Histology Thyroid gland dr. Ahmed Alhuchami
Thyroid gland
Embryologically, it is derived from the cephalic portion of the alimentary canal (endoderm)
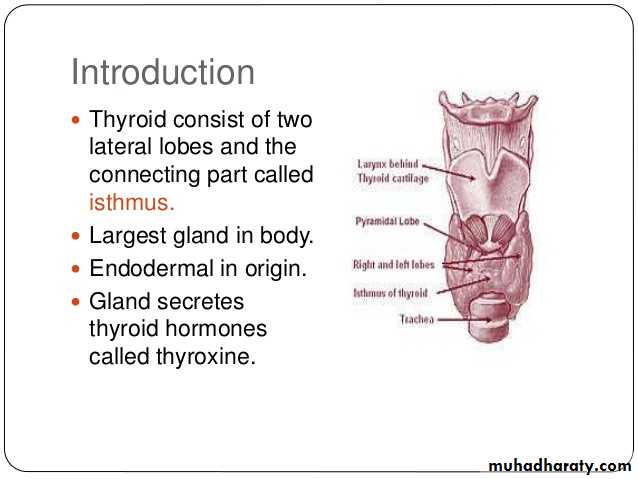
It is located in the cervical region, anterior to larynx and trachea
It has two lobes that are connected to each other’s by the isthmus
It is covered by connective tissue capsule
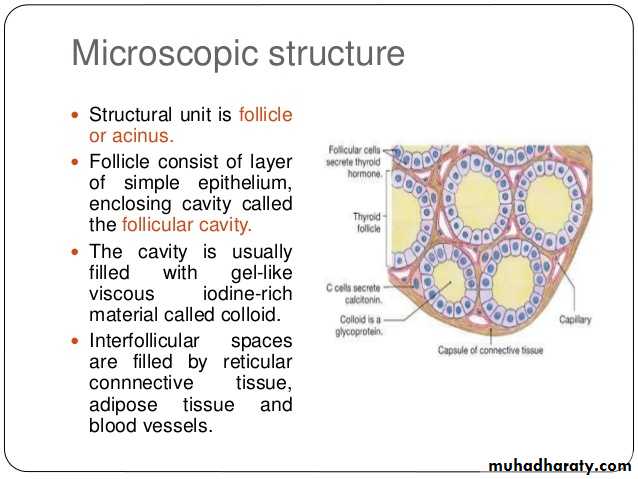
Thyroid gland section is composed of thyroid follicles that are filled with gelatinous substance called colloid.
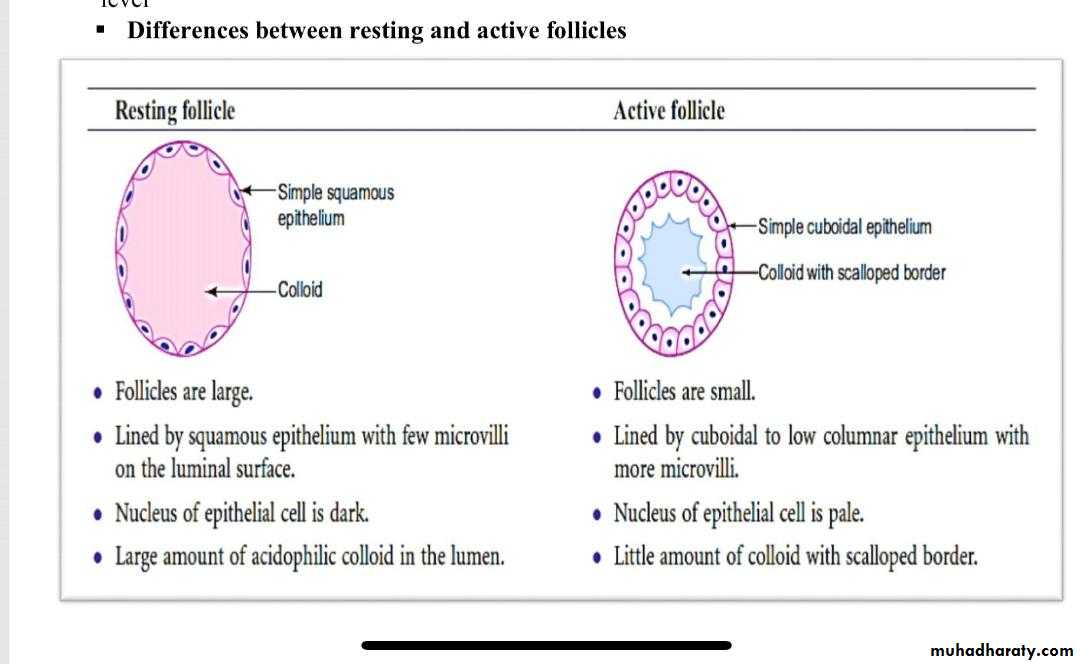
Follicular wall is composed of cells called follicular cells which range from squamous to low columnar epithelium, according to their secretory activity.
