
Plastic surgery
Definition:
is branch of surgery that is concerned
with remold, repair and restore body parts especially
by transfer of tissue.
Plastic as word came from Greek word
plastikos
which mean remold or reform.
Plastic as adjective mean capable of being shaped or
formed.
History:
•
India:
Susrutha.
first one used skin graft.
at 8
th
B.C
• Europe:
Heinrich.
At 15
th
century.
• America:
Dr John Peter.
at 1827 first cleft
palate repair.
•
Newzeland:
Sir Harold Gillies.

Aesthetic or cosmetic
surgery:
which performed to reshape normal
structure of body to improve the
patient appearance.
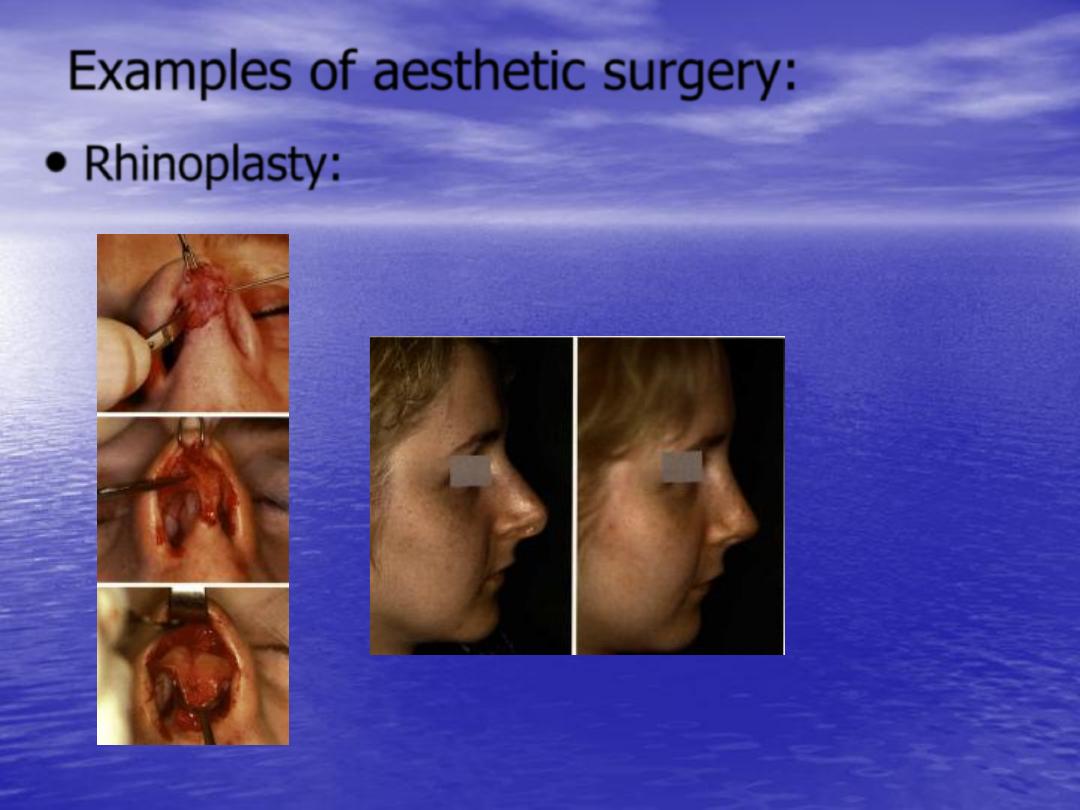
Examples of aesthetic surgery:
•
Rhinoplasty:

•
Abdominoplasty:

• facelift:
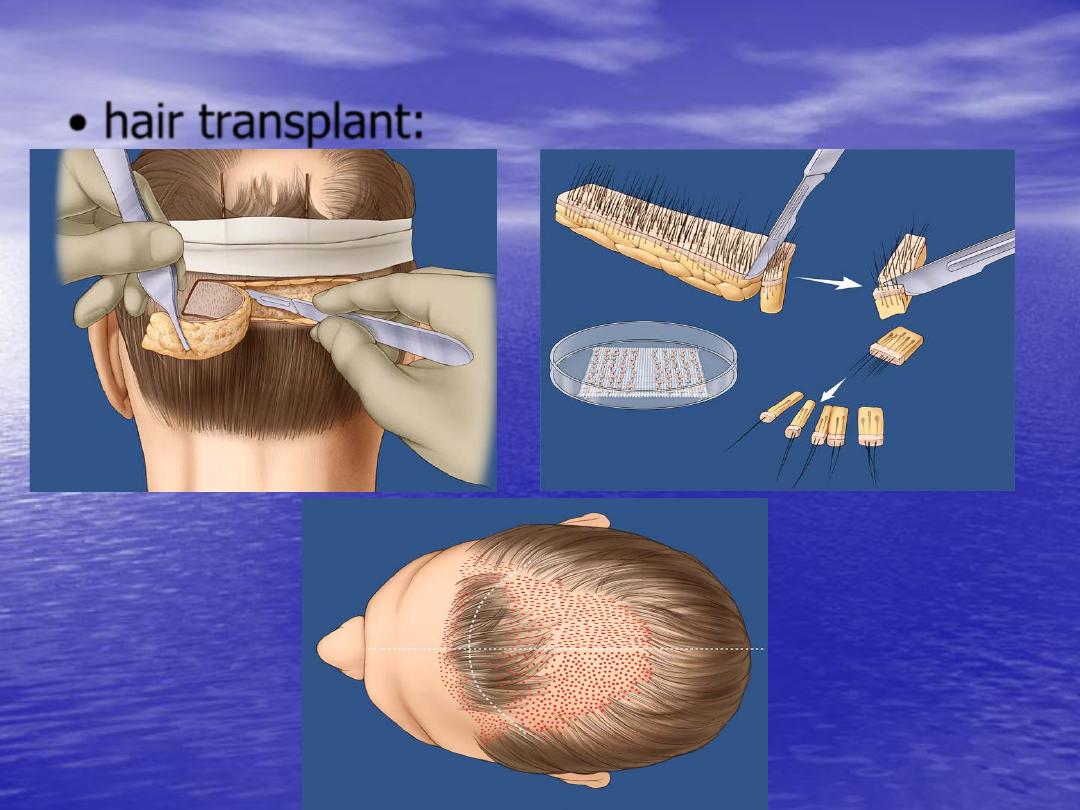
• hair transplant:


