Page 1 of 9
Surgery Dr.Abdulhadi
PRINCIPLES OF ENDOSCOPIC STAGING AND THERAPY
§ Diagnostic and surveillance endoscopies are performed with the goal of determining the
presence and location of neoplastic disease and to biopsy any suspicious lesion.
§ Multiple (6–8) biopsies using standard size endoscopy forceps
§ Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) can be
performed in the evaluation of small lesions.
• EUS performed prior to any treatment is important in the initial clinical staging of gastric cancer.
• Careful attention to ultrasound images provides evidence of depth of tumor invasion
(T-category), presence of abnormal or enlarged lymph nodes likely to harbor cancer
(N-assessment), and occasionally signs of distant spread, such as lesions in surrounding organs (M-
category) or the presence of ascites.
• FNA of suspicious lymph nodes should be performed if it can be achieved without traversing an
area of primary tumor or major blood vessels, and if it will impact on treatment decisions
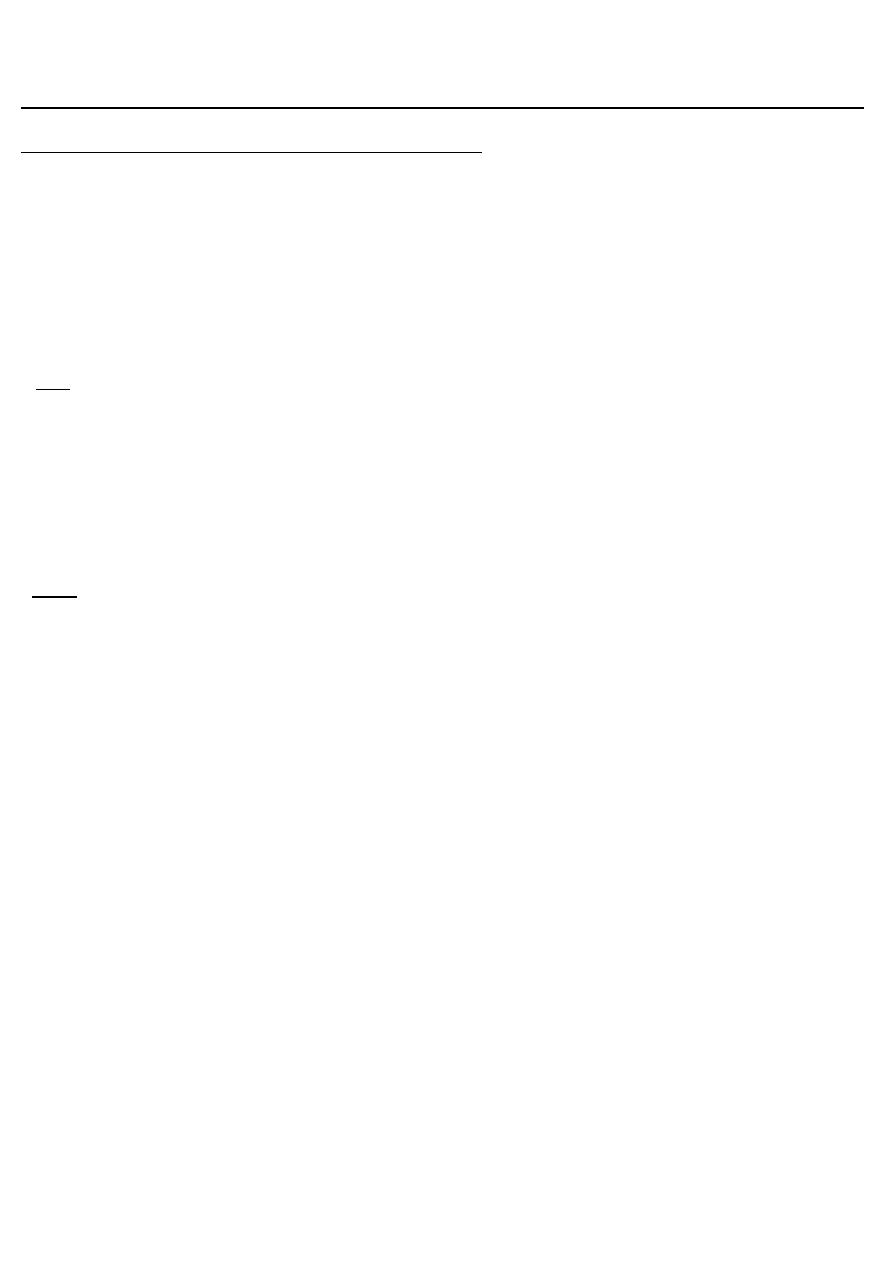
CONTRAST RADIOLOGY
— Single Contrast/ Double Contrast
— Barium Meal
— Advantages
— Sensitivity comparable to endoscopy
— Non Invasive procedure
Findings in ca stomach
§ Irregular filling defect
§ Loss of rugosity
§ Delayed emptying
§ Dilatation of stomach in carcinoma pylorus
§ Decreased stomach capacity in linitis plastica
Page 2 of 9
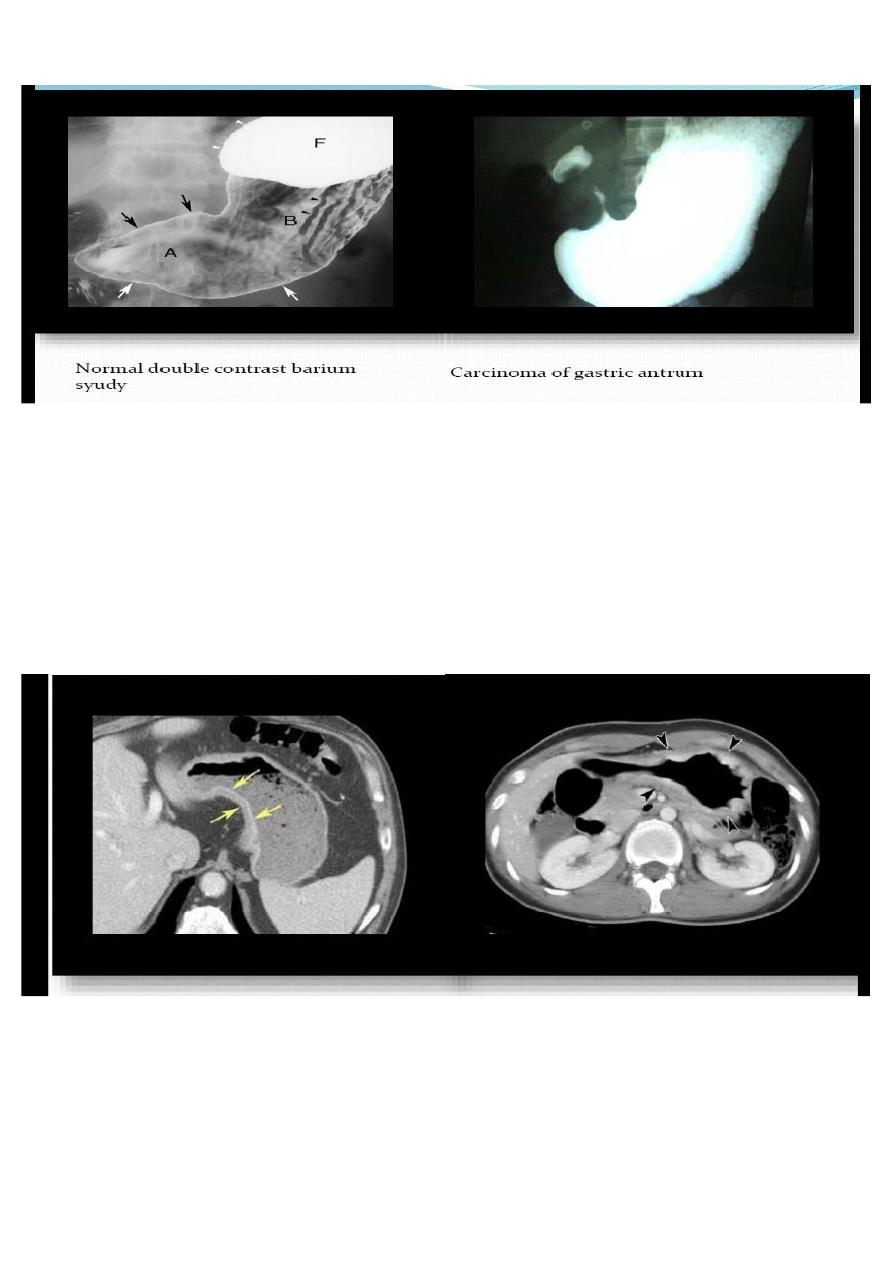
CECT CHEST, ABDOMEN AND PELVIS
- Abdominal extent of the disease
- Distant metastasis
- Involvement of celiac or periaortic nodes or extragastric disease( help to determine which lesions
extend to surgically resectable structures)
Little value in ruling out peritoneal seeding.