Follicular cells secret both Thyroxine (tetraiodothyronin) (T4) and triiodothyronin (T3)
Between follicles, there is loose connective tissue that contains Parafollicular cells (also called C-cells) which are large, pale, polyhedral cells that secret calcitonin (suppress bone resorption by osteoclasts. Calcitonin secretion is triggered by elevated blood Ca2+ levels).
MEDICAL APPLICATION
A diet low in iodide hinders the synthesis of thyroid hormones, causing increased secretion of TSH and compensatory growth of the thyroid gland, a condition known as iodine deficiency goiter. Goiters are endemic in some regions of the world, where dietary iodide is scarce and addition of iodide to table salt is not required.Parathyroid glands
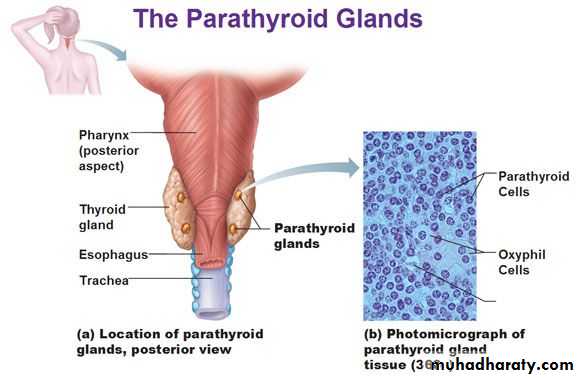
they are four small glands, their total weight = 0.4 gm (0.1 each) they lie within the capsule of thyroid gland one at each end of the upper and lower
poles
Embryologically, they are derived from pharyngeal pouches; the two superior parathyroid glands are derived from the fourth pouch, while the two inferiors from the third one. each parathyroid gland is covered by connective tissue capsule
Two types of cells are present in parathyroid glands: chief (or principal) cells and oxyphil cells. The chief cells are small polygonal cells with round nuclei and pale staining, slightly acidophilic cytoplasm. Ultrastructurally the cytoplasm is seen to be filled with irregularly shaped granules 200–400 nm in diameter. These are secretory granules containing the polypeptide parathyroid hormone (PTH), a major regulator of blood calcium levels.
oxyphil cells sometimes present, more commonly in older individuals. These are much larger than the principal cells and are characterized by acidophilic cytoplasm filled with abnormally shaped mitochondria. Some oxyphil cells show low levels of PTH synthesis, suggesting these cells are transitional derivatives from chief cells.
Parathyroid hormone targets osteoblasts, which respond by producing an osteoclast stimulating factor to increase the number and activity of osteoclasts. This promotes resorption of the calcified bone matrix and the release of Ca2+, increasing the concentration of Ca2+ in the blood, which suppresses parathyroid hormone production .Calcitonin from the thyroid gland inhibits osteoclast activity, lowering the blood Ca2+ concentration and promoting osteogenesis.