Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
1
White & Red Lesions of The Oral Mucosa
Oral submucous fibrosis (OSF):
OSF is a high-risk, precancerous condition characterized by chronic,
progressive scarring of the oral & oropharynx mucosa. It is seen
primarily in the Indian subcontinent, Southeast Asia, Taiwan, southern
China, Polynesia, and Micronesia. Cases among Asian communities out
of Asia, also have been reported.
It’s a slowly progressive chronic fibrotic disease. In the earliest stages
there may be a burning sensation and scattered small vesicles, followed
by fibro-elastic changes and inflammation of the mucosa with epithelial
atrophy and scarring leading to a progressive stiffness of the oral
mucosa, trismus & inability to open the mouth, eat & swallow, or speak.
Lesions may also appear as leukoplakia or erythroplakia patch.
Etiology:
1. As the lesion is mostly seen in Indian and other Asian people, the
etiology is mostly linked to the use of betel quid and related products
(chewing or sucking)
# The quid consists of a betel leaf wrapped around a mixture of areca
nut, slaked lime, possibly tobacco, and sometimes sweeteners and
spices. Chewed for many hours
# The slaked lime releases alkaloids from the areca nut to produce a
euphoric feeling for the user. All these products are irritant to the
mucosa
2. Excessive consumption of chilies & hot spices are also thought to have
a role in the etiology of OSF.
3. Tobacco (Chewing)
Note: At the site of chewing betel quid, the teeth are typically stained
dark red, with severe periodontitis, and burning sensation when there
are atrophic or erythematous lesions.
Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
2
Diagnosis: # History & clinical examination. # Biopsy
Treatment:
1. Abstain the habits
2. Vitamins, minerals, & antioxidants rich diet
3. Steroids: intra-lesional, topical & systemic
4. Intra-lesional injection of interferon-gamma
5. Topical or intra-lesional proteolytics (e.g collagenase, hyaluronidase,
chymotrypsin, and human placental extract)
6. Pentoxifylline (for muscle pain and trismus)
7. Physiotherapy & exercises for trismus
8. Surgical excision
9. Laser therapy
10. Clinical follow up for any malignant changes
Lupus erythematosus
It's a chronic immunologically mediated inflammatory disorder of the
skin, connective tissue (CT) and specific internal organs.
that represent the severity and distribution
3 clinical forms
It occurs in
of involvement:
1. The mildest form is called Discoid LE, its chronic lesions confined to
the sun exposed skin of the face scalp & ears, as well as oral mucosa.
2. The intermediate form is called acute cutaneous LE, it's widely spread
& affects the head, neck, upper trunk & extensor surfaces of the arms.
3. The severe form is called systemic LE, in addition to the skin, it
involves many organs such as kidneys, heart, lungs & bone marrow.

Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
3
Other classification may include:
a. Relatively mild skin disease, chronic cutaneous LE (CCLE) (discoid)
b. Serious systemic disease, systemic LE (SLE)
c. An intermediate disease, sub-acute cutaneous LE (SCLE)
# Another classification may include (Systemic, Discoid, Drug-induced,
Neonatal).
# Oral lesions observed in Discoid & Systemic LE, however, it may
present in the other forms of LE.
Systemic Lupus erythematosus (SLE):
The disease onset is at 15-45 years of age. It occurs in both males and
females, more common in females. It’s essentially a skin disease and
involves many organs such as CT, muscles, bone & bone marrow, heart,
blood vessels, kidneys, & lungs. Oral MM involved in about 20-30% of
cases.
Common symptoms include: Painful & swollen joints (arthralgia), fever,
malaise, chest pain, hair loss, oral ulcers, swollen lymph nodes,
tiredness, & a red rash which is most commonly on the face. The lesions
and symptoms associated with great variety of autoantibody production
particularly antinuclear.
SLE may also occur with other rheumatologic disorders such as
secondary Sjögren’s syndrome & mixed connective tissue disease.
Discoid Lupus erythematosus (DLE):
DLE is a relatively common form of LE. It’s essentially a skin disease with
mucocutaneous lesions indistinguishable from those of systemic LE. DLE
predominantly affects adults in the third or fourth decade of life.

Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
4
The lesions may be associated with arthralgia but rarely significant
autoantibody production. The most common sites of DLE lesions are the
sun exposed skin areas favoring the face, ears, and scalp. Oral MM
involved in around 20-50% of cases. Sometimes other body areas may
be involved especially when they are exposed to sun such as chest, back
and extremities.
Skin lesions of LE:
1. The classical skin lesions of LE first present as slightly elevated red or
purplish patches or flat macules (disc-shaped in DLE) which are often
covered by white/grayish or yellowish adherent scales.
2. Finally, the lesions develop (heal with) extensive atrophic scarred
centers with pink or red peripheries.
3. In darker skin, the lesions often lose skin pigmentation in the center
(become lighter) and develop increased, dark skin pigmentation (rim)
around the center of the lesion (appear darker than the surrounding
normal skin).
4. In lighter skin, the lesions may develop a gray color or have very little
color change.
Oral lesions of LE:
1. Oral involvement is reported in 20-50 % of cases of DLE & 20-30% of
cases in SLE.
2. The oral lesions appear prior to or following the skin lesions.
3. The oral lesions begin as erythematous areas.
4. Superficial painful ulcerations may occur with crusting and bleeding.
5. The margins are not sharply demarcated but frequently show a
narrow zone of keratinization with fine white striae radiate out from the
margins.

Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
5
6. Sometimes the erythematous, atrophic center of the lesion may show
a fine stippling of white dots.
7. DD Atrophic & Erosive LP.
Diagnosis of LE:
1. History & clinical examination
2. Histopathology
3. Direct IF reveals deposition of antibodies at BM zone {granular
deposition of IgM, IgG, IgA, and C3 (lupus band test)}.
4. Laboratory findings including:
a. Antinuclear antibodies is positive (Specific)
b. Rh factor is positive
c. Anemia
d. Leukopenia
e. Thrombocytopenia
f. ESR is increased
g. False positive serological test for syphilis
Treatment of LE:
1. Drug of choice is corticosteroid
# To obtain relief of symptoms, potent topical steroids such as
clobetasol propionate gel 0.05%, betamethasone dipropionate 0.05%, or
fluticasone propionate spray 50 μg aqueous solution are usually
required.
Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
6
# The treatment may begin with applications two to three times a day
followed by a tapering during the next six to nine weeks. The overall
objective is to use a minimum of steroids to obtain relief
2. Immunosuppressive drugs. Along with antifungals/antivirals to
prevent/treat opportunistic fungal/viral infections
3. Antimalarial drugs:
# Chloroquine 250mg tab twice daily
# Hydroxychloroquine 200mg tab twice
4. Keratolytic agents: Retinoids (Retin A®) & Isotretinoin.
5. Laser therapy.
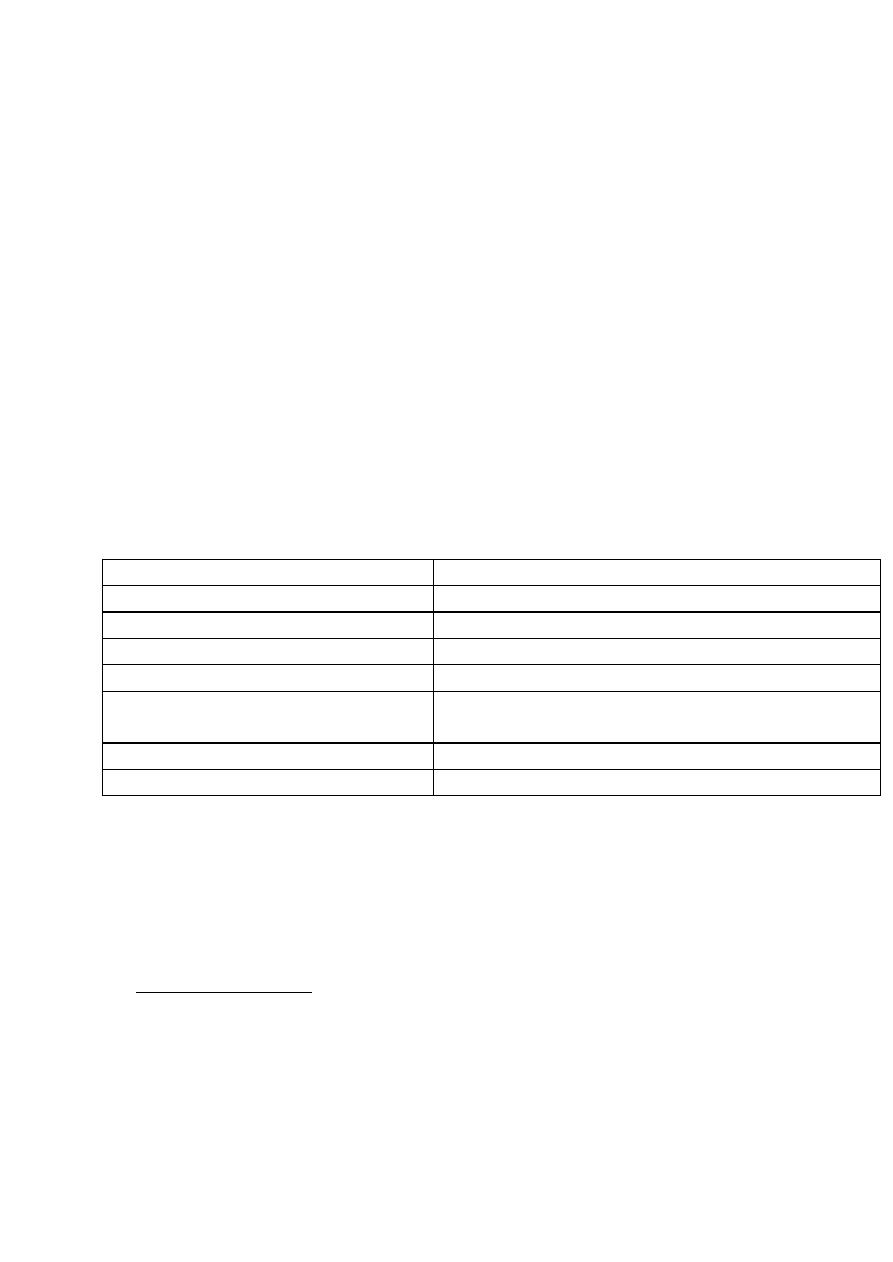
Table. Topical Therapy for Oral Lesions of Lupus Erythematosus
Directions for Use†
Topical Steroid Therapy
Place on affected area(s) 2 × /d for 2 wk
0.05% fluocinonide gel
Place on affected area(s) 2 × /d for 2 wk
0.05% clobetasol gel
Swish and spit 10 mL 4 × /d for 2 wk
Dexamethasone elixir (0.5 mg/mL)
Intralesional injection
Triamcinolone acetonide 5 mg/mL
Dissolve in mouth 5 × /d for 10 d
Topical antifungal therapy, 10 mg
clotrimazole troches
Swish and spit 5 mL 4 × /day for 10 d
Nystatin suspension (100,000 U/mL)
Swish and spit 10 mL 2 × /day until lesions resolve
Chlorhexidine rinse (0.12%)
*Fungal infections are a side effect of topical steroids. †If lesions do not respond
appropriately to topical steroids in 2 weeks, consider systemic therapy such as
antimalarials, steroids, thalidomide, clofazimine, and methotrexate.
ts
Intra oral skin graf
Pieces of skin grafted into the oral mucosa usually to:
# Line a surgically deepened buccal sulcus
# Repair an oro-antral fistula

Dr. Ahmed Salih Khudhur
BDS, M.Sc., PhD. Newcastle University/UK
7
# Repair extensive traumatic oral wound
Such grafted tissue has been mistakenly identified as a white lesion. The
grayish white appearance depends on imbibition of fluid by the thick
stratum corneum. Normal keratinized oral mucosa does not exhibit this
phenomenon.
