& restore sweating
Erythema ab igne
Persistent erythema or the coarsely reticulated residual pigmentation resulting from it, due to long exposure to excessive heat without burn.First transient, then permanent
Mostly on the legs of women
May cause epithelial atypia, rarely Bowen’s disease or squamous cell carcinoma.
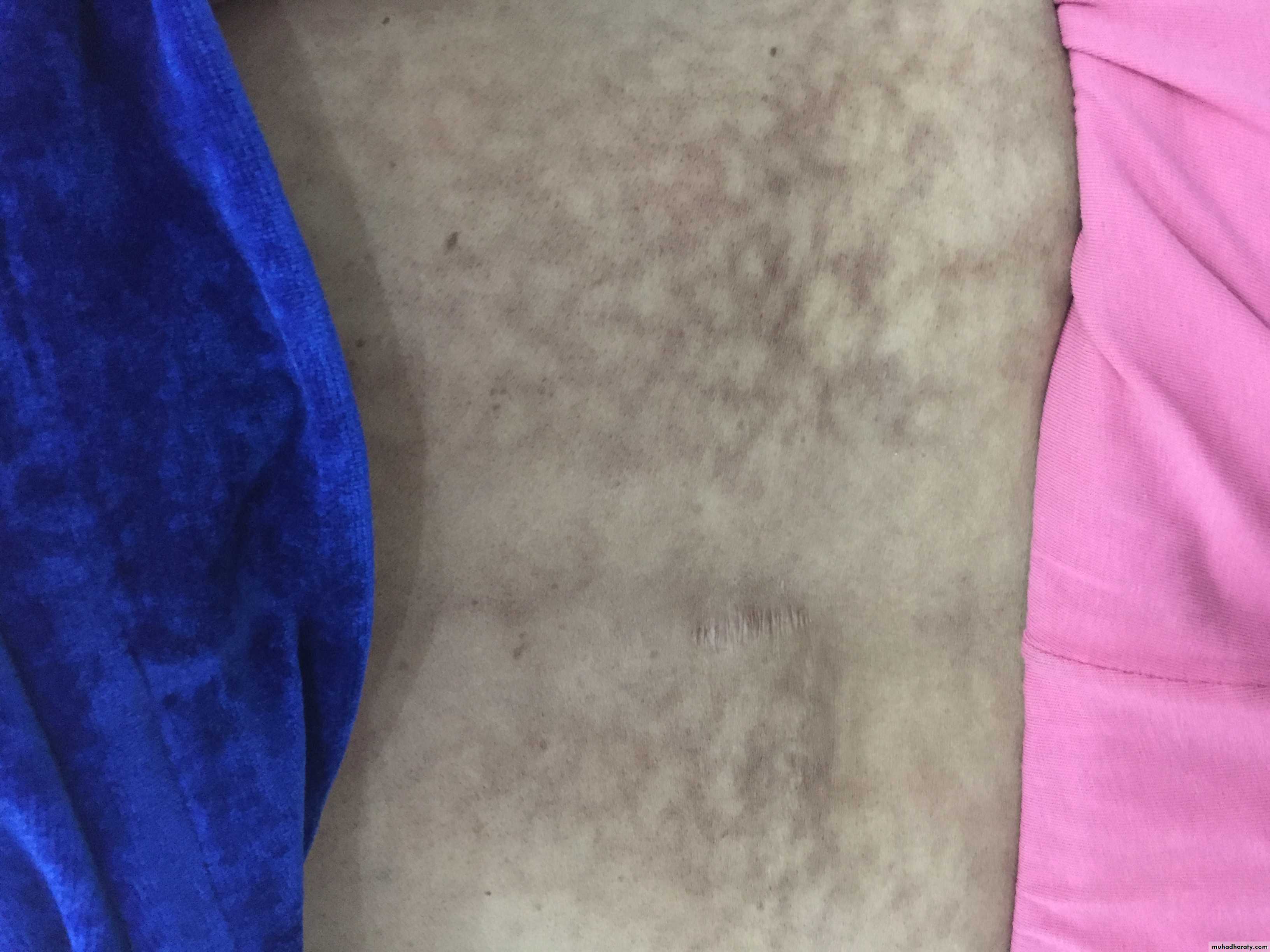
Cold injuries:1- perniosis(=chill blains)
Cold hypersensitivityErythema & swelling (purple pink) of exposed parts
Mainly fingers, toes, nose & ears
Can lead to blistering or ulceration
Pain, itching & burning
Cool to touch, onset enhanced by dampness
IMG_9356.JPG
IMG_9356.JPGtreatment
Protection & prophylaxis of cold Quit smoking
Topical steroids & systemic antihistamines
Nifidipine 20 mg t.d.s., vasodilators (nicotinamide, dipyridamole)
Spontaneous resolution occur in 1-3 weeks
2- frost bite
Frost bite
Cold toxicity due to exposure to extremely low temperaturesFreezing of tissue
Affected part is pale, waxy, painless
Different degrees of tissue damage from erythema to deep gangrene similar to burn
Degree of damage depends on temperature & duration
treatment
Rapid rewarming in hot water bathAnalgesia: counteract thawing pain
Supportive measures:
Bed rest
High protein/calorie diet
Wound care
Avoidance of trauma
Solar injury
The sunlight spectrum is divided intoVisible light 400 to 760 nm, has little biologic activity, except for stimulating the retina
Infrared radiation: above 760 nm, experienced as radiant heat.
