Hypersensitivity reactions
ByDr Dhafer Alghezi
M.sc. , Ph. D. Clinical immunology ( Cancer research)
Introduction
The same immune reactions that protect us from infection can also inflict a great deal of damage to our own cells and tissues.The immune response uses multiple strategies to reduce damage to self by turning off responses once pathogen is cleared, and by avoiding reactions to self antigens.
However, these checks and balances can break down, leading to immune-mediated reactions that are more detrimental than protective.
Some immune-mediated disorders are caused by a failure of immune tolerance.
Others are caused by an inappropriately vigorous innate and/or adaptive response to antigens that pose little or no threat. These disorders, called hypersensitivitiesHypersensitivity
It refers to undesirable reactions produced by the normal immune system.There are multiple types of hypersensitivity reactions.
A) Immediate hypersensitivity reactions: result in symptoms that manifest themselves within very short time periods after the immune stimulus.
It results from antibody-antigen reaction.
B) Delayed-type hypersensitivity (DTH) reaction: take 1 to 3 days to manifest themselves.
DTH is caused by T-cell reactions.
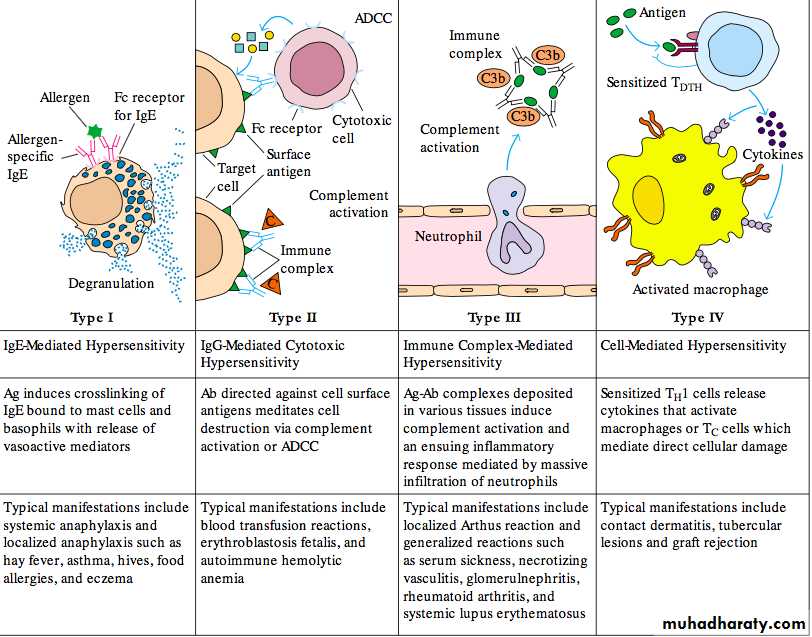
Hypersensitivities are classically divided into four categories (types I–IV) that differ by:
A) The immune molecules and cells that cause them.
B) the way they induce damage.
Hypersensitivity reactions (Type I)
Mediated by IgE antibodies that bind to mast cells or basophils and induce mediator release.These reactions include the most common responses to respiratory allergens, such as pollen and dust mites, and to food allergens, such as peanuts and shellfish.
Hypersensitivity reactions (Type II )
Result from the binding of IgG or IgM to the surface of host cells, which are then destroyed by complement- or cell-mediated mechanisms.For example, this is the fate for transfused red blood cells in transfusions between people differing in ABO blood types.
Hypersensitivity reactions (type III )
Antigen-antibody complexes (such as those generated by the injection of foreign serum proteins) deposited on host cells or tissues activate complement or the release of mediators from granulocytes, often causing inflammatory responses.hypersensitivity reactions (Type IV )
Result from excessive and sometimes inappropriate T-cell activation. Common examples are the skin reactions caused by poison oak or poison ivy.Allergies: Type I Hypersensitivity
Type I hypersensitivity reactions are mediated by IgE antibodies, and include the most common allergic reactions, such as allergic rhinitis (hay fever), asthma, atopic dermatitis (eczema), and food allergies.In normal individuals, the level of IgE in serum is the lowest of any of the immunoglobulin classes.
Individuals without allergies generate IgE antibodies only in response to parasitic infections.
Individuals who genetically are highly susceptible to allergies, a condition known as atopy, are predisposed to generate IgE antibodies against common environmental antigens.
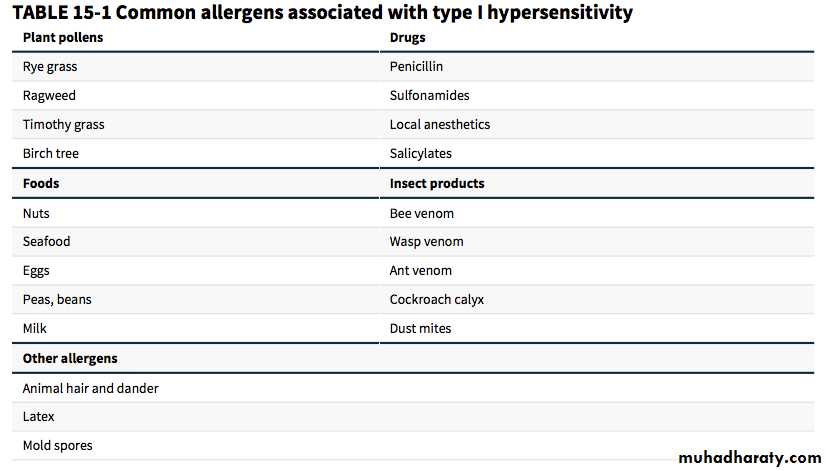
Recently, several features shared by many allergens have begun to provide clues to the biological basis of their activity.