Reconstructive surgery:
•
which is done for these who have
congenital deformities e.g. cleft lip and
palate, or those who have acquired
deformities as result of, infection,
accident, burn.
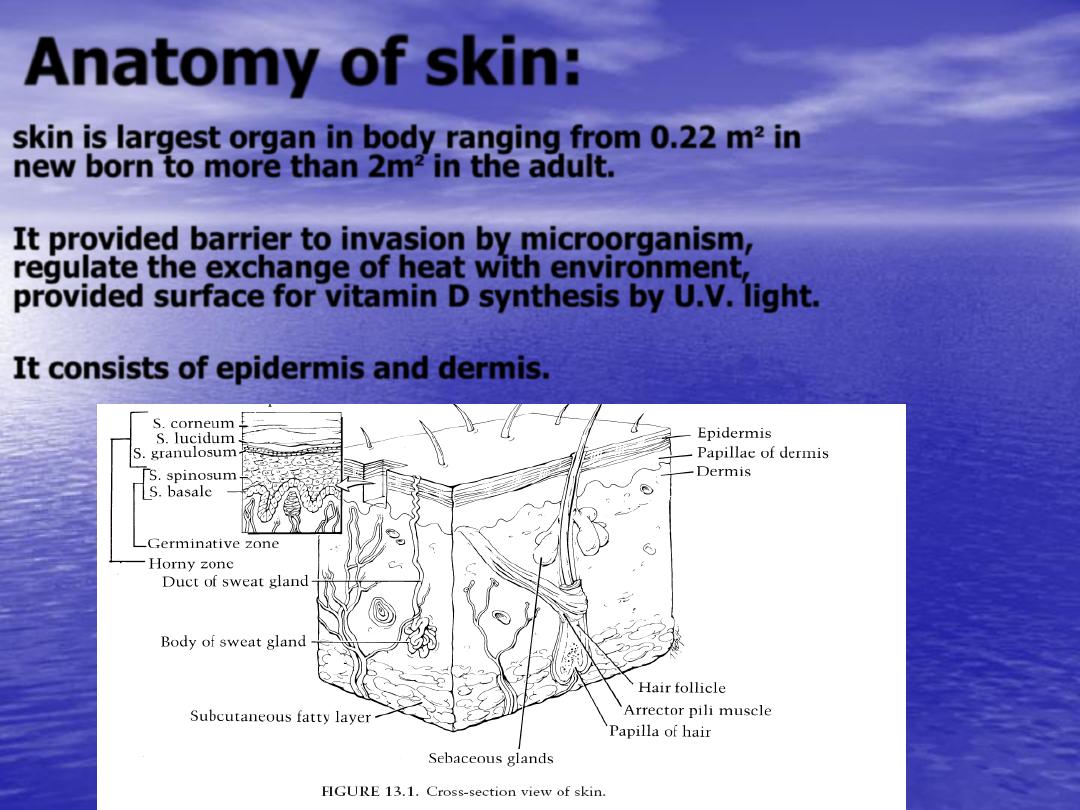
Anatomy of skin:
skin is largest organ in body ranging from
0.22 m²
in
new born to more than
2m²
in the adult.
It provided barrier to invasion by microorganism,
regulate the exchange of heat with environment,
provided surface for vitamin D synthesis by U.V. light.
It consists of
epidermis
and
dermis.
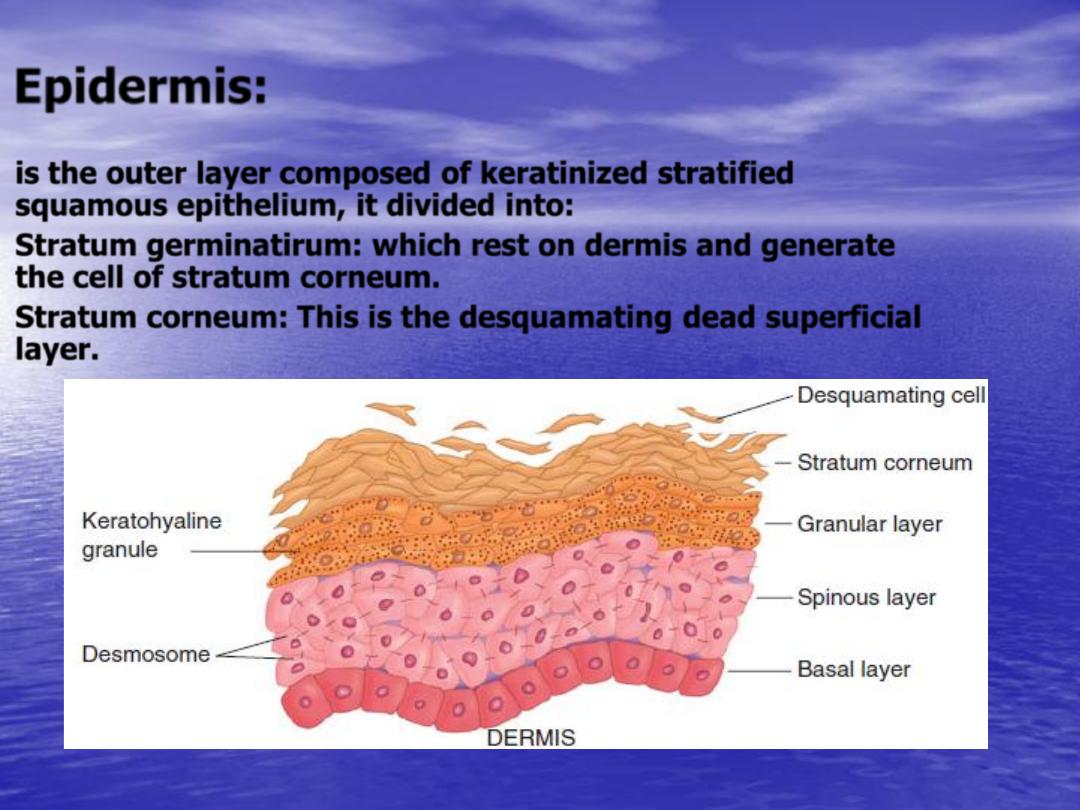
Epidermis:
•
is the outer layer composed of keratinized stratified
squamous epithelium, it divided into:
•
Stratum germinatirum:
which rest on dermis and generate
the cell of stratum corneum.
•
Stratum corneum:
This is the desquamating dead superficial
layer.
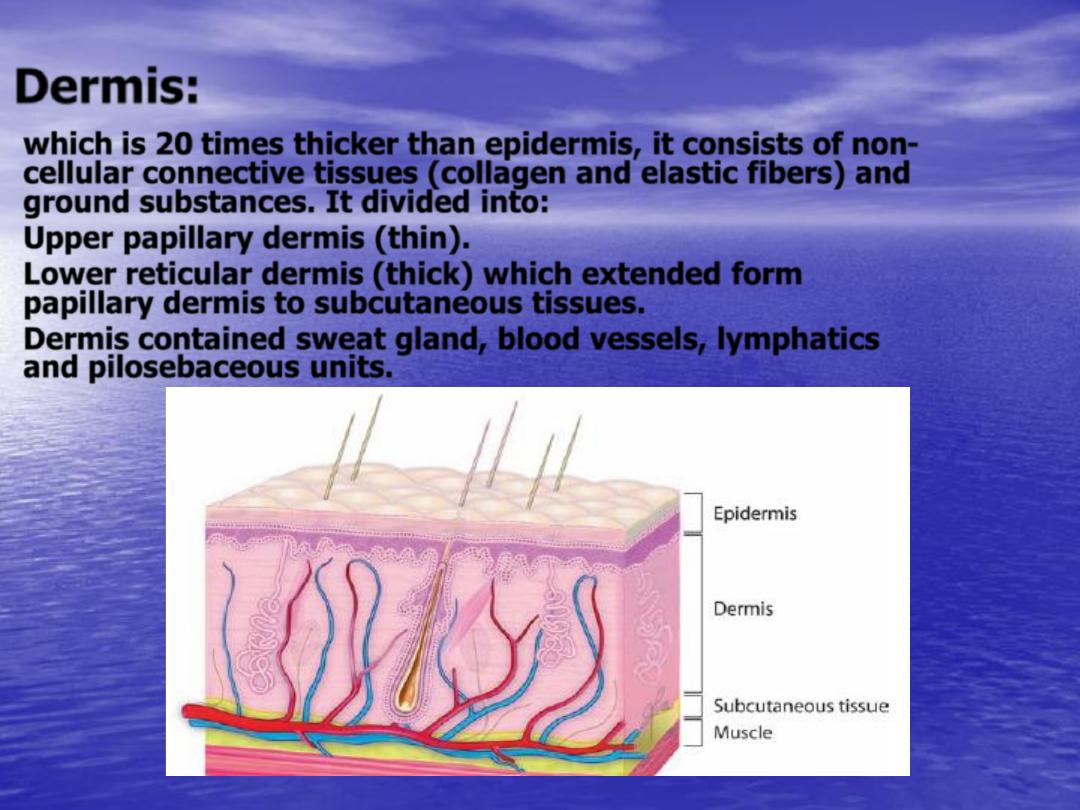
Dermis:
•
which is
20
times thicker than epidermis, it consists of non-
cellular connective tissues (collagen and elastic fibers) and
ground substances. It divided into:
•
Upper papillary dermis
(thin).
•
Lower reticular dermis
(thick) which extended form
papillary dermis to subcutaneous tissues.
•
Dermis contained sweat gland, blood vessels, lymphatics
and pilosebaceous units.
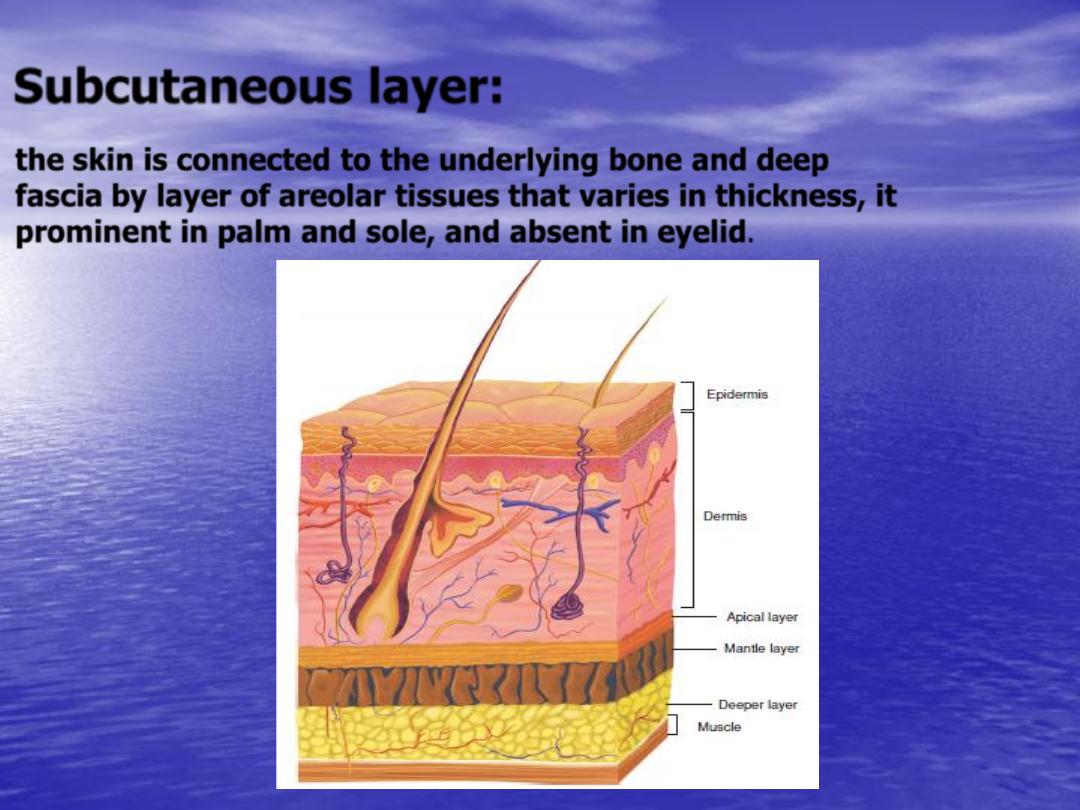
Subcutaneous layer:
•
the skin is connected to the underlying bone and deep