Ultraviolet: Below 400 nm spectrum, divided into 3 bands:
1-UVA: 320 to 400 nm
2-UVB: 290 to 320 nm
3-UVC: 200 to 290 nm; Virtually no UVC reaches the earth’s surface, because it is absorbed by the ozone layer
Sun burn
Normal reaction of skin to sunlight in excess of erythema dose
Present as erythema, edema, sometimes blistering on sun exposed skin
Desquamation usually follows within a week
If severe; it may be accompanied by fever, chills, nausea & hypotension
Treatment: analgesics, cool compresses, topical steroids
Erythema, edema, blistering
desquamation
Treatmentcool compresses
photosensitivityAbnormal reaction to normal amount of sunlight; can be either:
1- Chemical photosensitivity: phototoxic & photo allergic photosensitizers
2- Metabolic disorders
3- Light exacerbated disorders
4- Idiopathic photosensitivity
Chemical photosensitivity
Photosensitizers: are substances that may induce an abnormal reaction in skin exposed to sunlight or its equivalent.
These substances may be delivered externally or internally.
Increased sunburn response without prior allergic sensitization is called phototoxicity which may occur from both externally applied phytophotodermatitis or internally administered chemicals phototoxic drug reaction.
While photo allergy needs prior exposure to the substance (sensitization) before inducing the photosensitivity reaction
phytophotodermatitis
Contact between certain plants containing a substance called furocumarine with moist skin & then exposed to long wave ultraviolet light (UVA)A dermatitis develops at the contact site followed by intense pigmentation that can last weeks or months
More common in women & children dealing with citrus fruits, especially on exposed skin (face & hands)
2- metabolic photosensitivity (pellagra & porphyria)
Pellagra: Niacin deficiency 4 D’s disease:1- Dermatitis
2- Diarrhea
3- Dementia
4- Death
porphyria
Defect in heam
synthesis3- light exacerbated disorders(Diseases aggravated by sun light exposure)
These are diseases that are aggravated by exposure to sun light, they are either:1- Genetic disorders: xeroderma pigmentosum
2- Acquired diseases: SLE, Darier’s, vitiligo, acne, small percentage of patients with psoriasis, dermatomyositis, lichen planus actinicus, & chloasma.
4- idiopathic photosensitivity: ple (=polymorphic light eruption)
Called by this name as it has different morphologies in different patients, but a constant morphology in the same patientIt can be papular, vesicular, urticarial or any other type or any combination, but the type is constant for the specific patient
More in young adults, more in females
Mostly erythematous papular rash on sun-exposed skin
A recurrent disease, usually starts in spring & improves in summer
Treatment: 1- Prophylaxis:
Avoid sun exposure especially between 10 am-2 pm.Barrier protection with hats, clothing & umbrellas
Using sunscreen agents which include UV-absorbing chemicals (chemical sunscreens) and UV-scattering or blocking agents (physical sunscreens)
The best sunscreens ideally contain both types with a sun protection factor (SPF) more than 30
2- Medical treatment
1- Topical steroids: usually potent steroids are used
2- Systemic antihistamines: to control itching
3-Systemic steroids: only in severe cases
5- Antimalarial: as chloroquine
6- Light therapy as PUVA or UVB to induce hardening of the skin
7- Immunosuppressant only in recalcitrant cases: azathioprine & cyclosporine
Mechanical trauma
CALLUS: circumscribed hyperkeratosis induced by pressure, diffuse with no central core.CLAVUS: (corn): circumscribed conical thickening with base on surface & apex down pressing on subjacent structures, of 2 types: Soft corns & hard corns