First, many allergens have intrinsic enzymatic activity that contributes to the allergic response.
Allergens from dust mites (the allergenic component of house dust), cockroaches, pollen, fungi, and bacteria have protease activity.
Some of these proteases is capable of disrupting the integrity of epithelial cell junctions, allowing allergens to access the underlying cells and molecules of the innate and adaptive immune systems.
Others, including a protease (Der p 1) produced by the dust mite (Dermatophagoides pteronyssinus), cleave and activate complement components at the mucosal surface.
Still others cleave and stimulate protease-activated receptors on the surfaces of immune cells, enhancing inflammation.
Second, many allergens contain potential pathogen-associated molecular patterns, or PAMPS capable of interacting with receptors of the innate immune system and initiating a cascade of responses that contribute to an allergic response.
Third, many allergens enter the host via mucosal tissues at very low concentrations, which tend to induce TH2 responses. The IL-4 and IL-13 produced by TH2 cells induce heavy-chain class switching to IgE during the generation both of plasma cells secreting allergen-specific antibodies and of allergen-specific memory B cells
Key Concepts
Allergens are highly soluble proteins or glycoproteins, usually with multiple epitopes.Many allergens are proteases and/or contain PAMPs, which result in stimulation of the immune system.Some allergens activate TH2 cells, which induce heavy-chain class switching to IgE.
IgE Antibodies act by binding antigen, resulting in the Cross-Linking of Fc Receptors
IgE antibodies alone do not cause harmful responses.They cause hypersensitivity by binding to Fc receptors, called FcRIs , specific for their constant regions.
FcRIs are expressed by a variety of innate immune cells, including mast cells and basophils.
The binding of IgE antibodies to FcRI activates these granulocytes, inducing a signaling cascade that causes cells to release the contents of intracellular granules into the blood or tissue, a process called degranulation
The contents of granules vary from cell to cell, but typically include histamine, heparin, and proteases.
Together with other molecules (leukotrienes, prostaglandins, chemokines, and cytokines) that are synthesized by these activated granulocytes, these mediators act on surrounding tissues and other immune cells, causing allergy symptoms.
A second Fc receptor with lower affinity for IgE, FcRII, regulates the production of IgE by B cells.
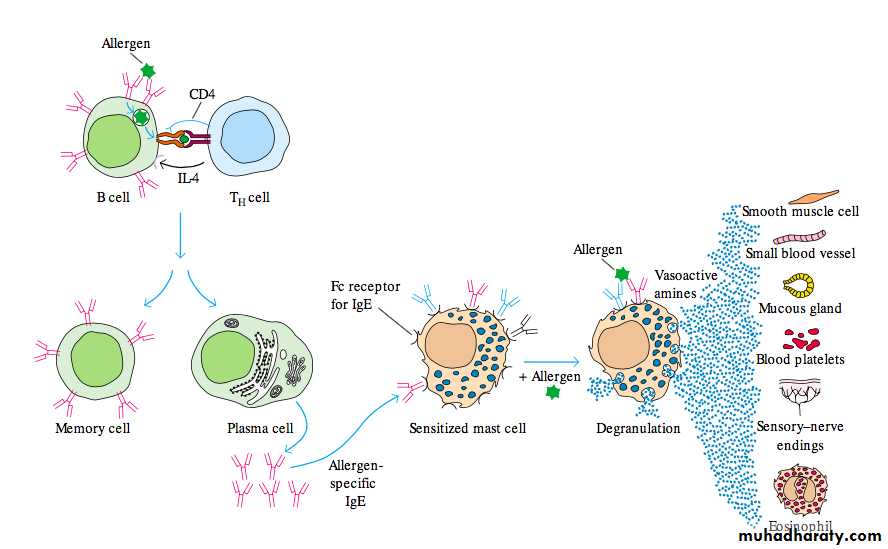
Pathogenic mechanisms
Three classes of mediators derived from mast cells:1) Preformed mediators stored in granules (histamine)
2) Newly sensitized mediators:
leukotrienes, prostaglandins, platelets activating factor
3) Cytokines produced by activated mast cells, basophils
e.g. TNF, IL3, IL-4, IL-5 IL-13, chemokines
* These mediators cause: smooth muscle contraction, mucous secretion and bronchial spasm, vasodilatation, vascular permeability and edema
General mechanism underlying an immediate type I hypersensitivity reaction. Exposure to an allergen activates TH2 cells that stimulate B cells to proliferate, undergo heavy-chain class switching to IgE, and differentiate into IgE-secreting plasma cells and memory B cells expressing membrane IgE B-cell receptors (mIgE). The secreted IgE molecules bind to IgE-specific Fc receptors (FcRI) on mast cells and blood basophils. A second exposure to the allergen leads to cross-linking of the bound IgE, triggering the release of pharmacologically active mediators from mast cells and basophils. The mediators cause numerous effects, including smooth muscle contraction, increased vascular permeability, and vasodilation.