fascia by layer of areolar tissues that varies in thickness, it
prominent in palm and sole, and absent in eyelid.
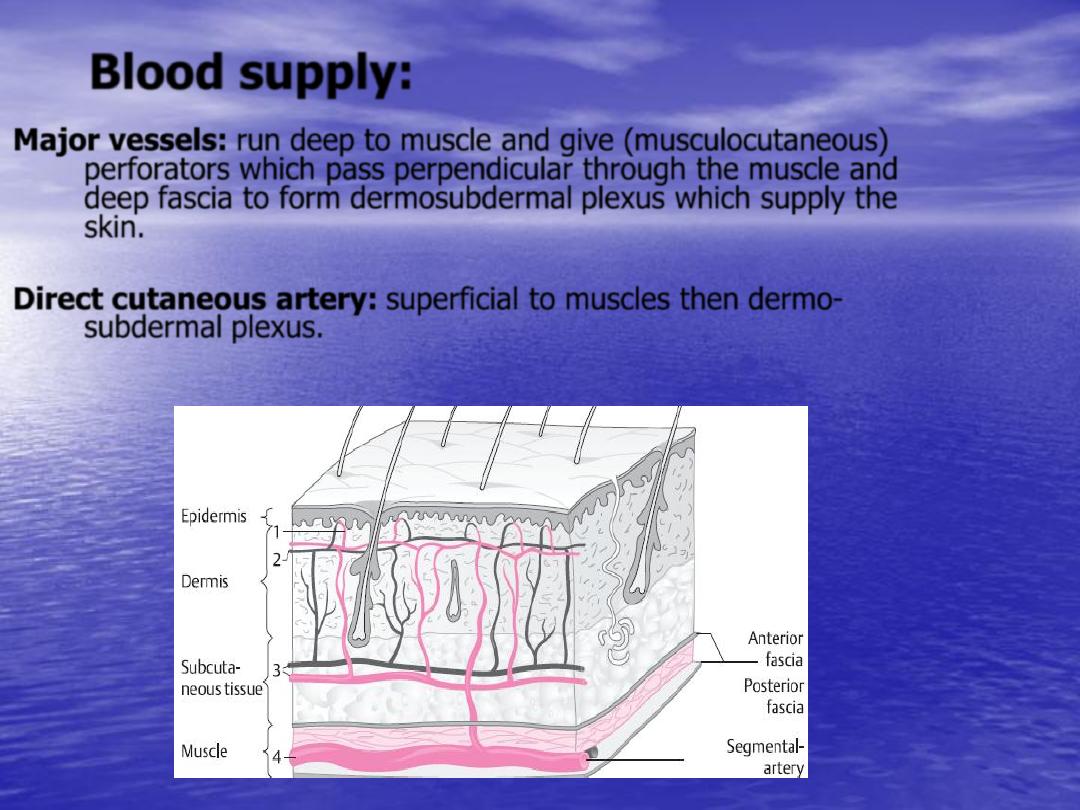
Blood supply:
Major vessels:
run
deep to muscle and give (musculocutaneous)
perforators which pass perpendicular through the muscle and
deep fascia to form dermosubdermal plexus which supply the
skin.
Direct cutaneous artery:
superficial to muscles then dermo-
subdermal plexus.
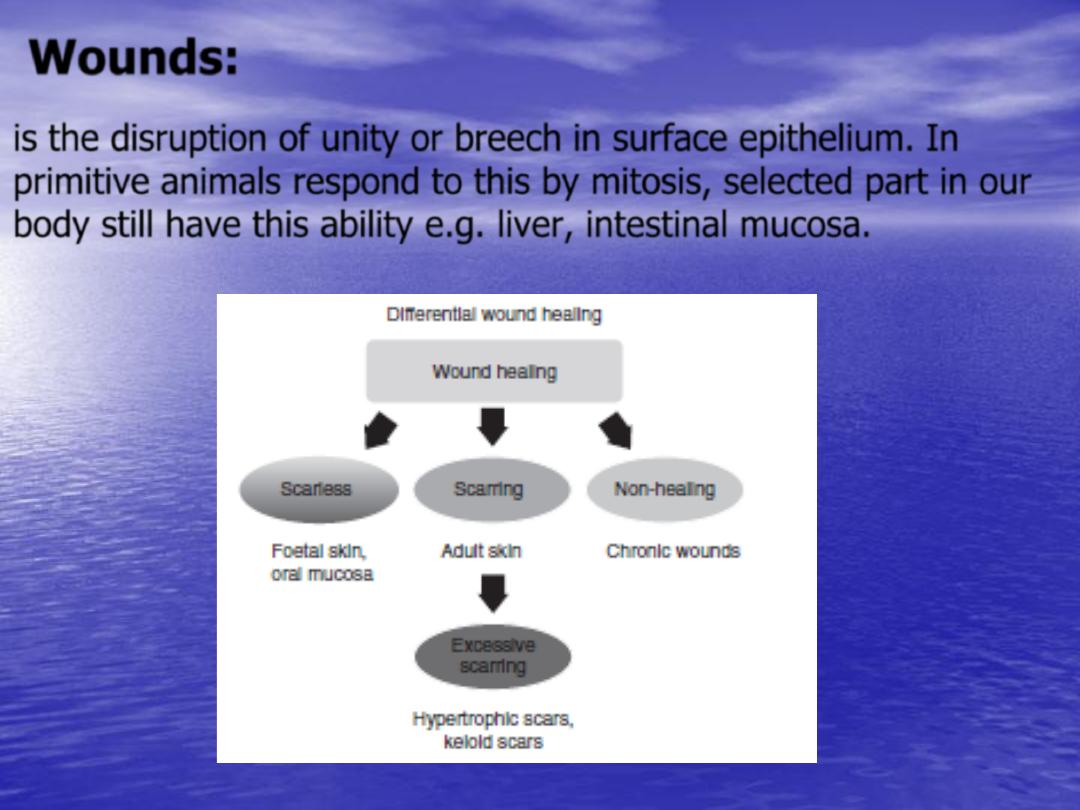
Wounds:
is the disruption of unity or breech in surface epithelium. In
primitive animals respond to this by mitosis, selected part in our
body still have this ability e.g. liver, intestinal mucosa.
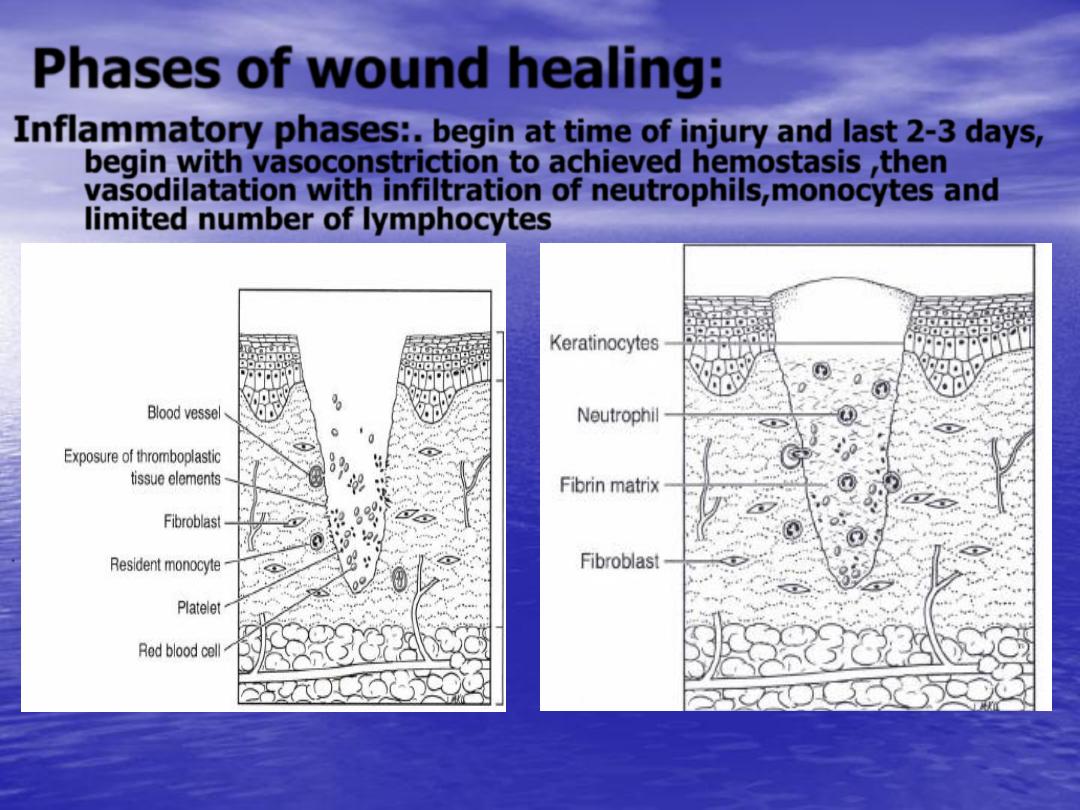
Phases of wound healing:
Inflammatory phases:
.
begin at time of injury and last
2-3
days,
begin with vasoconstriction to achieved hemostasis ,then
vasodilatation with infiltration of neutrophils,monocytes and
limited number of lymphocytes
.
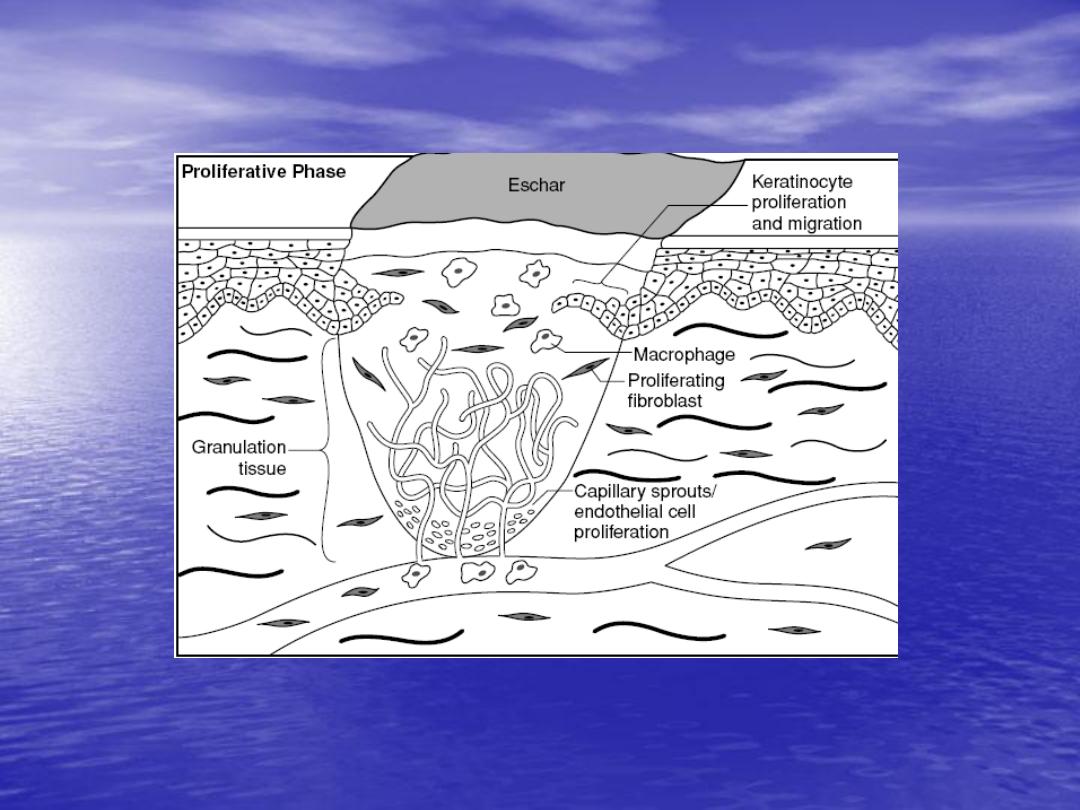
Proliferative phase:
begin around day
3
and
last through week during which collagen
synthesis and epithelization occur.
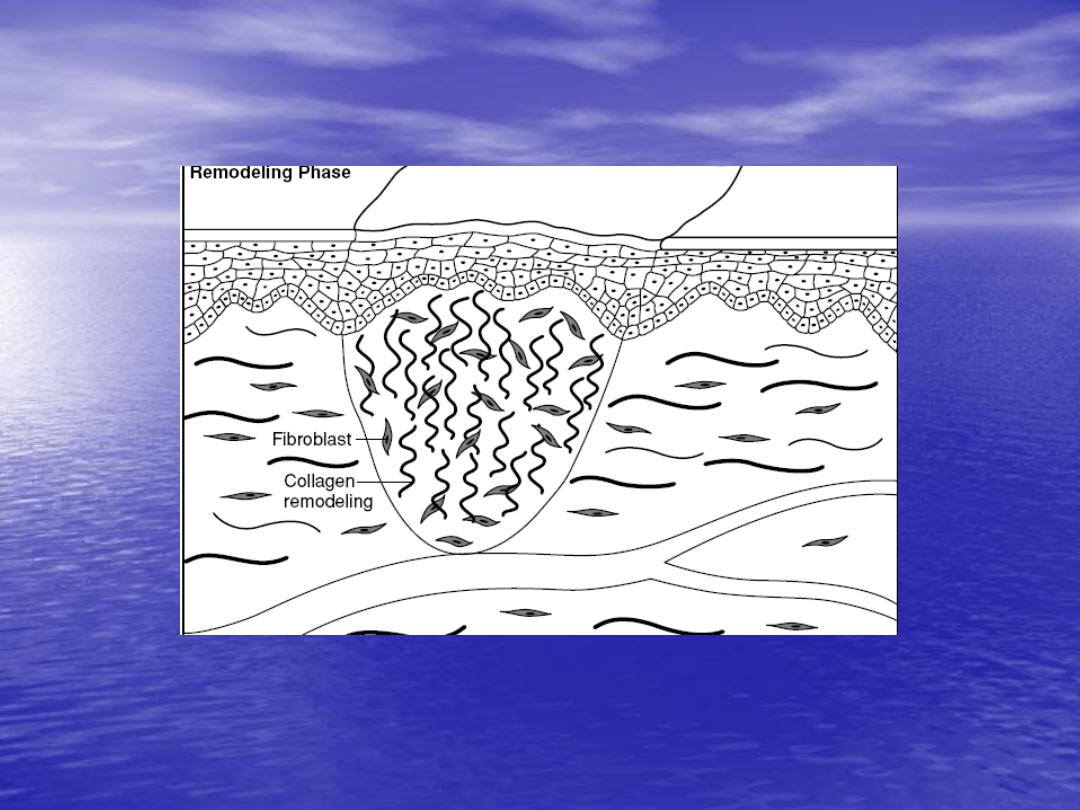
Remolding phase:
during which increase
in collagen production and breakdown, continuous
for
6 month-1 year
. Wound strength increase as
collagen reorganized and vascularity decrease

