Communication skills
1\ 2\ 2021By Dr Muslim N.Saeed
4th stage
1
Learning Objectives
To discuss the basics of communication skills in clinical encounters.To discuss the management of difficult patients.
To discuss the steps for delivering bad news to patients.
2
Relevance of communication skills
3Why are Communication Skills Important?
Conducting a medical interview is a core clinical skill of doctors especially primary health care providers.Effective doctor-patient communication is directly linked to improved patient satisfaction, adherence, and health outcomes.
A good doctor-patient relationship is especially important in the management of chronic diseases.
Patients who are well-informed about their disease and involved in the decision making, are more adherent to the medical recommendations and willing/able to carry out more health – related behavior.
4
The Basics of Communication skills
5Basic Communication Skills in a Medical Encounter (1)
Preparing the stage: organizing the setting of the clinic, making sure that you have what you need for the encounter.The Opening: greeting the patient and engaging in informal discussion.
Asking: use open-ended questions to know the reason of presentation of the patient. Avoid leading and judgmental questions.
Clarification: this is used to clarify unclear information provided by the patient.
Facilitation: to encourage patients to proceed in telling their story. It can be both verbal (and then what…) or non-verbal (nodding your head) .
Reflection: use reflective statements on what patients said to encourage them to answer specially sensitive questions.
6
Basic Communication Skills in a Medical Encounter (2)
Confrontation: it helps to clarify information given by the patient. This includes for example asking for explanation to non-clear information, showing the contradictions in the messages of the patient.Summarizing: to summarize the information provided by the patient.
Preparing the patient for physical exam: need to explain to the patient about the content of the exam.
Congruence: to be genuine in dealing with the patient. Your verbal and non-verbal messages should not be contradictory.
Negotiation: this helps reaching common ground with the patient.
Closing: at the end of the encounter.
7
The Art of Communication
8Steps to Follow when Communicating with Patients
Focus on the PatientEstablish a connection with the patient
Assess the patient’s response to illness and suffering
Communicate to foster healing
Use the power of touch
Laugh a little
Show some empathy
9
Step 1- Focus on the Patient
Prepare for the encounter before the patient enters into your clinic. This will set the stage for what comes next.Make sure first that you are ready to receive the patient; your mind is set and free.
Check the patient medical record.
Get to know your patient: check previous encounters.
10
Step 2: Establish a Connection with the Patient
Use the first few minutes of the encounter to connect with the patient – short non-medical social interaction.Build a rapport with the patient. This can provide some clues to the patient’s emotional state.
**Rapport is a close and harmonious relationship in which the people understand each other's feelings or ideas and communicate well.
Set the agenda of the encounter with the patient: reason for coming, additional issues that the patient would like to discuss, agree on what can be done during this encounter and if there is a need to set another appointment for the remaining issues.
Setting the agenda with the patient will increase his/her satisfaction .
11
Step 3: Assess the Patient’s Response to Illness & Suffering
Assess how the patient is responding to his/her illness. This can uncover important clinical clues.Assess the suffering level of the patient, which can be both physical and psychological.
12
Step 4 – Communicate to Foster Healing
Include the following in your communication with the patient:Congruence : to be authentic.
Acceptance: show that you value the person that the patient is even if you do not agree with his/her actions.
Understanding : try to relate and be sensitive to what the patient is experiencing.
13
Step 5 – Use the Power of Touch
A warm handshake or a pat on the shoulder can help calm worried patients.
Make sure to be culturally sensitive.
14
Step 6 – Laugh a Little
Humor can be helpful sometimes in establishing rapport. Make sure that the patient accepts the humor well and does not lack a sense of humor.Humor can relieve anxiety , enhance healing, and decrease frustration.
15
Step 7 – Show Some Empathy
Empathy is an important part of communication.It is important as well that you express your understanding of the situation of the patient. This would encourage sharing by the patient of more personal and clinical information that would help in his/her management.
16
Patient-centered medical interviewing
17Patient-Centered Approach
Patient-centered care is an essential element of high quality care.Patient-centered approach has three main goals:
To elicit the patient’s perspective on the illness
To understand the patient’s psychosocial context
To reach shared treatment goals based on the patient’s values.
18
Sequence of Patient-Centered Medical Interviewing
Introduce and build rapport
Elicit the patient’s agenda
List all of the patient’s agenda items
Negotiate the agenda
Start discussing the patient’s concerns with open-ended questions
Ask direct questions to elicit details about the chief concern, and perform a review of systems
Elicit the patient’s perspective
Empathize
Summarize
Transition
19
Difficult Encounters
20Difficult Encounters
Difficult encounters account for around 15% to 30% of visits to family doctors.Disparity between the expectations, perceptions or actions of patient and doctor characterizes difficult encounters.