FcRI signaling leads to several mast cell and basophil responses:
(1) Degranulation: the fusion of vesicles containing multiple inflammatory mediators with the plasma membrane and release of their contents(2) Synthesis of inflammatory cytokines.
(3) Conversion of arachidonic acid into leukotrienes and prostaglandins, two important lipid mediators of inflammation.
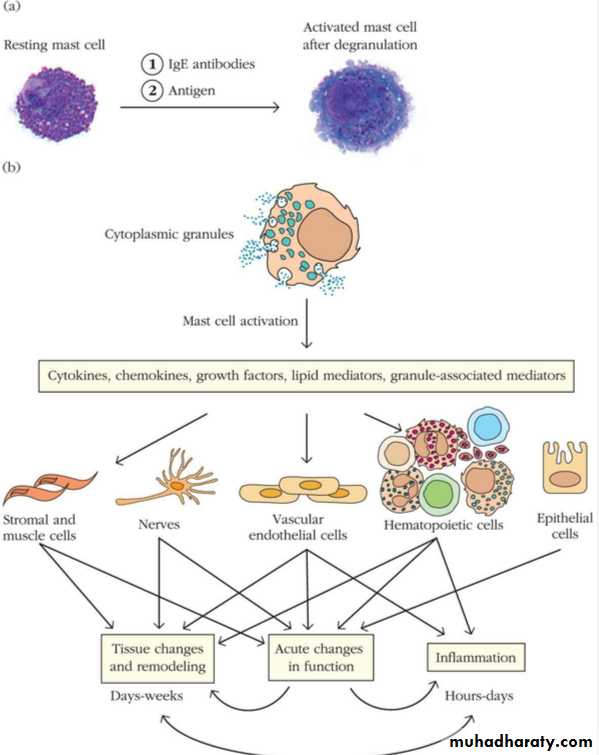
Figure effects of mast cell activation.
• Mast cells before (left) and after degranulation (right) induced by IgE antibodies and antigen that is bound by the antibodies. Resting mast cells have numerous granules (secretory vesicles) stored in their cytoplasm. After the mast cell is activated by addition of IgE antibodies (which bind to FcRI) and an antigen that cross-links the IgE antibodies, the granules fuse with the plasma membrane, releasing their contents. Extra membrane from the granules is seen in the cell’s plasma membrane after degranulation.• (b) Mast cell mediators and their effects. Various stimuli activate mast cells to secrete different types and/or amounts of products. Activated mast cells immediately release preformed, granule-associated inflammatory mediators (including histamine, proteases, and heparin) and are induced to generate lipid mediators (such as leukotrienes and prostaglandins), chemokines, cytokines, and growth factors (some of which can also be packaged in granules). These mediators act on different cell types, and have both acute and chronic effects. When produced over long periods of time, mast cell mediators have a significant influence on tissue structure by enhancing proliferation of fibroblasts and epithelial cells, increasing production and deposition of collagen and other connective tissue proteins, stimulating the generation of blood vessels, and more.
Anaphylaxis
* Systemic form of Type I hypersensitivity* Exposure to allergen to which a person is previously sensitized
* Allergens:
Drugs: penicillinSerum injection : anti-diphtheritic or ant-tetanic serum
anesthesia or insect venom
* Clinical picture:
Shock due to sudden decrease of blood pressure, respiratory distress due to bronchospasm, cyanosis, edema, urticaria
* Treatment: corticosteroids injection, epinephrine, antihistamines
Atopy* Local form of type I hypersensitivity
* Exposure to certain allergens that induce production of specific Ig E
* Allergens :
Inhalants: dust mite faeces, tree or pollens, mould spore.
Ingestants: milk, egg, fish, chocolate
Contactants: wool, nylon, animal fur
Drugs: penicillin, salicylates, anesthesia insect venom
* There is a strong familial predisposition to atopic allergy
* The predisposition is genetically determined
Methods of diagnosis
• 1) History taking for determining the allergen involved• 2) Skin tests:
• Intradermal injection of battery of different allergens
• A wheal and flare (erythema) develop at the site of
• allergen to which the person is allergic
• 3) Determination of total serum Ig E level
• 4) Determination of specific Ig E levels to the different allergens
Management
1) Avoidance of specific allergen responsible for condition2) Hyposensitization:
Injection gradually increasing doses of extract of allergen- production of Ig G blocking antibody which binds
allergen and prevent combination with Ig E
- It may induce T cell tolerance