Sequel of wound healing:
scaring
Hypertrophic scar
keloid
Chronic wound
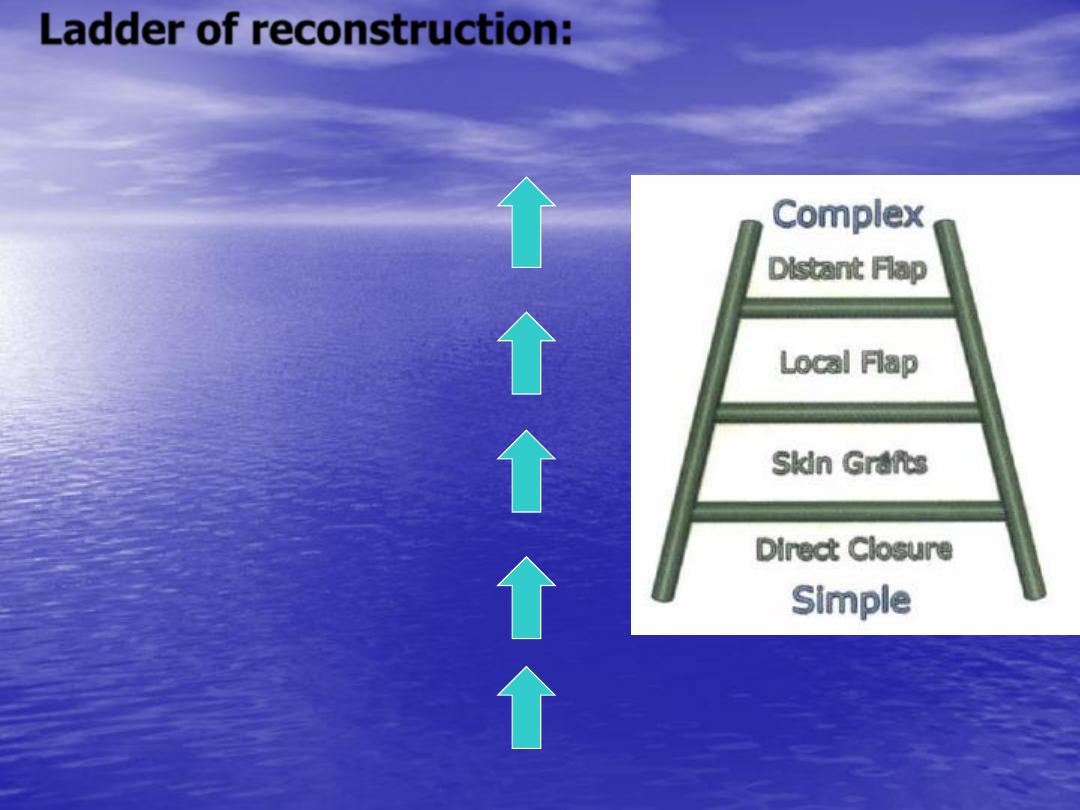
Ladder of reconstruction:
By secondary intention
direct
closure
skin graft
local flap
distance
flap
free flap.
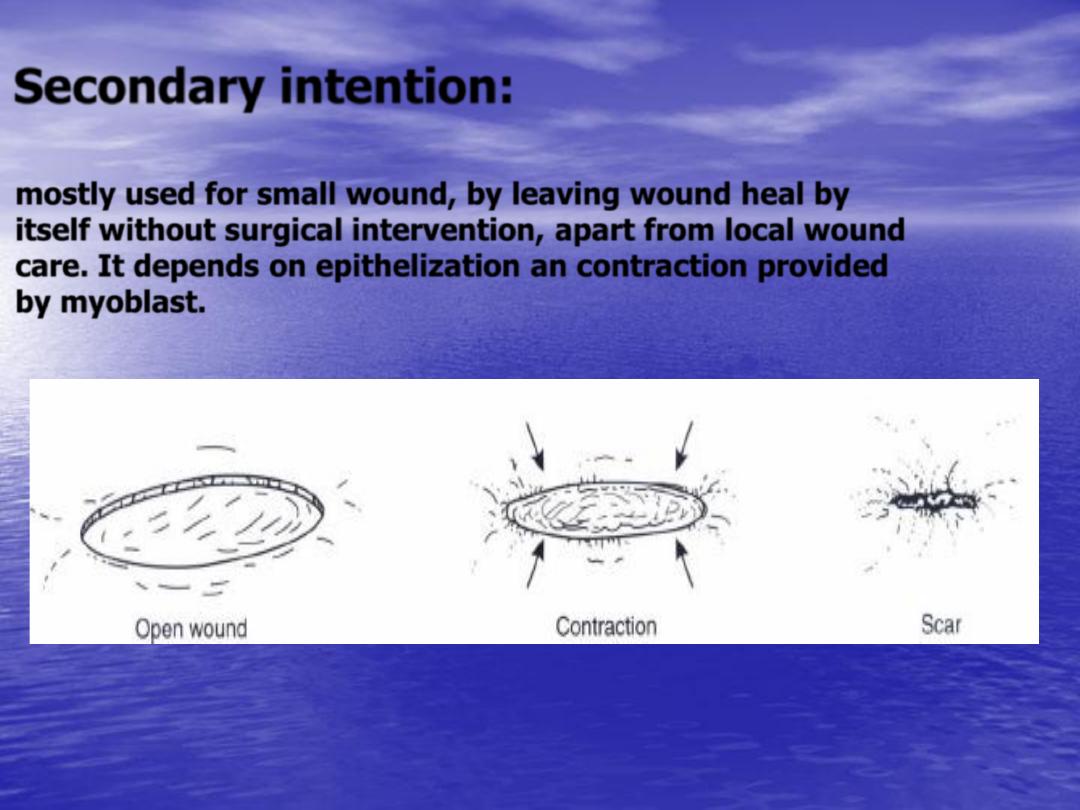
Secondary intention:
•
mostly used for small wound, by leaving wound heal by
itself without surgical intervention, apart from local wound
care. It depends on epithelization an contraction provided
by myoblast.

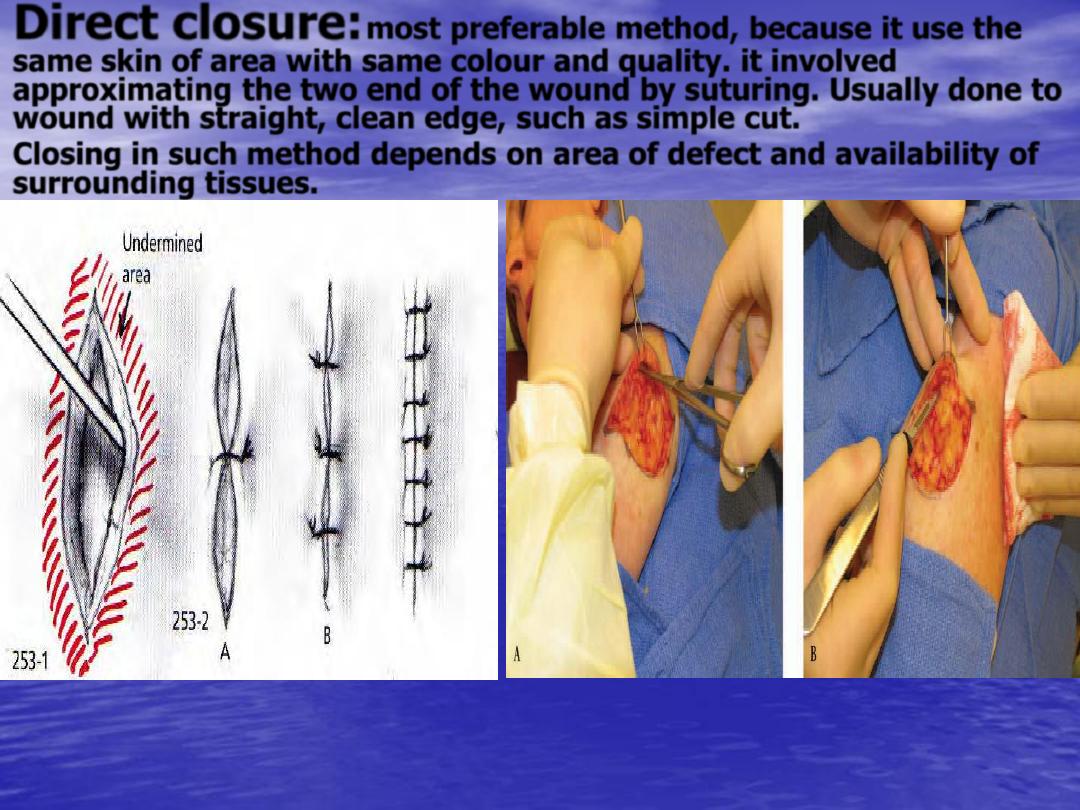
Direct closure:
most preferable method, because it use the
same skin of area with same colour and quality. it involved
approximating the two end of the wound by suturing. Usually done to
wound with straight, clean edge, such as simple cut.
Closing in such method depends on area of defect and availability of
surrounding tissues.
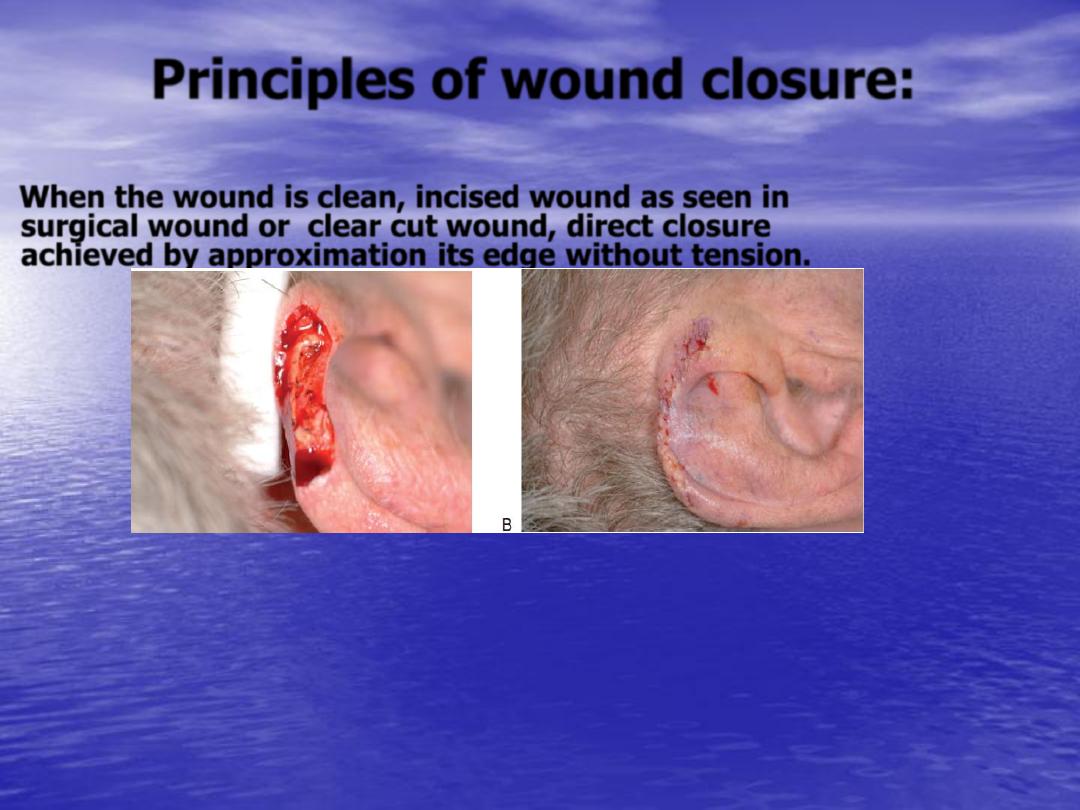
Principles of wound closure:
When the wound is clean, incised wound as seen in
surgical wound or clear cut wound, direct closure
achieved by approximation its edge without tension.
When handling the tissues during closure we should avoiding
excessive retraction and pressure on wound, irrigation
and moist pack should be used to prevent wound
desiccation.
•
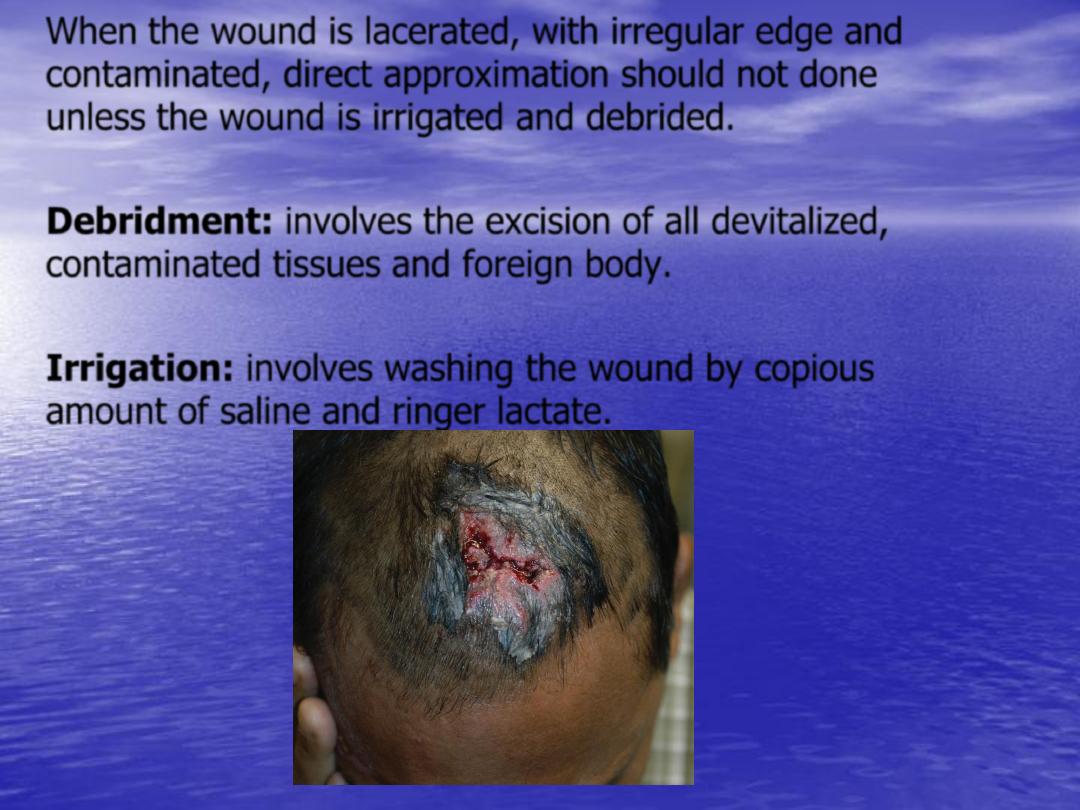
When the wound is lacerated, with irregular edge and
contaminated, direct approximation should not done
unless the wound is irrigated and debrided.
•
Debridment:
involves the excision of all devitalized,
contaminated tissues and foreign body.
•
Irrigation:
involves washing the wound by copious
amount of saline and ringer lactate.
Method of debridment:
•
Mechanical:
This involved sharp or blunt
excision of dead tissues.
•
Gauze:
repetitive application of moistened
gauze which desiccates and gradually removed
necrotic debris from the wound.
•
Chemical:
topical enzyme application which
digests devitalized tissues

