
Well Baby Clinic
Dr.Mazin Al-Jadiry
1
12 November 2012
Well baby clinic
Learning objectives
Describe the purpose of prenatal history.
Recognize the significance of common abnormalities found shortly after birth as well as
the careful examination of the newborn..
Explain when and what are the appropriate outpatient follow-up for the healthy Infant.
The Newborn at birth
The whole key to the management of the newborn infant lies in a proper assessment of the
baby at birth.
This necessitates obtaining certain basic information in relation to two different individuals, the
mother and the baby, and obtained in two completely different ways, by the history and by the
physical examination.
History
The mother: This includes;
1. Pregnancy-related health issues
2. Important are the parent’s blood groups and Rh antigen, duration of labour, whether or
not there was an operative delivery, drugs and anaesthetics.
3. Antenatal Ultrasound Findings (heart, brain and kidneys)
This information will have determined whether the baby is at risk in terms of the mother having a 'high
risk' pregnancy or labour.
The baby:
1. Condition at birth and Apgar scores at 1 and 5 minutes after birth and details of any
resuscitative measures used (this information should be present with the baby’s card
after delivery).
2. Vitamin K administration

Well Baby Clinic
Dr.Mazin Al-Jadiry
2
12 November 2012
Examination
Importance
1. Earliest possible detection of deviations from normal.
A. Major deviations: Serious correctable congenital malformations;
I.
Early diagnosis enables treatment that makes the difference between life
and death, e.g. oesophageal atresia, imperforate anus, and diaphragmatic
hernia.
II.
Early diagnosis enables treatment that reduce the incidence of permanent
and severe disability, e.g. congenital dislocation of the hips and club feet
B. Minor deviations: Enables the doctor to give parents a clear explanation about
minor deviations from usual (if present, eg birth marks, acrocyanosis) which if not
explained are likely to cause concern.
2. Establishes a baseline for subsequent examinations.
When
1. Immediately after birth
2. Before discharge from maternity unit
3. As a scheduled visits for 2 years
4. Whenever there is any concern about the infant's progress
General
It is important that a few exact measurements be made and recorded:-
Weight
Crown-heel length
Head circumference.
These should be plotted on the appropriate centile chart as all parameters of growth need to be related
to gestational age for sensible interpretation.
Record respiratory rate and heart rate with infant quiet. Your routine examination
should be flexible.
If the infant is quiet and relaxed when first approached, auscultation of heart and palpation of abdomen
should precede more disturbing examinations such as those of the mouth and hips.
If the infant is struggling and crying during auscultation of the heart, then temporary shunt reversal may
prevent hearing of a murmur present when the baby is at rest.
Overall Inspection
In general does he look ill or well?
Is he normally active?
Is the cry normal?
Are there any obvious malformations? (e.g. with Down Syndrome?)
What is his colour? Pallor? Cyanosis? Plethora? Jaundice?
What is his respiration? Chest movements? Is there a grunt?
The apex beat is frequently visible on inspection.
What is the shape of the head?

Well Baby Clinic
Dr.Mazin Al-Jadiry
3
12 November 2012
What a normal new baby can do?
Newborn babies are able to do many things besides cry.
There are times when they sleep and times when they are awake.
They can move their arms, legs and head.
They can stretch, hiccup, sneeze and make many other movements.
They are also able to receive a certain amount of information from the world around them
through the five senses-
Sight
Hearing
Touch
Smell
Taste
Well-Baby examination
Well-baby examinations are scheduled regularly during the first two years of life due to the
rapid growth and change that occurs during infancy.
During each visit the pediatrician monitors, advises, and answers questions on a baby's growth
and development.
The Pediatrician should see the infant for a check-up
At birth,
Two weeks,
Two months,
Four months,
Six months,
Nine months,
12 months,
15 months,
18 months,
24 months, and
Annually thereafter.
A well-baby exam consists of :
1. Answer parent’s questions about the baby's general health and development
2. Physical exam: measurements of length/ height, weight and head circumference, vital signs, and
a general physical examination.
Weight is a pediatric vital sign, because of dosing considerations and the importance of
growth as an indicator of chronic disease in children.
3. Special attention is paid to whether the baby has met normal developmental milestones.