DIAGNOSTIC LAPOROSCOPY
• To stage the disease especially in locally advanced tumours
• Peritoneal secondaries
• Occult metastases
• Organ invasion
• Peritoneal lavage for cytology
• Biopsy of peritoneum and nodes

Page 3 of 9
Treatment:
* Surgical resection is the only curative treatment for gastric cancer and most patients with
clinically resectable locoregional disease should have gastric resection.
* Complete resection with adequate margins (4 cm or greater) is widely considered as a standard
goal, whereas the type of resection (subtotal vs. total gastrectomy) along with extent of lymph
node dissection remains a subject of controversy.
Obvious exceptions include patients who cannot tolerate an abdominal operation, and patients
with overwhelming metastatic disease.
The goal of curative surgical treatment is resection of all tumor (i.e., R0 resection). Thus, all margins
(proximal, distal, and radial) should be negative and an adequate lymphadenectomy performed.
More than 15 resected lymph nodes are required for adequate staging.
Operability
It is important that patients with incurable disease are not subjected to radical surgery that cannot
help them, hence the value of CT/PET and preoperative laparoscopy.
Unequivocal evidence of incurability
* haematogenous metastases,
* involvement of the distant peritoneum,
* N4 nodal disease and disease beyond the N4 nodes,
* and fixation to structures that cannot be removed. It is important to note that involvement of
another organ per se does not imply incurability, provided that it can be removed.
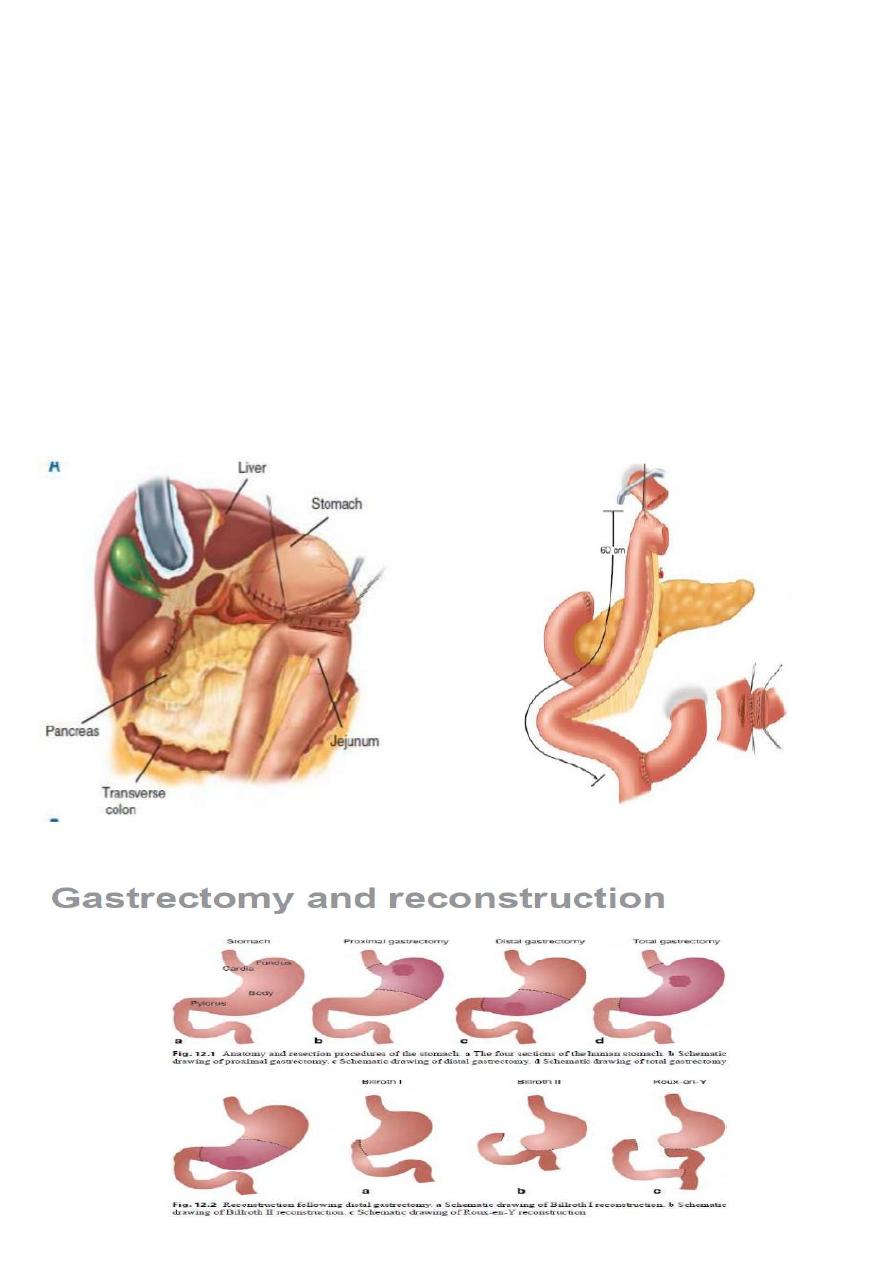
Extent of gastrectomy:
The standard operation for distal gastric cancer is
radical subtotal gastrectomy.