Aseptic technique:
by strict using aseptic measurement such
as hand scrubbing, using of sterile instrument, and
clean operative site, and hair shaving.
Hemostasis:
as bleeding can cause ischemia and hematoma
formation which can lead to infection which affect
normal wound healing.hemostasis can achieved by:
-Topical application of adrenaline.
-Electrocautery.
-Large vessels can be clamped or suture.
-Topical hemostatic e.g. fibrin glue.
Antibiotics:
Most soft tissues infection caused by gram (+)
organism e.g. (staph., strept.).Usually we begin with
broad spectrum antibiotics such as cephalosporin, and
more specific therapy directed by bacterial culture and
sensivity.
Indications of antibiotics:
– Acute wound with surrounding cellulitis with
gross contaminated.
– Human or animal bit.
– Immunosuppressed or diabetic patient.
– Vulvular heart disease to prevent
endocarditis.
•
Closure methods:
•
Simple interrupted suture.
•
Horizontal and vertical mattress.
•
Subcuticular continuous suture.
•
Continuous running suture.

Simple interrupted suture
Horizontal and vertical mattress
Subcuticular continuous suture
Continuous running suture
Closure materials:
•
Suture materials:
This divided to natural and
synthetic materials or to absorbable or non-
absorbable.
•
Staples:
which more rapid than sutures and
create minimum reaction.
•
Surgical tapes:
either alone or with other
suture materials e.g. steri-strip.
•
Biological or synthetic materials
e.g.
Cynoacrylate.
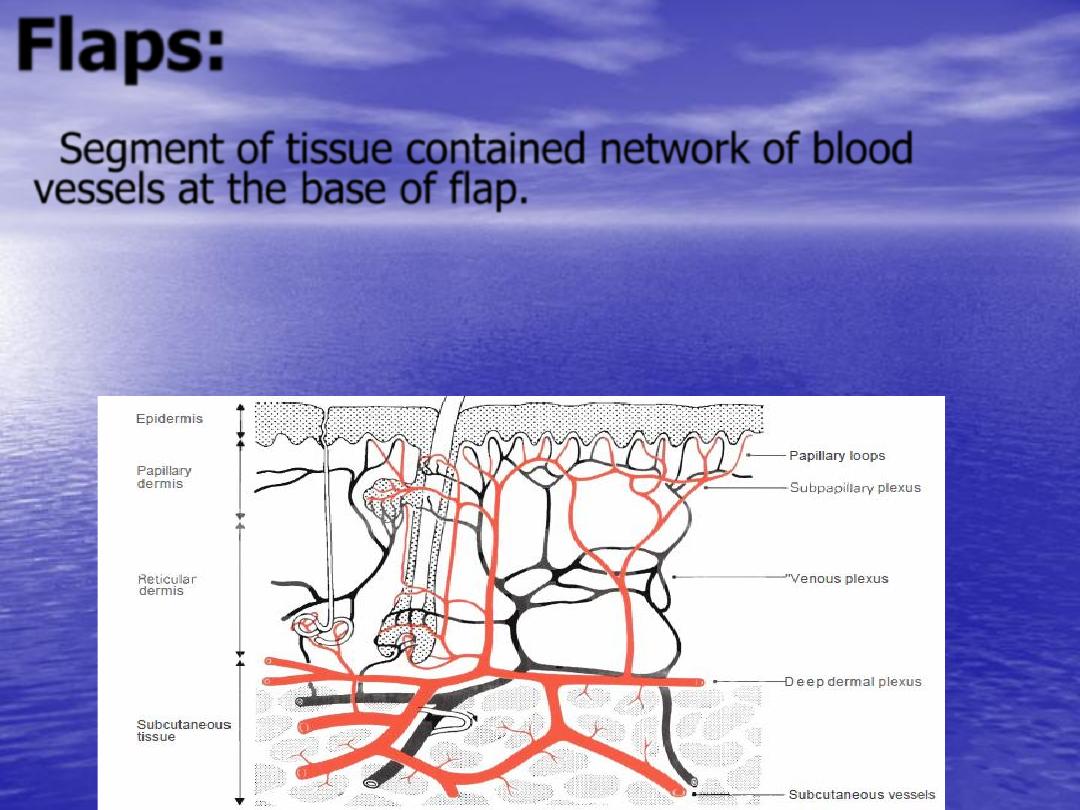
Flaps:
Segment of tissue contained network of blood
vessels at the base of flap.
Historically the word
flap
originated from the 16
th
century Dutch word '
flappe
' - this being anything
that hung broad and loose, fastened only by one
side.
Indication of flap:
1-Wound with poor vascularity.
2-Full thickness defect of ear, check,nose.
3-Padding of body prominence e.g. patient with bed
sore.
4-Muscle flap as motor unit.
5-Control of infection since have good blood supply.
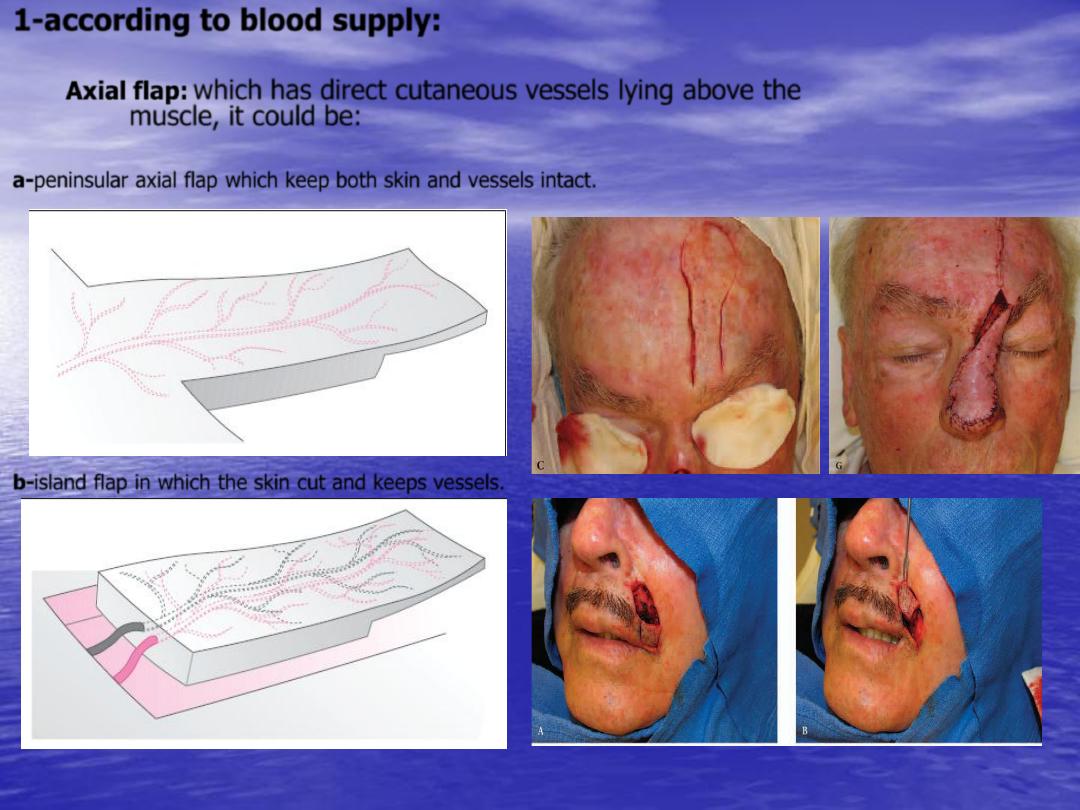
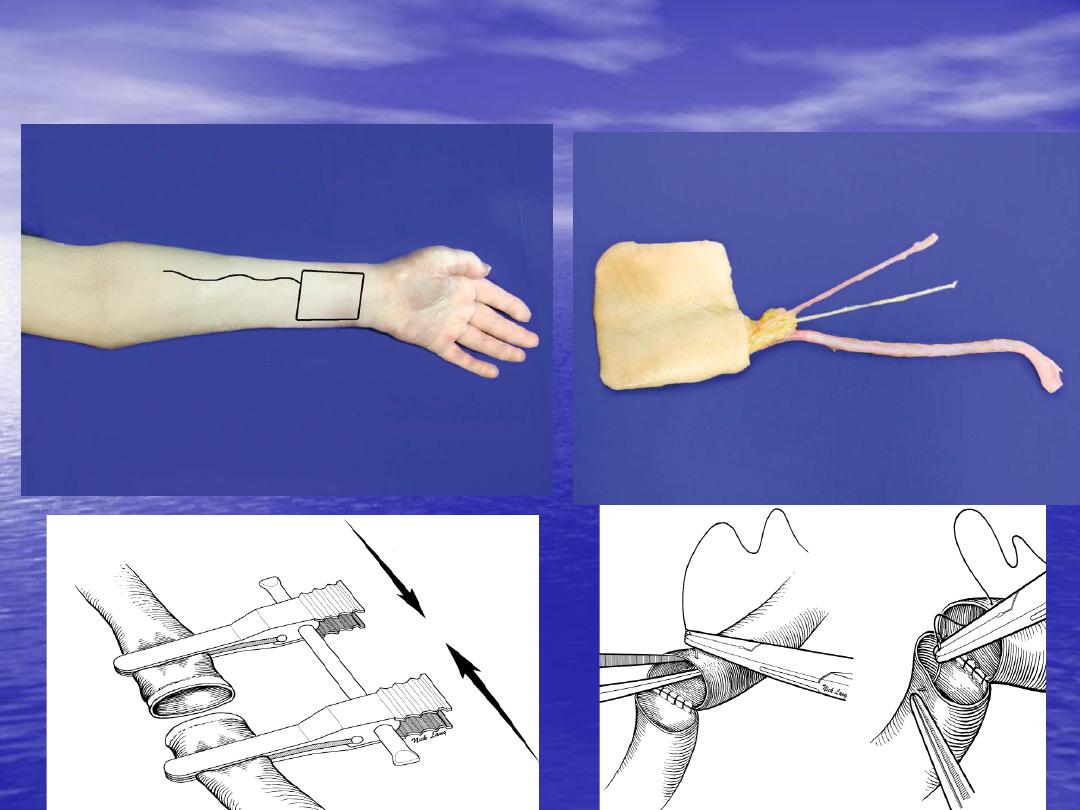
1-according to blood supply:
Axial flap:
which has direct cutaneous vessels lying above the
muscle, it could be:
a-peninsular axial flap which keep both skin and vessels intact.
b-island flap in which the skin cut and keeps vessels.
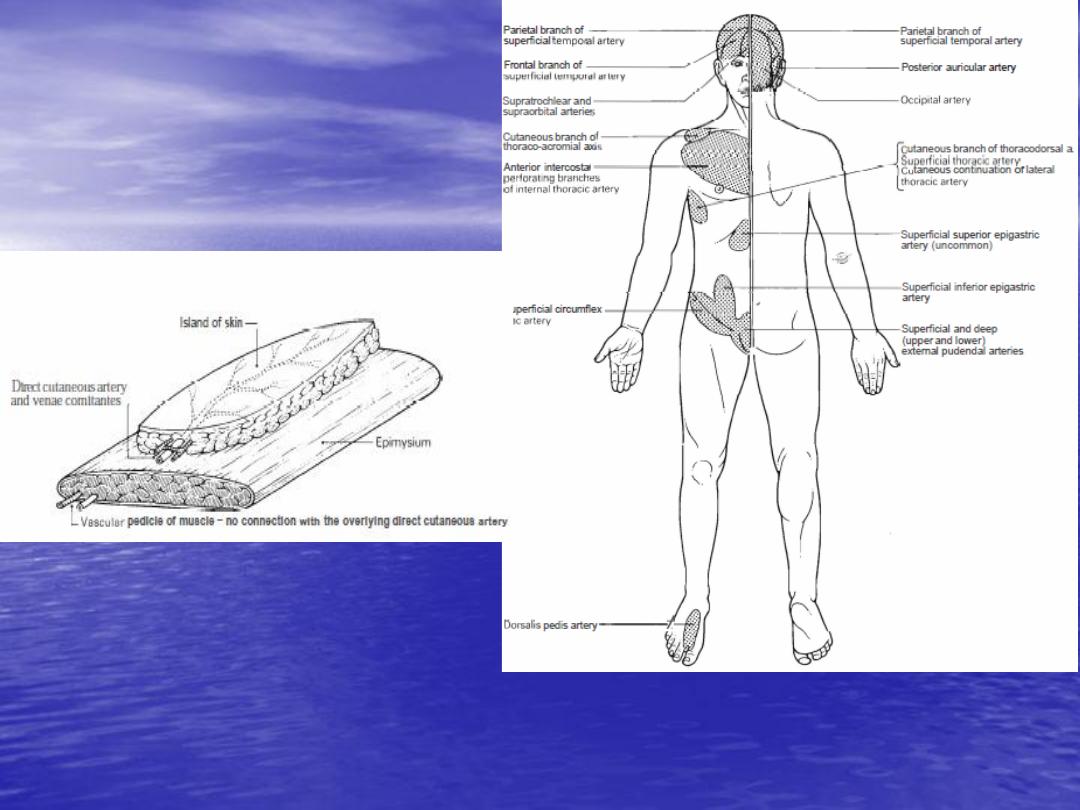
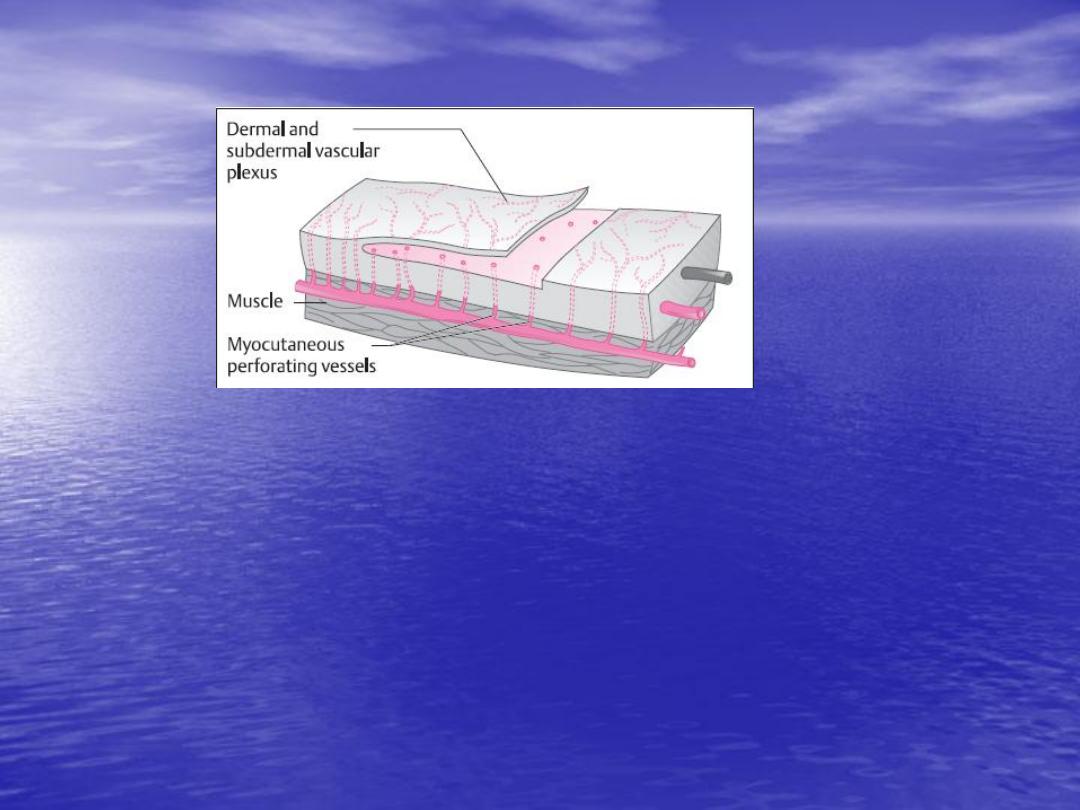
Random flap:
which depend on musculocutaneous
artery pass deep to the muscle and send perforator to
base of flap
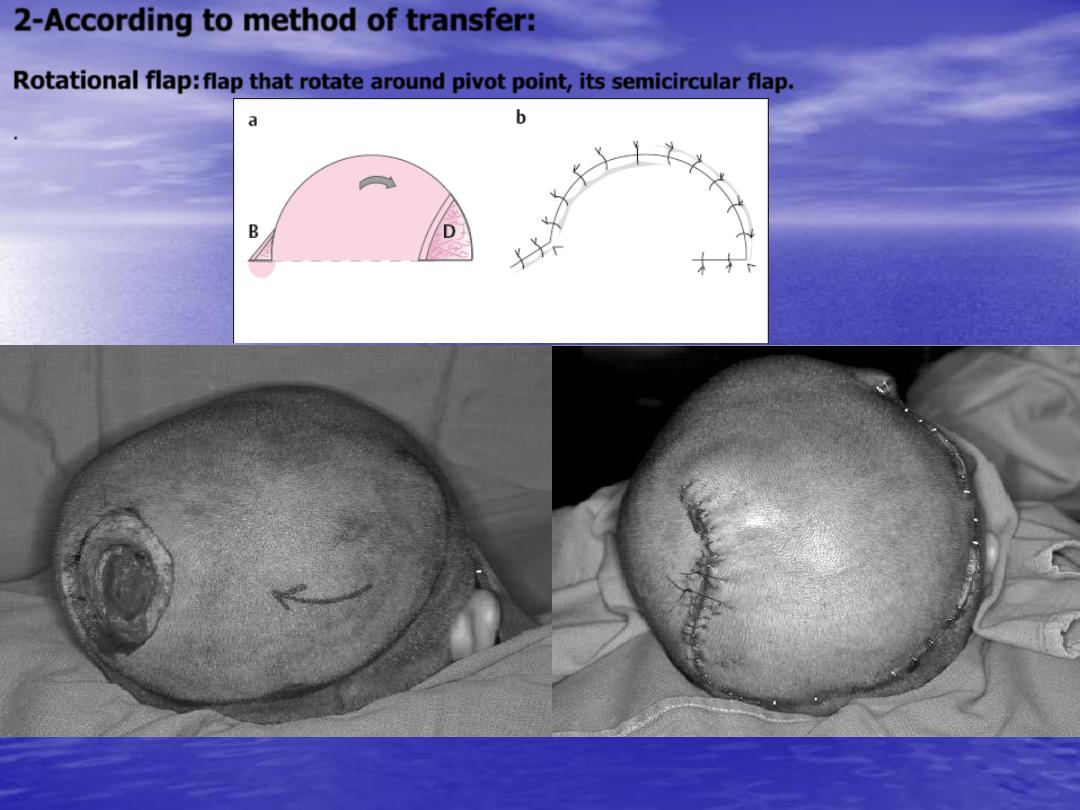
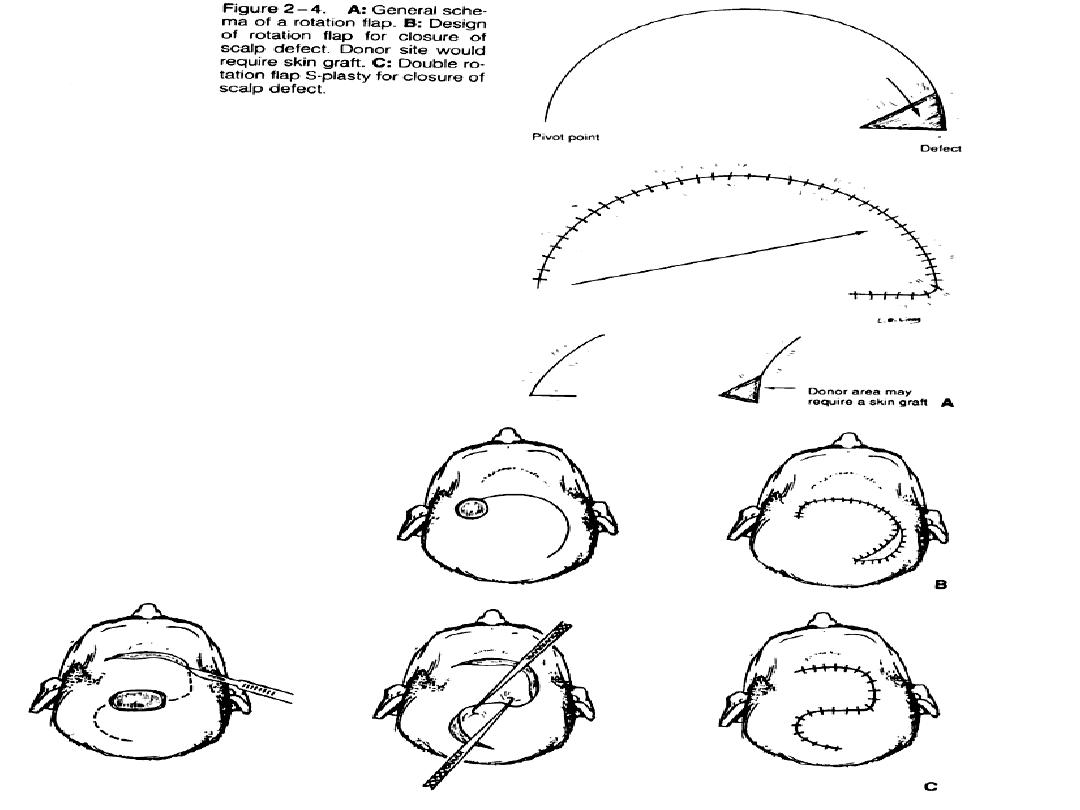
2-According to method of transfer:
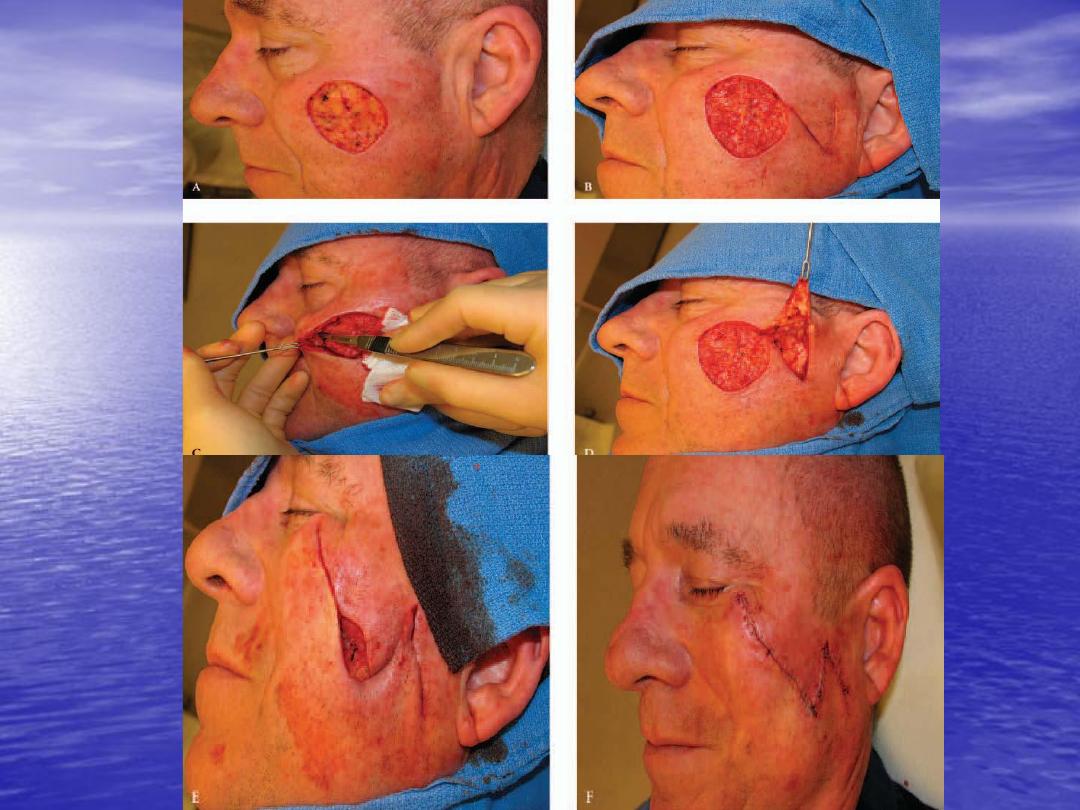
Rotational flap:
flap that rotate around pivot point, its semicircular flap.
.