Well Baby Clinic
Dr.Mazin Al-Jadiry
4
12 November 2012
I.
At birth
Starting with the obstetric dates, the examination of the baby can aid in assigning a
correct gestational age to detect those at risk babies.
Head to-toe exam. With special attention to:
Head circumference
Genitalia
Presence of neonatal reflexes
Metabolic screen to assess thyroid activity, and for phenylketonuria (PKU), a genetic
disorder than can be easily corrected by diet.
Blood glucose screening should be performed on infants at risk for hypoglycemia, e.g.
infants of diabetic mothers
Vitamin K administration after delivery reduces the risk of hemorrhagic disease in the
newborn.
Recommend human milk for all infants (except if there is a contraindication)
Discharge
Most infants are ready for discharge at 48 hours after a vaginal delivery and 72 to 96
hours after a cesarean section delivery.
The infant is medically ready for discharge when:
He or she has stable vital signs for at least 12 hours
Appears healthy and has normal physical examination
Passed stool and voided
Is feeding well
Has completed all screening tests, and
Has appropriate follow-up care planned.
Norms in the first few days after birth
The 4- to 5-day-old infant who is consuming an adequate amount of
human milk should have 6 to 8 voids and yellow, seedy stools daily;
have lost no more than 7% to 8% of birth weight; and be satisfied after
20 to 30 minutes of nursing.
Achieving the same birth weight at 10-14 days of life
II.
At two weeks: The first well-baby visit occurs.
The first outpatient visit must occur several days after hospital discharge or after
2weeks from birth to evaluate general well-being.
complete head to-toe exam will be performed

Well Baby Clinic
Dr.Mazin Al-Jadiry
5
12 November 2012
Developmental milestones that represent a normal progression of physical and mental
maturity should be assessed
If BCG, Oral Polio Vaccine, Hepatitis B vaccine were not given in the hospital, the first
shot may be given at this visit.
The two-month: visit will be a repeat of the two week visit with a physical exam, developmental
and behavioral assessment, guidance for upcoming developmental changes, and immunizations
(Pentavalent vaccine (DTP-1, Hib1, and HBV-2), OPV1 and Rotavirus1).
III.
The four & six-month exam:
Physical exam, developmental and behavioral.
Discuss adding solid foods to the baby's diet, usually in the form of cereal then pureed
food.
Immunization
IV.
The 9-mo & 1-yr exam: quite a change in baby from birth.
Answer questions regarding the baby's sleep habits, feeding patterns, teething, standing
up, walking and talking.
The physical exam is performed, plotted on the standard growth curve, and any
deviations are noted.
A blood test for anemia may be performed
Growing up
Involves three major dynamic processes:
Growth
Development
Sexual Maturation
Physical Growth
Increase in the size of the body as a whole or the increase in its separate parts.
Growth milestones are the most predictable
It is essential to plot the child’s growth on gender and age appropriate charts