Unless required for R0 resection, total gastrectomy confers no additional survival benefit and may
have adverse nutritional or quality-of-life consequences and higher perioperative morbidity and
mortality.
Total gastrectomy with Roux-en-Y esophagojejunostomy
may be required for R0 resection, and may be the best operation for patients with proximal gastric
adenocarcinoma.
— R0 – no macroscopic or microscopic tumor at resection margins.
Page 4 of 9
— R1 – microscopic margins +ve.
— R2 – macroscopic margins +ve.
— AIM - R0 resection always
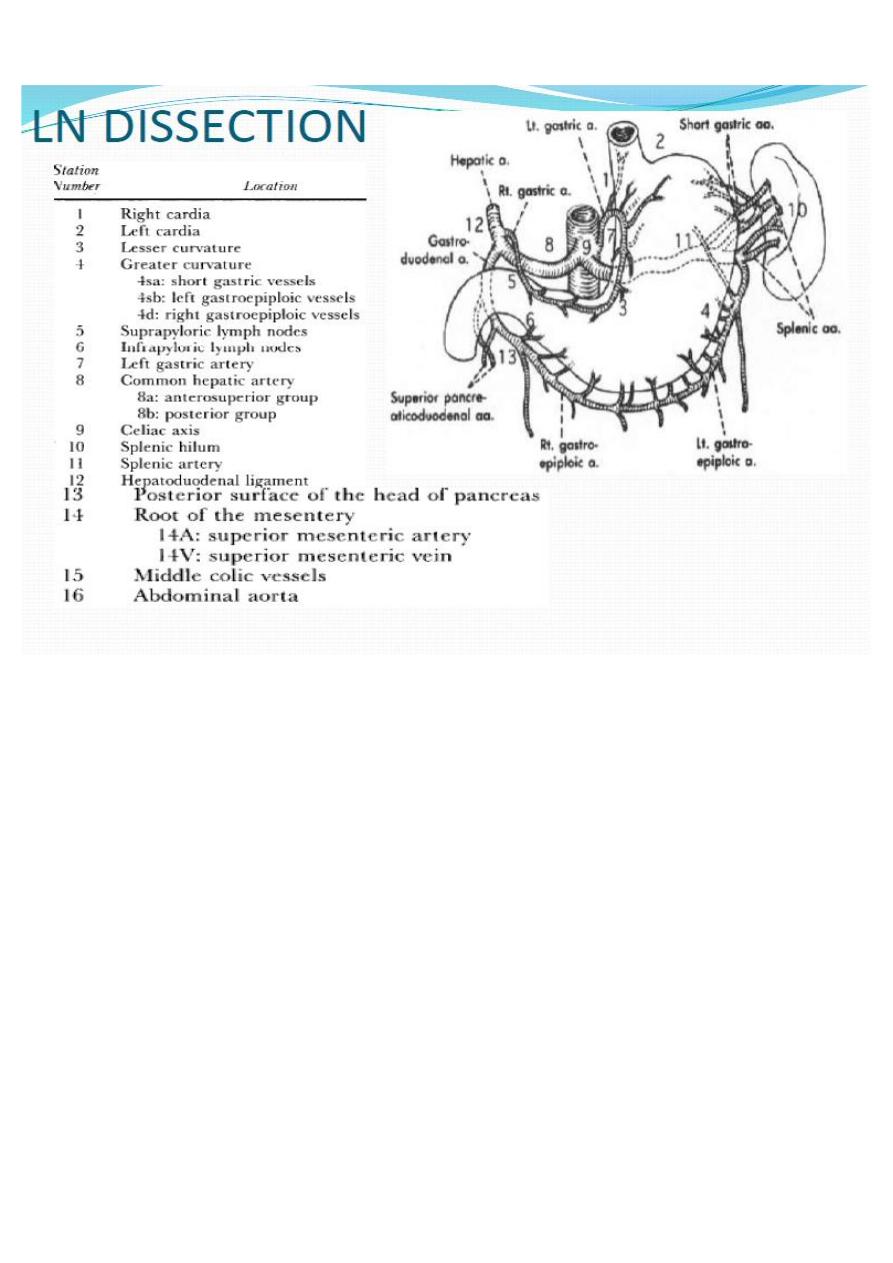
Extent of lymphadenectomy: definition of extent of lymphadectomy is different according to the
type of gastrectomy
D1 Perigastric node( Station 1-6)
D2 D1+ perarterial nodes(left gastric, hepatic, celiac, splenic)(7-11).