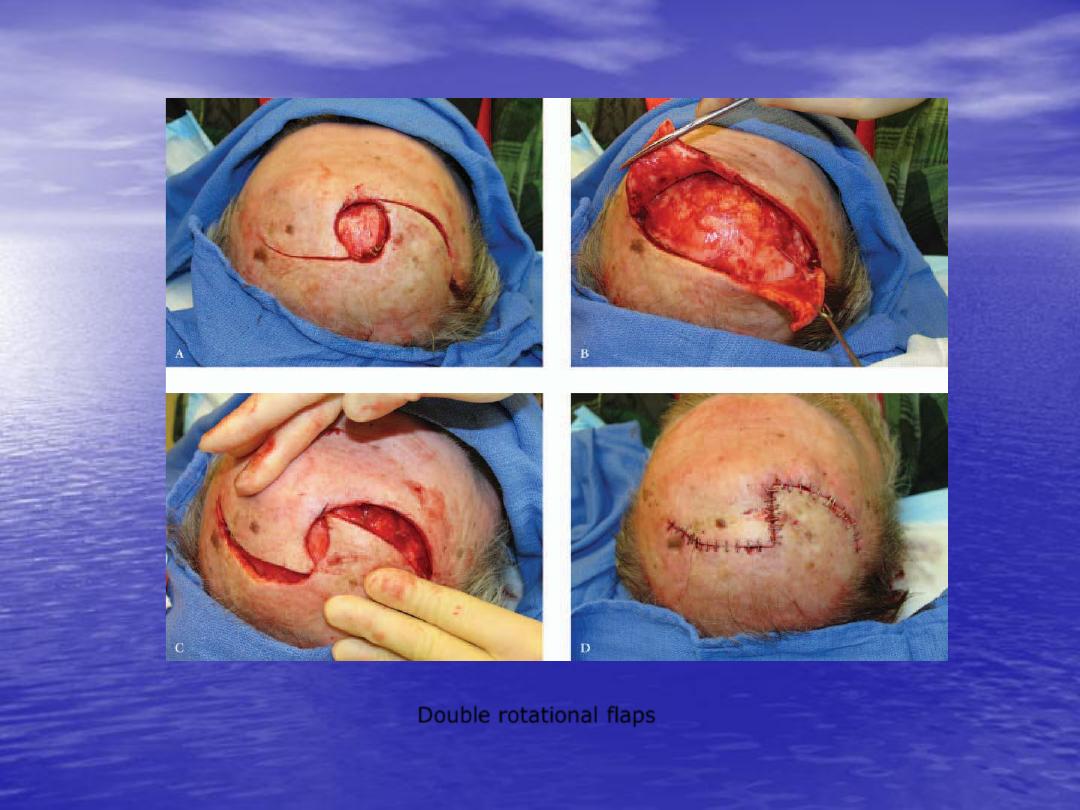
Double rotational flaps
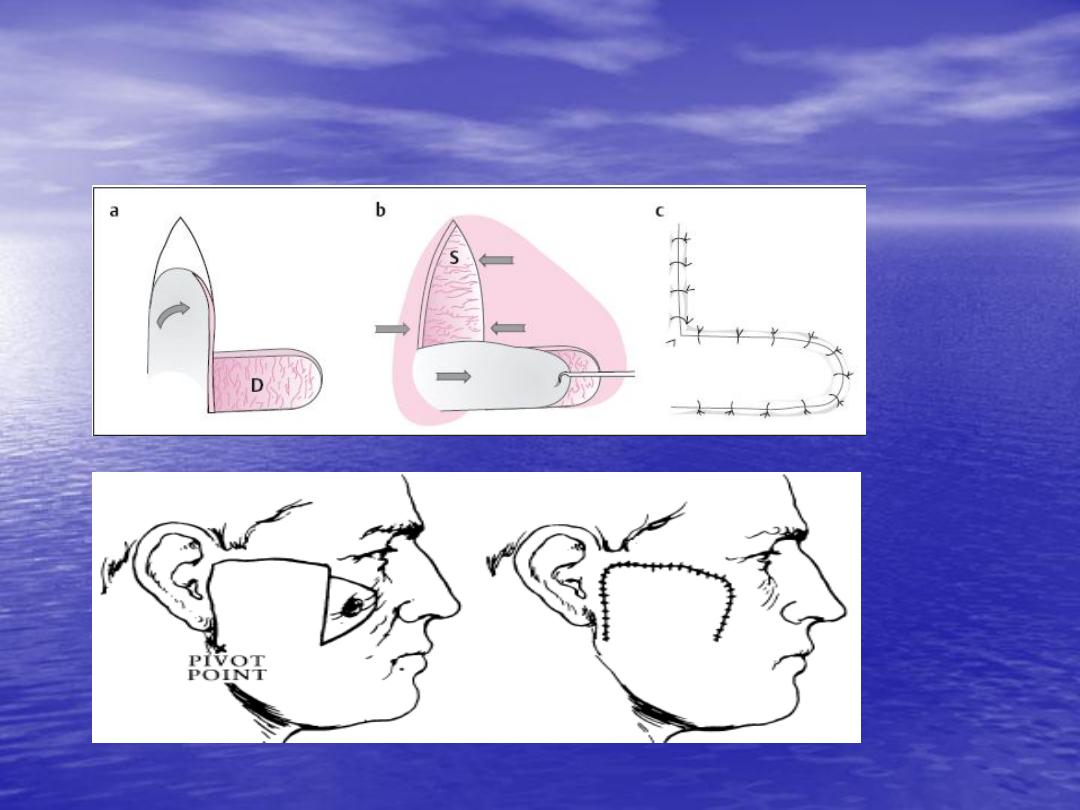
Transposition flap:
rectangular flap that rotate on
pivot point, the donor site can be either closed
directly or if not possible covered by skin
graft.
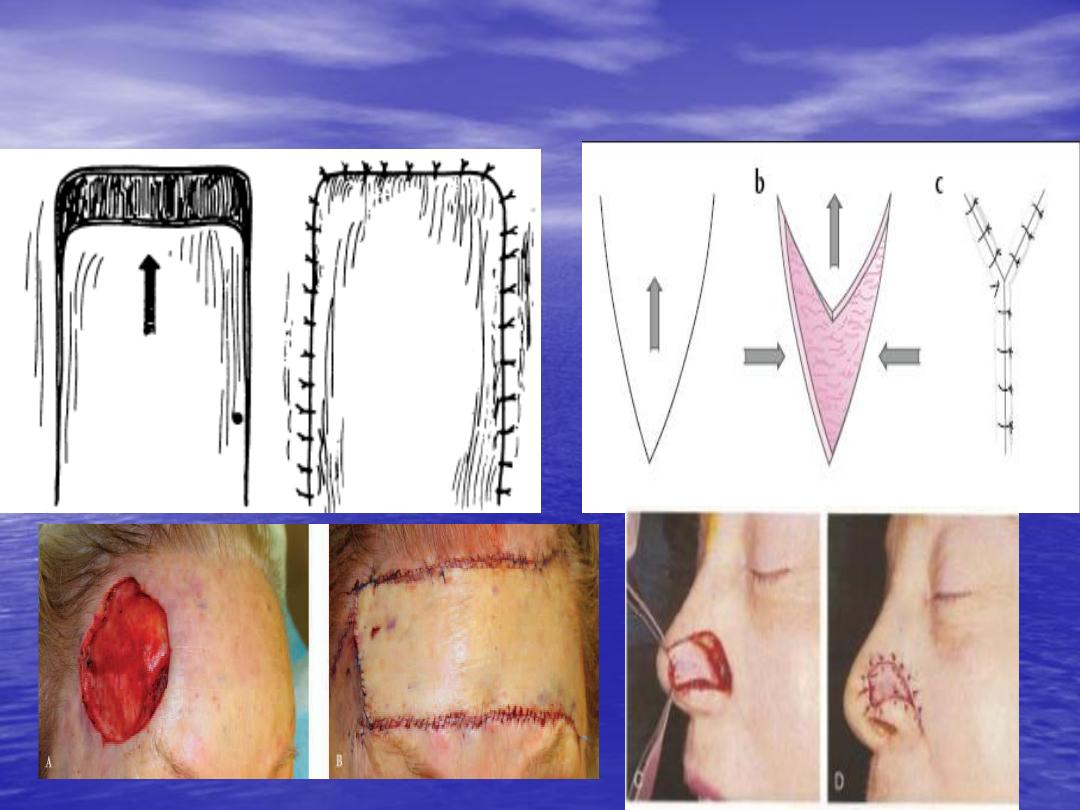
Advancement flap:
it moved primarily in straight
line from donor site to recipient site. There are
various advancement flap like single pedicle
advancement flap, bipedicle advancement flap
and V-Y advancement flap.
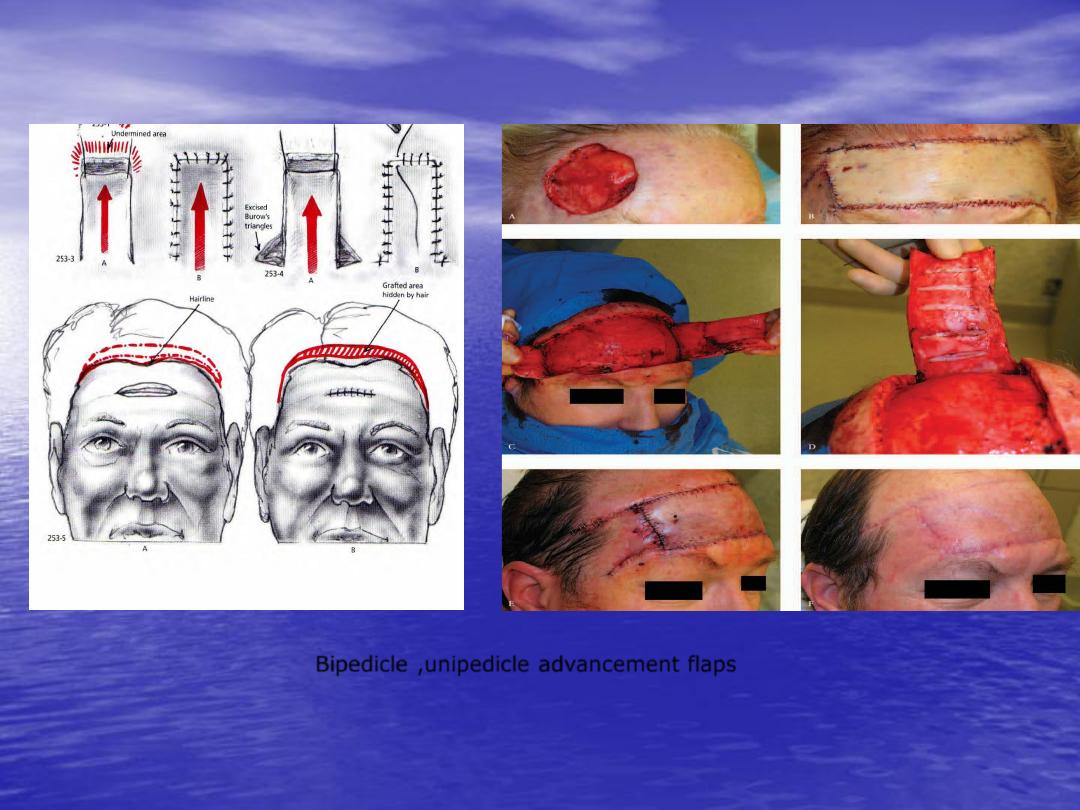
Bipedicle ,unipedicle advancement flaps
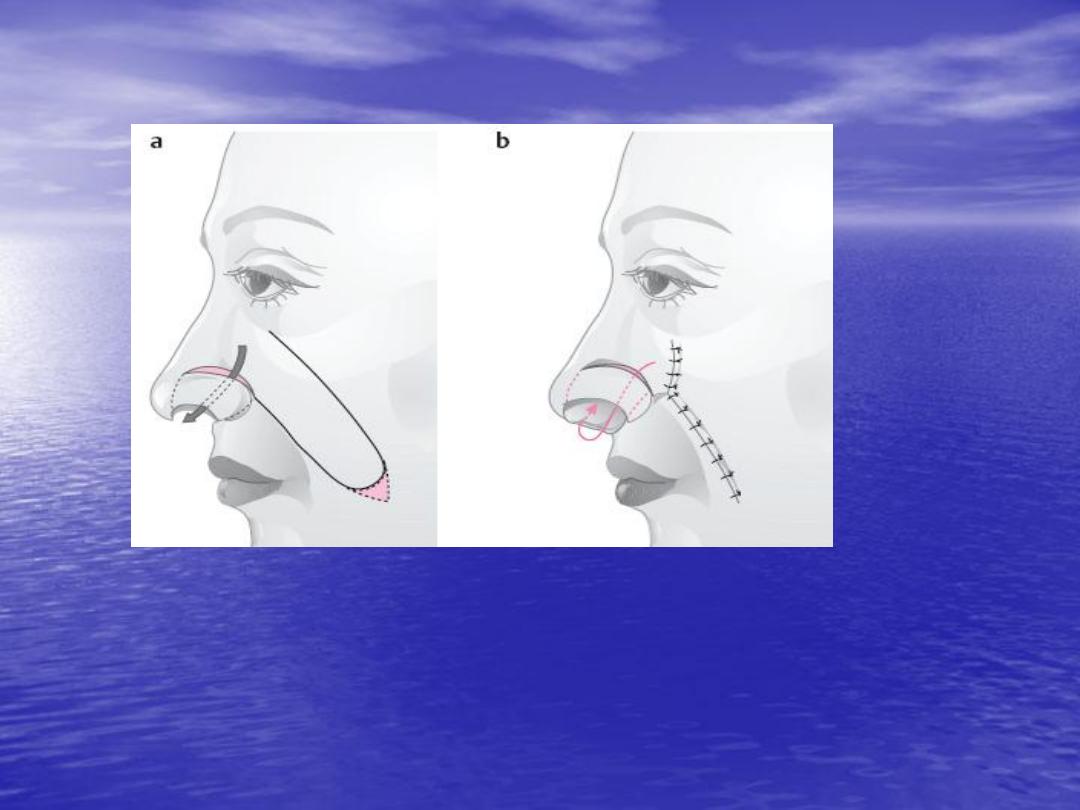
Interpolation flap:
in which the donor site is
separated from recipient site by pedicle of
flap, so should pass above or beneath tissue to
reach the recipient area