Well Baby Clinic
Dr.Mazin Al-Jadiry
6
12 November 2012
The growth of a child occurs in four phases:
Fetal Growth
Prenatally, the growth of the head predominates, reaching the peak in the third trimester.
The size of an infant at birth, which correlates poorly with ultimate adult height, is affected:
primarily by maternal size
Secondarily by other intrauterine factors such as maternal nutrition and use of
tobacco and alcohol, placental adequacy, intrauterine infection and gestational age
at birth.
Infantile Growth
During the first 12–24 months after birth, the time of greatest postnatal growth velocity, the
infant “seeks his or her own curve.” That is, by age 2–3 years, the child's stature reflects his
or her own genetic endowment rather than his or her mother's size and health.
Growth of the brain occurs almost exclusively during the early years of life. At birth, it is 25%
of adult size and at 1yr, 75%. Full development is not achieved until adolescence.
Juvenile and adolescent Growth
Growth during the remainder of childhood occurs at a rate of 5–6 cm per year, along the
percentile band achieved by 2–3 years.
Adolescence is characterized by an abrupt, short-lived increase in growth velocity (the
“growth spurt”), mediated by gonadal & growth hormones.
Well Baby Clinic
Dr.Mazin Al-Jadiry
7
12 November 2012
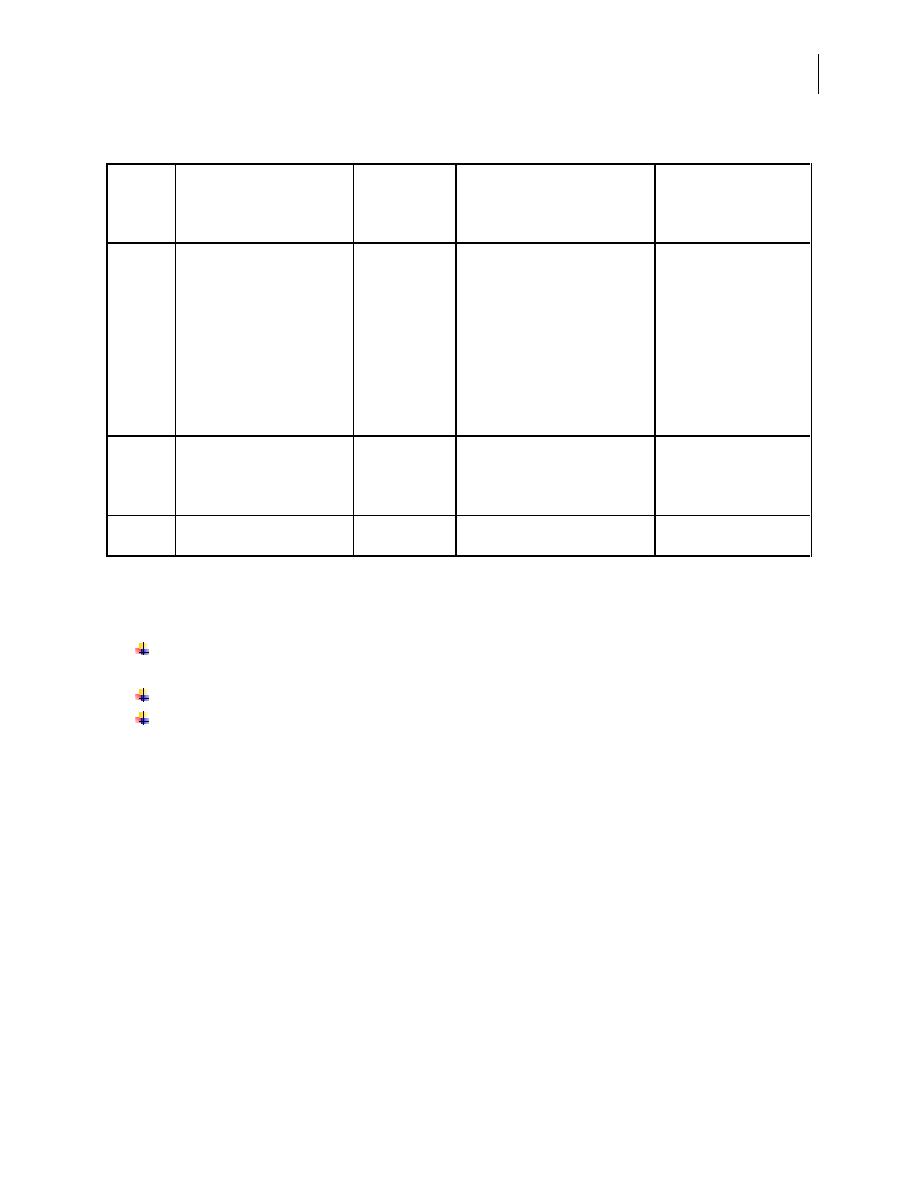
Normal growth and rule of thumb:
Age
OCCIPITOFRONTAL
CIRCUMFERENCE
HEIGHT
WEIGHT
DENTITION
Birth 35 cm
+2cm/mo (0 to 3 mo)
+1cm/mo (3 to 6 mo)
+0.5cm/mo (6 to 12 mo)
Mean = 1cm/mo
50.8 cm
+ 25.4cm
3 to 3.5 kg
Regains birthweight by 2 wk
Doubles birthweight by 5 mo
Central incisors—6mo
Lateral incisors—8mo
1 year 47 cm
+ 2cm
76.2 cm
+ 12.7 cm
10kg
Triples birthweight
First molars—14 mo
Canine –19 mo
2year
49 cm
88.9 cm
12 to 12.5 kg
Second molars—24mo
Growth assessment
For infants, the measure of linear growth is length, taken by two examiners (one to position the
child) with the child supine on a measuring board.
For older children, the measure is stature, taken with a child standing on a stadiometer.
The data are presented in five standard charts:
1. Weight for age;
2. Height (length and stature) for age;
3. Head circumference for age;
4. Weight for height (length and stature); and
5. Body Mass Index (BMI)= weight (kg)/height (m)2