D3 D2+ hepatoduodenal, peripancreatic, mesenteric root, portocaval, P-A nodes, middle colic(13-
16)
Page 5 of 9
Lymph node dissection may be classified as D0, D1, or D2 depending on the extent of lymph
nodes removed at the time of gastrectomy. D0 refers to incomplete resection of N1 lymph nodes.
• D1 involves gastrectomy and the removal of the involved proximal or distal part of the stomach
or the entire stomach (distal or total resection), including the greater and lesser omental lymph
nodes (which would be the right and left cardiac lymph nodes, along lesser and greater curvature,
and suprapyloric along the right gastric artery and infra pyloric area).
• D2 involves D1 plus the removal of all the nodes along the left gastric artery, common hepatic
artery, celiac artery, splenic hilum, and splenic artery.
• The technical aspects of performing a D2 lymph node dissection require a significant degree of
training and expertise.
SPLENECTOMY is sometimes performed, particularly in cancers of proximal third of stomach and
tumours of the body near the greater curvature .
Cancers in these locations are more likely to metastasize to lymph nodes in the splenic hilum that
can not be excised without splenectomy.

Page 6 of 9
Radiation therapy for Gastric Cancer:
RT (preoperative, postoperative, or palliative) can be part of treatment for gastric cancer.
Indications-
• T3-4 resectable disease
• Margins positive
• Residual disease
• LN +ve disease
• Inoperable
Radiotherapy has a role in the palliative treatment of painful bony metastases.
Postoperative Chemotherapy
Gastric cancer may respond well to combination cytotoxic chemotherapy , and neoadjuvant
chemotherapy improves the outcome following surgery.
Most patients therefore should have prior chemotherapy.
Chemotherapy for advanced disease is palliative.
Targeted Therapies
Newer biological agents such as trastuzumab (Herceptin) offer potential advantages to survival in
the minority of patients (<20%) with HER2-positive for the treatment of advanced or metastatic
gastric cancer.
CONCLUSION
§ Endoscopy with direct visualisation, cytology and biopsy yields the diagnosis in > 90% of patients.
§ Locally advanced disease is the most common presentation.
§ Only curative treatment is surgical resection of all gross and microscopic disease.
§ Even after curative gastrectomy, disease recurs in local or distant site or both in the majority of
patients.
§ Efforts to improve these poor results have focused on developing pre and postoperative systemic
and local adjuvant therapies.
§ Chemoradiation is the preferred adjuvant modality in patients with stage IB, II, IIIA, IIIB or IIIc and
M0 gastric cancer.
§ In case of locally unresectable disease, combined modality therapy is reasonable approach.

Page 7 of 9
GASTROINTESTINAL STROMALTUMOURS
GISTs comprise 1–3% of all gastrointestinal neoplasia.
Gastrointestinal stromal tumours (GISTs) may arise in any part of the gastrointestinal tract but 50%
will be found in the stomach. Previously named leiomyoma and leiomyosarcoma, the term GIST is
now used .
They are tumours of mesenchymal origin and are observed equally commonly in males and
females.
The tumours are universally associated with a mutation in the tyrosine kinase c-kit oncogene.
These tumours are sensitive to the tyrosine kinase antagonist imatinib, and an 80% objective
response rate can be observed.