3-According to its contents:
Cutaneous
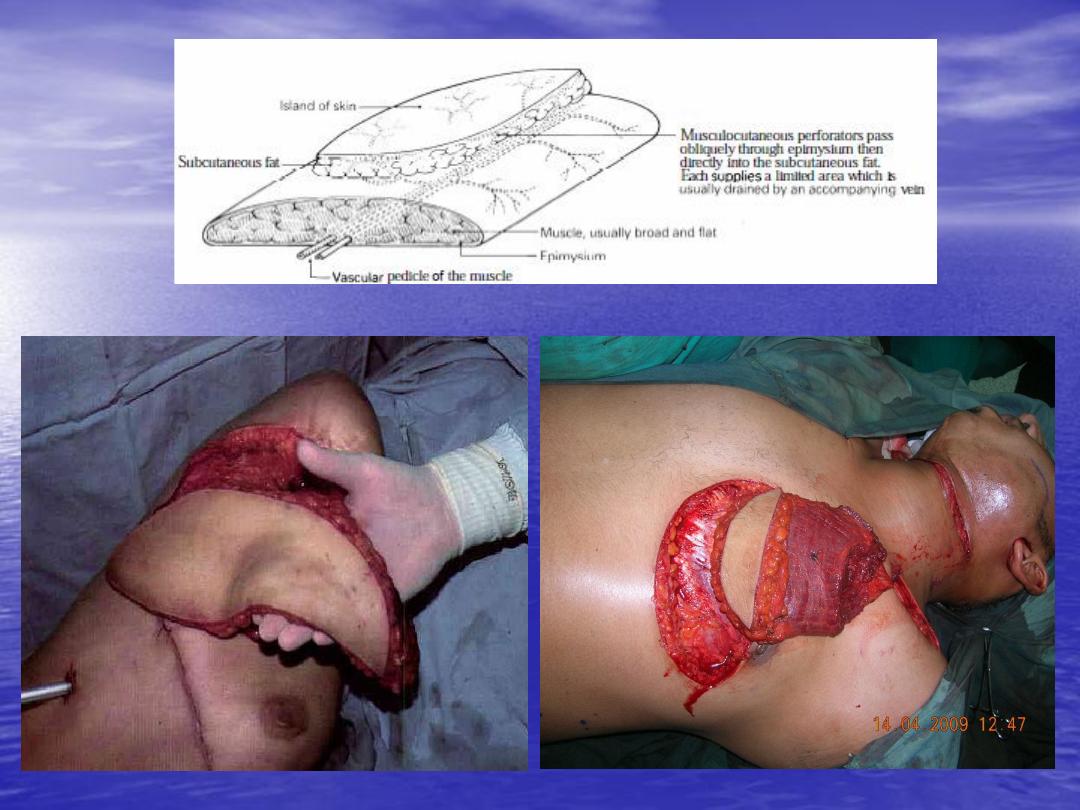
Musculocutaneous
Osteomusculocutaneous
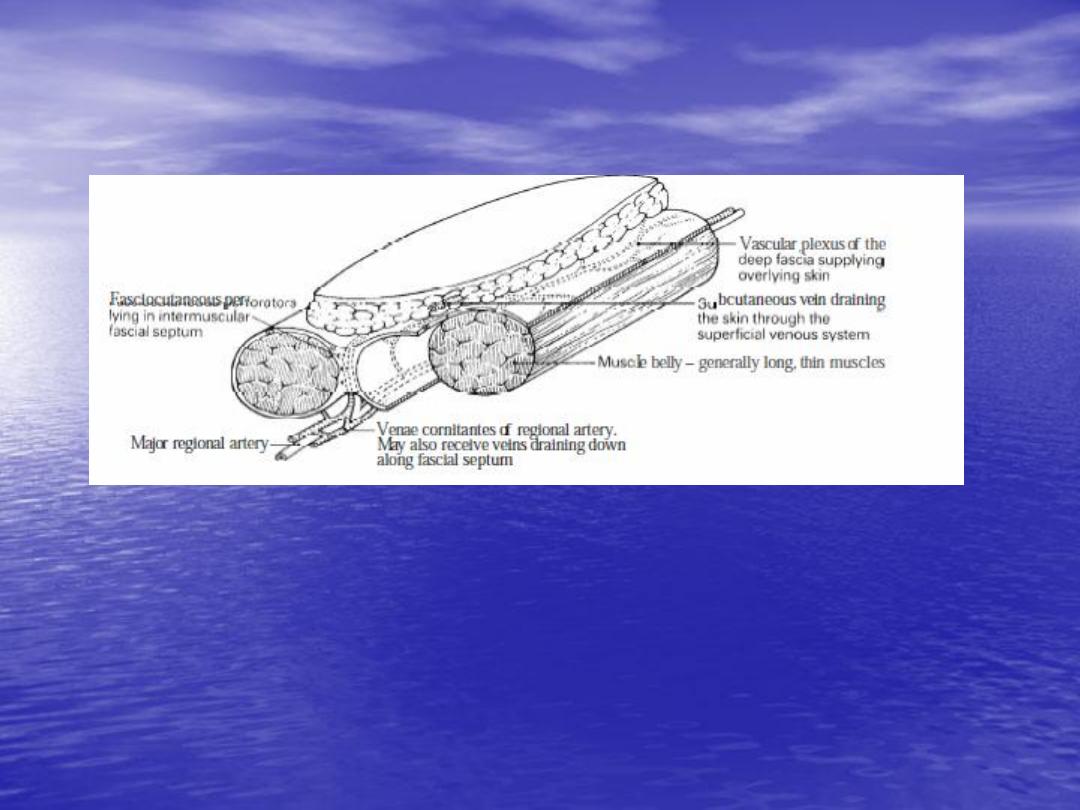
Fasciocutaneous.


Omental.
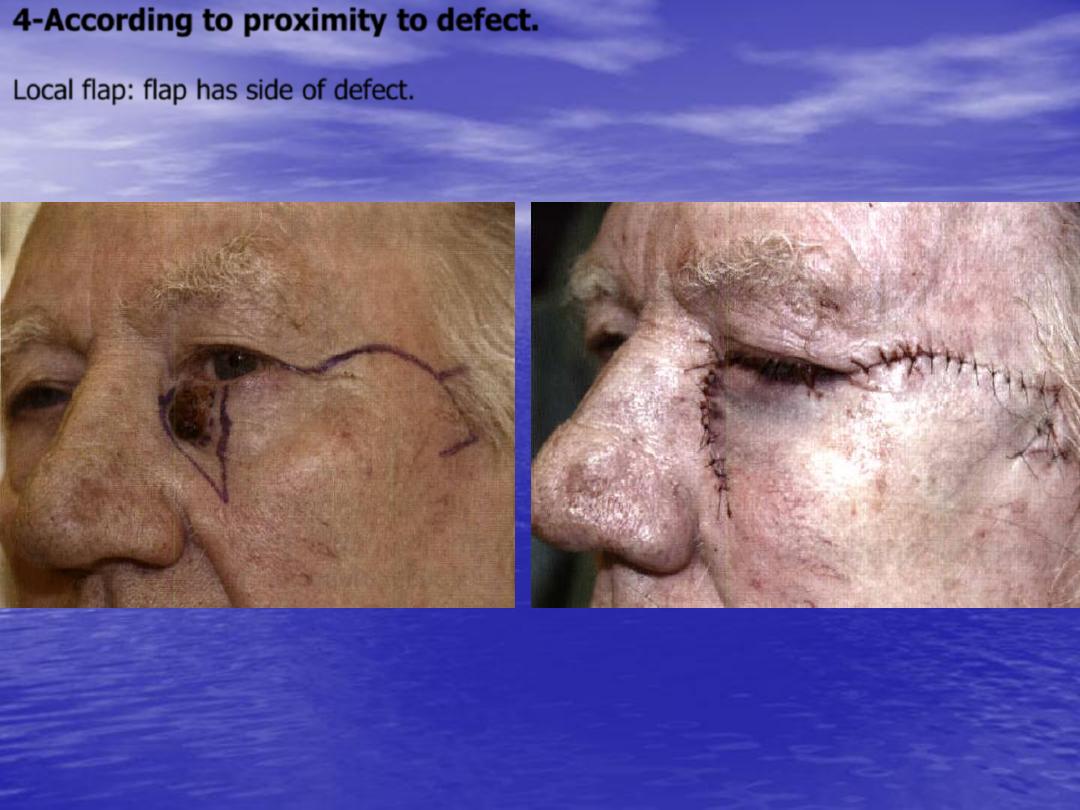
4-According to proximity to defect.
Local flap:
flap has side of defect.

Regional flap:
flap not immediate adjacent to defect e.g.
paramedian forehead flaps.

Distance flap:
not near to defect e.g. groin flap.
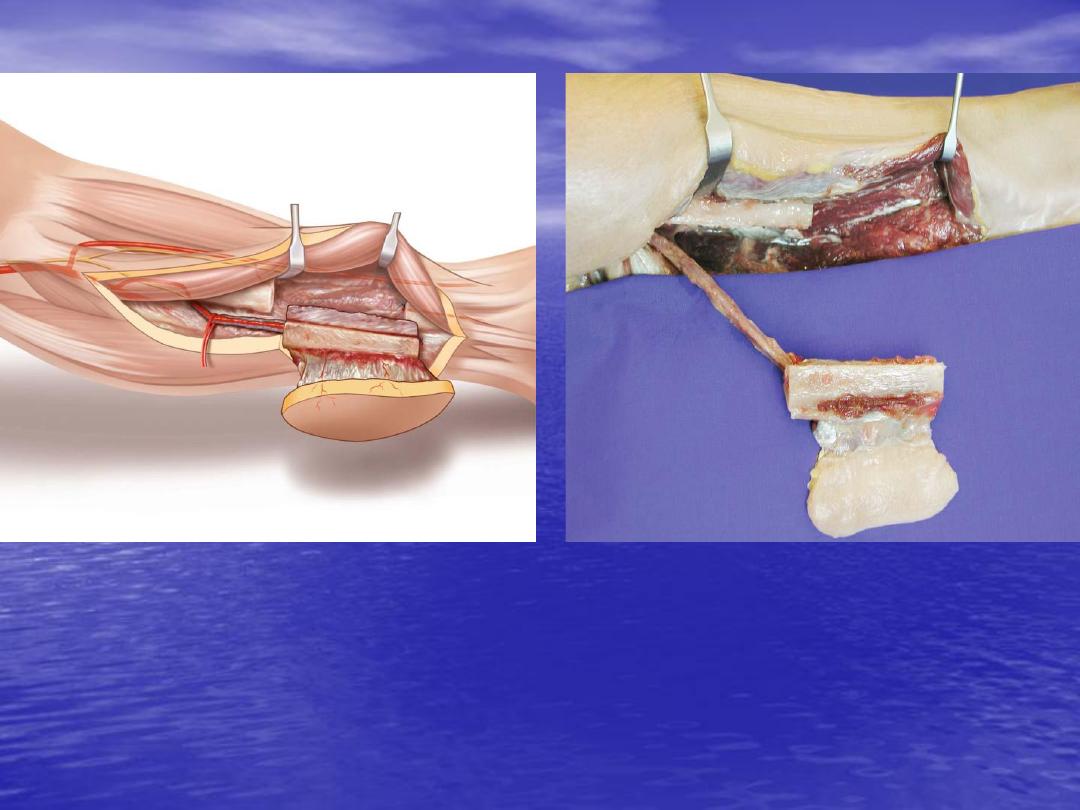
Free flap:
which mean free tissue transfer with its own
blood supply and anastomosis is done with recipient
site by microvascular surgery.
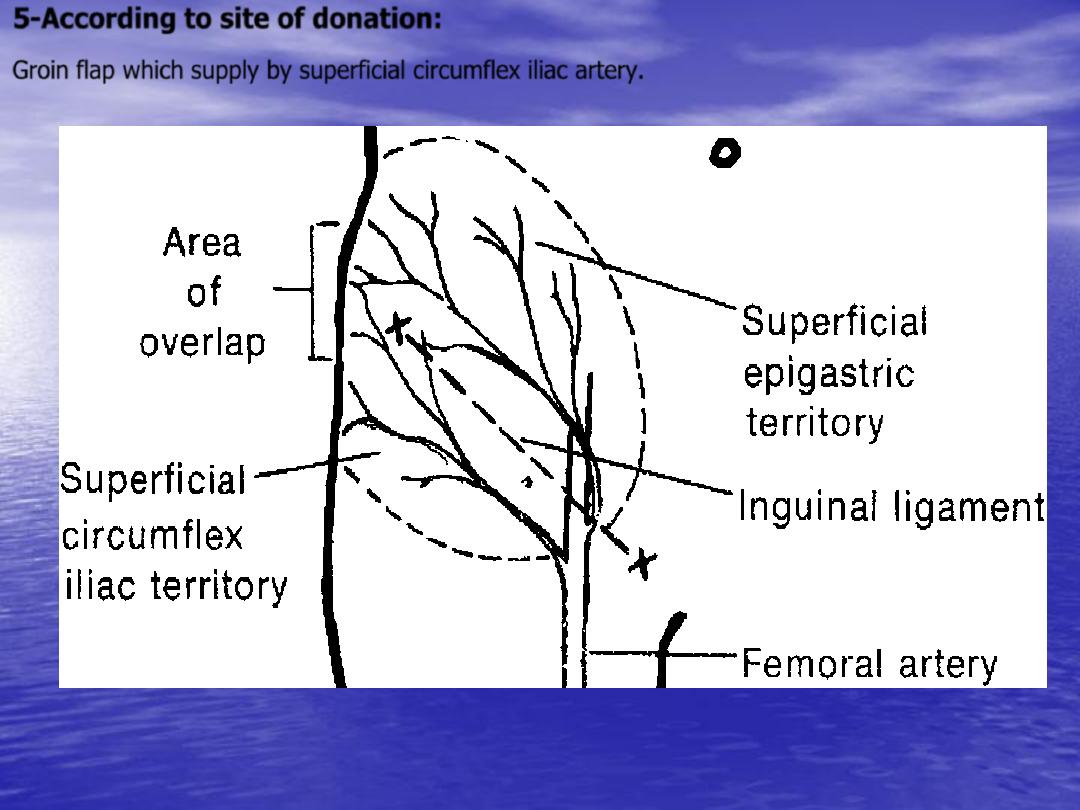
5-According to site of donation:
Groin flap which supply by superficial circumflex iliac artery.
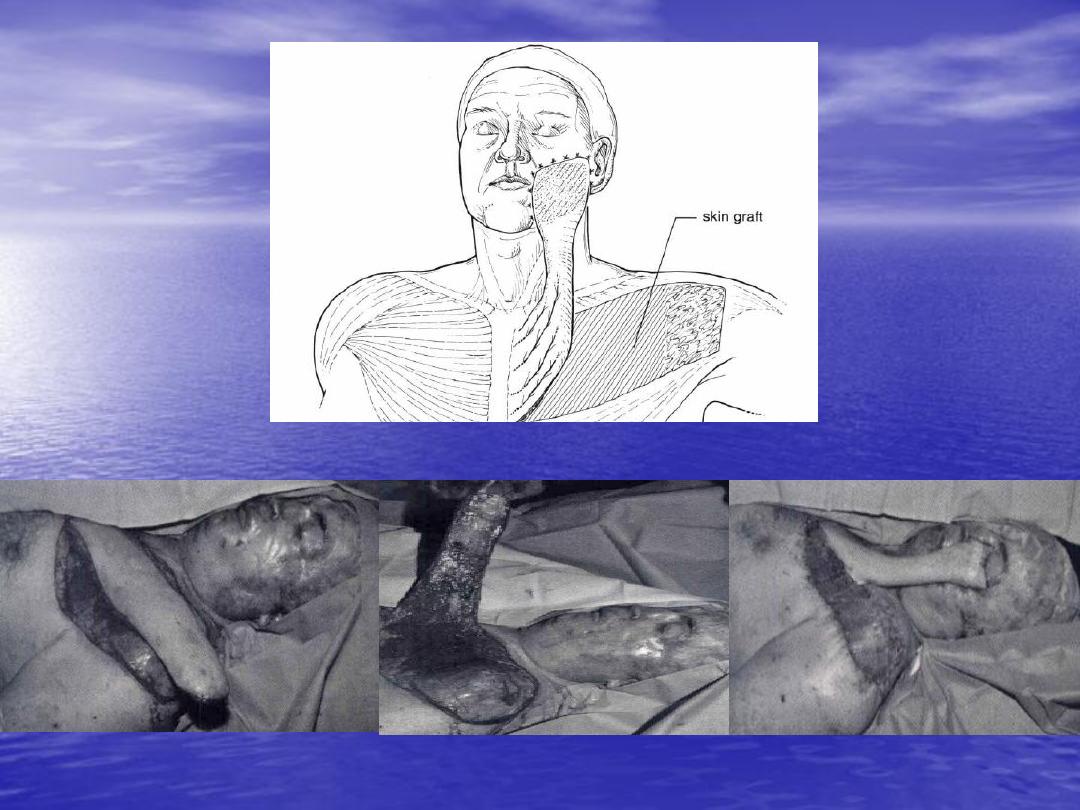
Deltopectoral flap
which supply by internal mammary
artery.