Doctors who have most difficulty with patient relationships are more likely to report job dissatisfaction and burnout symptoms.
Different factors interplay and might result in difficult encounters. These are classifies as doctors- related factors, patients-related factors, situation-related factors or a combination.
21
Doctors- Related Factors
Every doctor brings to each patient encounter his/her background, personality and experience.
Examples of encounters that can put the doctors on alert include the following:
Patients asking doctors for specific tests/treatments after searching the Internet --- might surprise or threaten the doctor.
Patients presenting with recurrent symptoms related to lifestyle factors despite receiving adequate counseling --- might lead the doctor to question his/her ability to influence behavior change.
22
Doctors- Related Factors
AttitudesConditions
Knowledge
Skills
- Emotional burnout
- Insecurity
- Intolerance of diagnostic uncertainty
- Negative bias toward specific health conditions
- Perceived time pressure
- Anxiety / depression
- Exhaustion/ overworked- Personal health issues
- Situational stressors
- Sleep deprivation
- Inadequate training in psychosocial medicine
- Limited knowledge of the patient’s health condition
- Difficulty expressing empathy
- Easily frustrated
- Poor communication skills
23
Patients- Related Factors
Behavioral issuesConditions
Psychiatric Disorders
- Angry/argumentative/rude
- Demanding/entitled
- Drug-seeking behavior
- Highly anxious
- Hyper vigilance to body sensations
- Manipulative
- Manner in which patient seeks medical care
- Non-adherence to treatment for chronic medical conditions
- Not in control of negative emotions
- Reluctance to take responsibility for his or her health
- Self-saboteur
- Addiction to alcohol or drugs
- Belief systems foreign to physician’s frame of reference
- Chronic pain syndromes
- Conflict between patient’s and physician’s goals for the visit
- Financial constraints causing difficulty with therapy adherence
- Functional somatic disorders
- Low literacy
- Multiple (more than four) medical issues per visit
- Physical, emotional, or mental abuse
- Borderline personality disorder
- Dependent personality disorder
- Underlying mood disorder
24
Situation-Related Factors
Prioritizing patho-physiological complaints rather than addressing psychological needs of patients as a result of condensed clinic schedules.Easy access of patients to health information (internet for example), triggering several questions from patients with an increased need to more in-depth discussions.
25
Management of Difficult Encounters
Doctors play a crucial role in the management of difficult encounters. Doctors need:To avoid prejudging and to acknowledge that the symptoms of the patients are valid.
To conduct a thorough assessment of the patients' distress. Undiagnosed and untreated psychopathologies can be common in difficult patients. History of abuse, difficult family or social situations can be detected as well.
To be empathetic. Empathy helps them suspend judgment and ensure that they are perceived as healers and allies rather than just service providers.
To follow the principles of effective communication.
26
Breaking Bad News
27
What is “Bad News”?
The term “Bad news” is defined as "any information likely to alter drastically a patient's view of his or her future…" or that "…results in a cognitive, behavioral, or emotional deficit in the person receiving the news that persists for some time after the news is received“.The definition depends heavily on the patient’s beliefs and perceptions.
Family doctors encounter many situations that involve breaking bad news: telling a young man that he has a sexually transmitted infection, telling a middle-aged woman that her magnetic resonance image raises the possibility of multiple sclerosis, telling the parents of a child that the symptoms of polydipsia and weight loss suggest diabetes mellitus.
28
Relevance to Family Doctors
It is crucial for family doctors to know the basics of breaking bad news.Evidence shows that the attitude, communication skills and empathy of doctor while delivering the bad news plays an important role in the coping and bereavement abilities of patients and their families.
The specialty of Family Medicine emphasizes the importance of understanding the psychosocial context of patients’ lives, and the trusting relationships that doctors develop with their patients over the years. This helps in determining the best way to deliver bad news and to predict how bad news can be accepted.