Size and mitotic index are the best predictors of metastasis. Peritoneal and liver metastases are
most common but spread to lymph nodes is extremely rare.
Because the mucosa overlying the tumour is normal, endoscopic biopsy can be uninformative
unless the tumour has ulcerated. Targeted biopsy by endoscopic ultrasound is more helpful.
Tumours over 5 cm in diameter should be considered to have metastatic potential.
* If easily resectable, surgery is the primary mode of treatment.
* Smaller tumours can be treated by wedge excision.
* Larger tumours may require a gastrectomy or duodenectomy but lymphadenectomy is not
required.
* Larger tumours which require multivisceral resection may be better treated with 3–6 months of
imatinib prior to operation as this will usually radically reduce the size and vascularity of the
tumours.
*Adjuvant imatinib for large resected tumours of high malignant potential should probably be
continued indefinitely.
The prognosis of advanced metastatic GISTs has been dramatically improved with imatinib
chemotherapy but resection of metastases, especially from the liver, still has an important role.
GASTRIC LYMPHOMA
Primary gastric lymphoma accounts for approximately 5% of all gastric neoplasms. Gastric
lymphoma is most common in the sixth decade and the presentation is no different from gastric
cancer, the common symptoms being pain, weight loss and bleeding.

Page 8 of 9
Acute presentations of gastric lymphoma such as haematemesis, perforation or obstruction are
not common.
Primary gastric lymphomas are B-cell derived, the tumour arising from the mucosa-associated
lymphoid tissue (MALT). Primary gastric lymphoma remains in the stomach for a prolonged period
before involving the lymph nodes.
At an early stage, the disease takes the form of a diffuse mucosal thickening, which may ulcerate.
Diagnosis is made as a result of the endoscopic biopsy and seldom on the basis of the endoscopic
features alone, which are not specific.
Following diagnosis, adequate staging is necessary, primarily to establish whether the lesion is a
primary gastric lymphoma or part of a more generalised process.
CT scans of the chest and abdomen and bone marrow aspirate are required, as well as a full blood
count.
Although the treatment of primary gastric lymphoma is somewhat controversial, it seems most
appropriate to use surgery alone for the localised disease process.
No benefit has been shown from adjuvant chemotherapy, although some oncologists contend that
primary gastric lymphoma can be treated by chemotherapy alone.
Chemotherapy alone is appropriate for patients with systemic disease.
Some of the more controversial aspects of gastric lymphoma concern the role of H. pylori. It has
also been shown that early gastric lymphomas may regress and disappear when the Helicobacter
infection is treated (Isaacson).
Gastric involvement with diffuse lymphoma
These patients are treated with chemotherapy, sometimes with dramatic and rapid responses.
Surgeons are frequently asked to deal with the complications of gastric involvement.
The two common complications are bleeding and perforation. Both may occur at presentation, but
more usually may follow the chemotherapy when there is rapid regression and necrosis of the
tumour. These operations can be technically very challenging and normally require gastrectomy.
Duodenal tumours
● Duodenal villous adenomas are commonly found around the ampulla of Vater and are
premalignant
● Duodenal carcinoma is uncommon, but the commonest site for adenocarcinoma is in the small
intestine
Page 9 of 9
●Both adenoma and carcinoma occur commonly in patients with familial polyposis and screening
these patients is advised .
Poor prognostic features in the resected specimen include regional lymph node metastases ,
transmural involvement and perineural invasion.
Curative surgical treatment will normally involve a pancreaticoduodenectomy (Whipple’s
procedure).
● Pancreatic cancer is the most common cause of duodenal obstruction .
Neuroendocrine tumours
A number of neuroendocrine neoplasms occur in the duodenum. It is a common site for primary
gastrinoma (Zollinger–Ellison syndrome).
Non-functioning neuroendocrine tumours (usually called carcinoid tumours) also occur but
uncommonly in comparison to the ileum.
Zollinger–Ellison syndrome
This syndrome is mentioned here because the gastrin producing endocrine tumour is often found
in the duodenal loop, although it also occurs in the pancreas, especially the head. It is a cause of
persistent peptic ulceration .
The advent of proton pump inhibitors such as omeprazole has rendered this extreme endocrine
condition fully controllable, but also less easily recognised.
Gastrinomas may be either sporadic or associated with the autosomal dominantly inherited multip
endocrine neoplasia (MEN) type I.
The tumours are most commonly found in the ‘gastrinoma triangle’