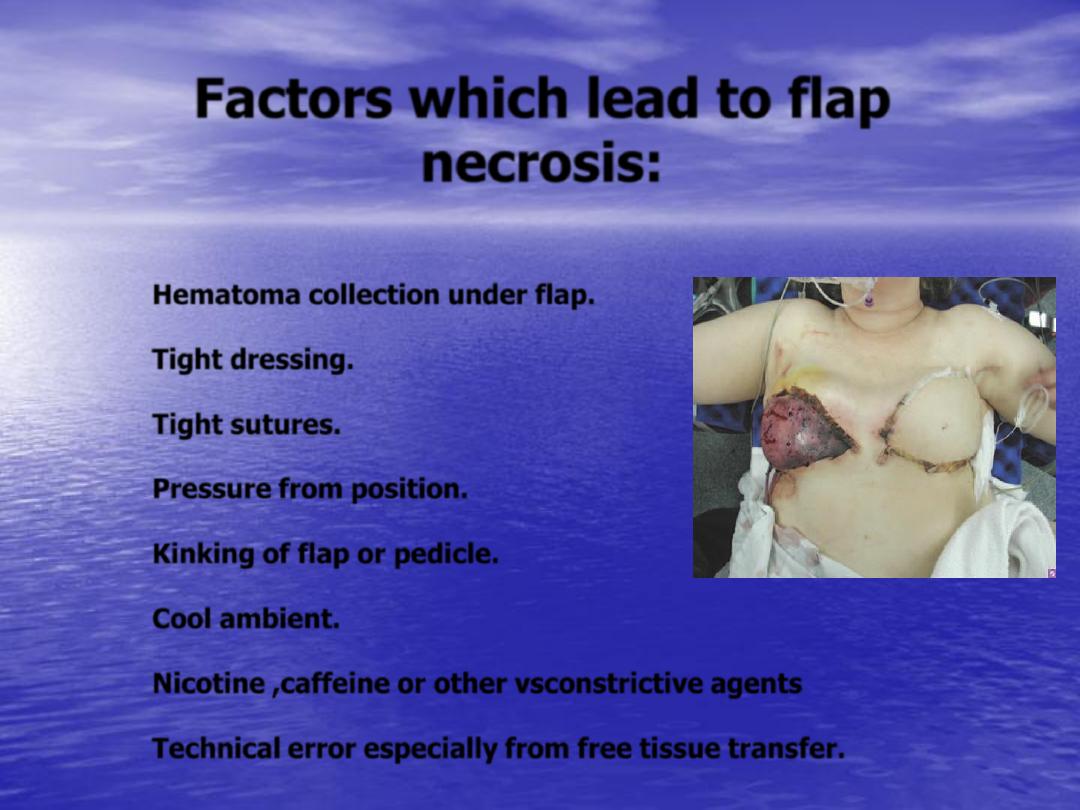
Factors which lead to flap
necrosis:
Hematoma collection under flap.
Tight dressing.
Tight sutures.
Pressure from position.
Kinking of flap or pedicle.
Cool ambient.
Nicotine ,caffeine or other vsconstrictive agents
Technical error especially from free tissue transfer.
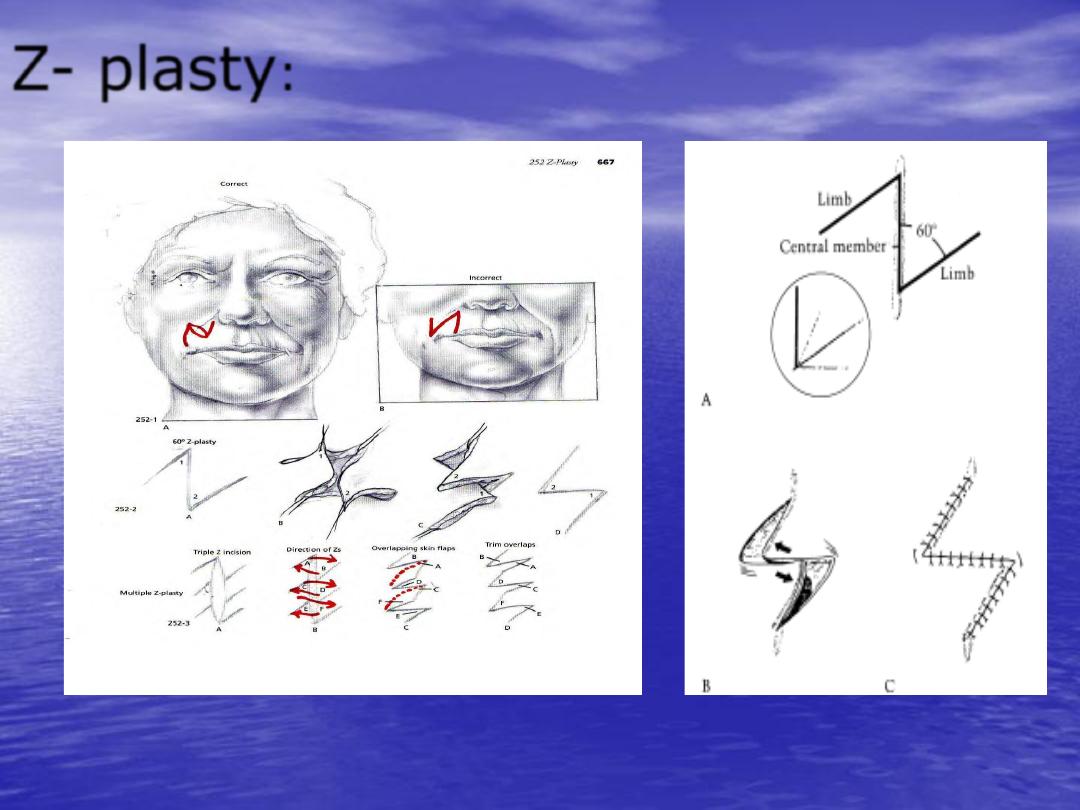
Z- plasty
:
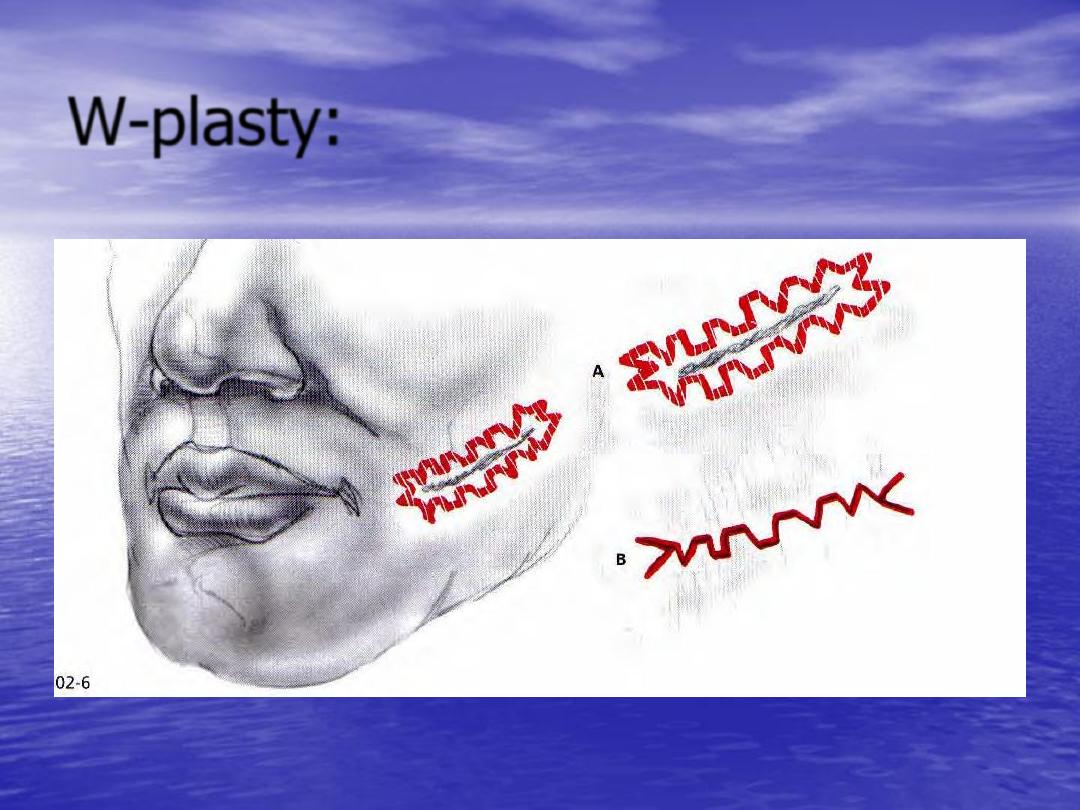
W-plasty:
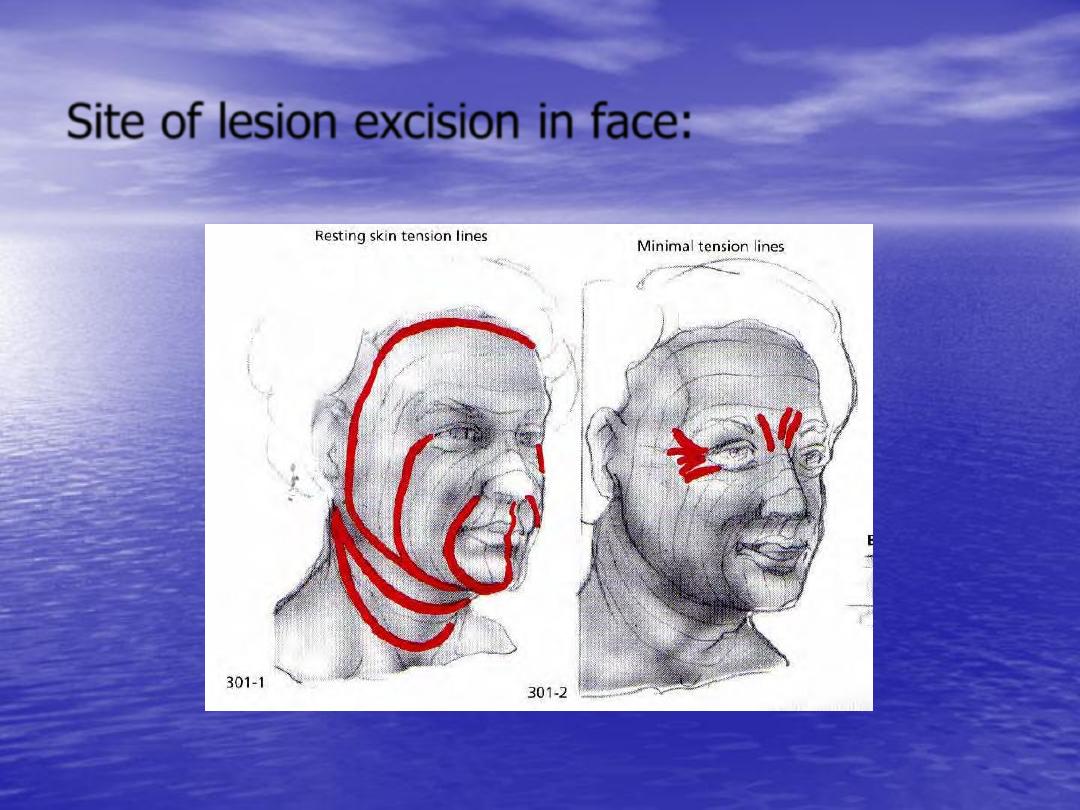
Site of lesion excision in face:
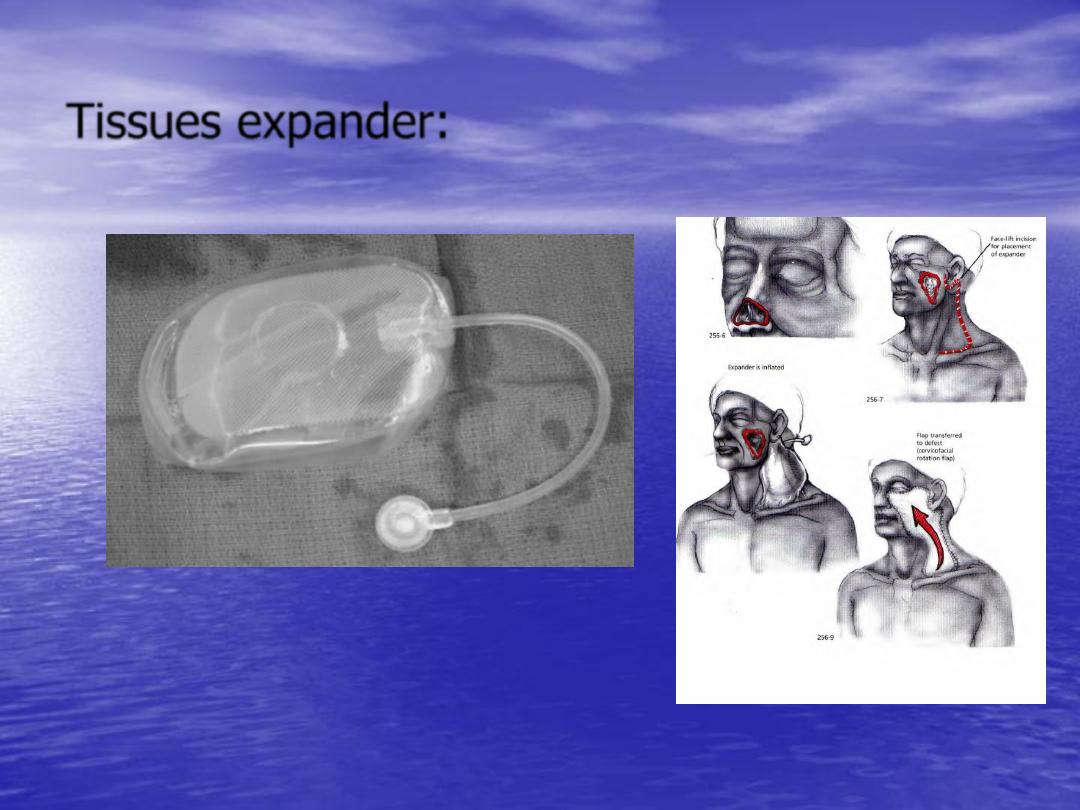
Tissues expander:

Thank you