29
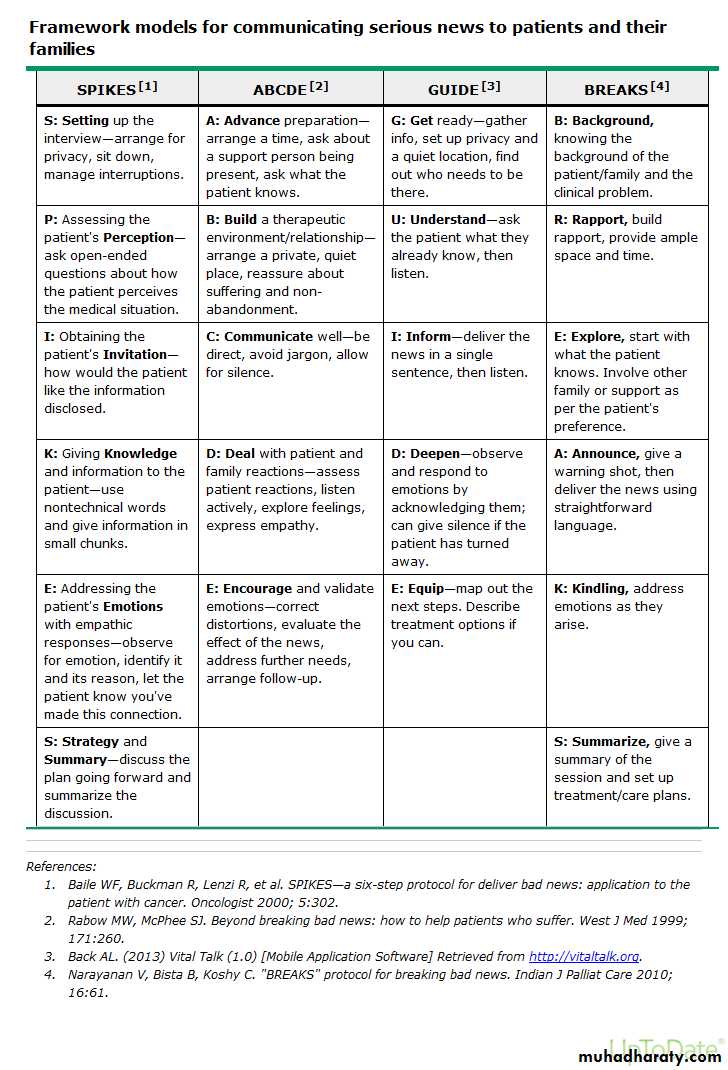
Frameworks for Breaking Bad News
Different Frameworks cited in the literature:SPIKES
ABCDE
GUIDE
BREAKS
30
Summary of the Steps
Preparation and SettingPerception: Asking the patient/family what they understand or perceive
Sharing the “bad news” itself
Attending to emotions as they arise
Planning and discussing next steps
32
Preparation and Setting
Secure a private and quiet setting.Avoid interruptions.
Make sure to allocate enough time for the discussion.
Ask the patient who he/she would like to be present during the discussion.
33
Perception: Asking the Patient/Family what they Understand or Perceive
Ask the patient/family what they already know about his/her condition.This helps the doctor to build on what the patient/family know and fill in the gaps.
Use active listening techniques such as leaning in, eye contact, open posture.
34
Sharing the Bad News Itself
Can start with giving a “warning shot” such as “I am sorry, I have some bad news”.
Use simple and direct language. Avoid medical jargon.
Keep the news brief; provide information in small chunks allowing time for the patient/family to understand.
After delivering the information, pause and give time to patient/family to process this information. This might be a period of 10 seconds of silence or more.
Avoid being blunt or insensitive while delivering the news.
35
Attending to Emotions as They Arise
Expect the emotional response of the patient/family to the news.Be quiet and listen. Try not to break the silence unless it is taking too long. It can help then to ask the patient/family “what is it like for you to hear this news?”, helping them to begin processing the news.
It is important to give the patient/family a “realistic hope” and avoid any false hope.
Be empathetic in dealing with strong emotions (use the NURSE acronym).
36
NURSE Acronym for Dealing with Strong Emotions
AcronymRequest
Example
N
Name
It sounds like you are frustrated
U
Understanding
I cannot imagine what it would be like to be in this situation
R
Respect
You are asking all the right questions and doing an amazing job of being an advocate for your husband
S
Support
I will be around to answer any of your questions
E
Explore
Tell me more about what you are thinking
37
Planning and Discussing Next Steps
Discuss the plan with the patient/family. Discuss follow up appointments, upcoming tests, referrals to other specialists etc.
Guide the patient/family in this new journey.
Check if the patient/family have any other questions.
38
Important Note to Doctors
Delivering bad news can be tough on doctors as well.Issues of counter-transference can develop, which might trigger poorly understood feelings.
It is important to seek support or advice as needed. A formal or informal debriefing session can be of help.
39