Reproductive health
Dr. Muslim N. SaeedFamily & Community Medicine DepartmentFeb. 3th ,2021 / online
Adolescence health
Objectives:by the end of this lecture, you’ll be able to:
1.Define adolescence period & its stages.
2.Understand Adolescence preventive services: screening, lab tests, immunization.
3.Understand proper ANC guidelines.
4.Identify high risk pregnancy.
5.Know proper preventive measures for pregnancy complications.
Definition
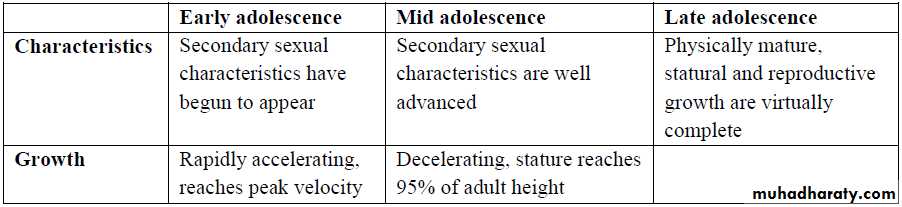
-Adolescence is a time of a physical, emotional, mental & psychosocial changes.*Stages of adolescence:
1- Early adolescence: 11-13 years of age &merges with mid adolescence at14-15 years. characterized by concrete thinking & body image disruption.
2- Mid adolescence: 14-15 years of age till 17 years, involves autonomy may lead to parental conflict.
3- Late adolescence: 17-21yr.the upper end is particularly variable & depends on cultural, economic,& educational factors. adolescents begin to think about the future & form stable intimate relationship.
Guideline of adolescence preventive services:
A series of recommendations regarding the delivery of health services ,promotion of well-being, screening for common conditions ,& provision of immunization for adolescents & young adults includes:• Annual health visits: (3 complete physical examinations, one at each stage).
• Counseling for both parents & adolescent.
• Screening
Adolescence preventive services:
A) Routine screening:• Hypertension (measuring Bp)
• Hearing ( conduct objective test at 12-15-18 yr.)
• Visual acuity (Snellen’s test)
• High risk or symptomatic adolescents( TB. ,anemia , cholesterol)
• eating disorder & obesity (BMI)
• Use of tobacco , alcohol & other abusable substances
B) Laboratory test:
In the asymptomatic teenager, screening lab. tests should be kept at a minimum.• Hb or Hematocrit : anemia screening is recommended at the end of puberty.
• Lipid profile.
• Sexually active adolescents :
- Males: gonorrhea, Chlamydia, annual syphilis serology, HBV (homosexual).
- Female: Pap smear starting at age 21 in vulnerable groups.
C) Immunization:
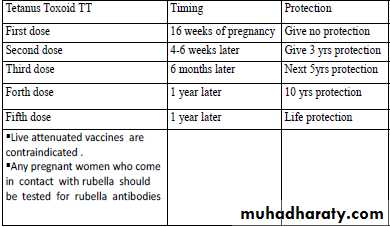
• Diphtheria, tetanus: a booster of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) is recommended 10 years after the initial dose.
• Meningococcal conjugate vaccine: administer to unvaccinated adolescents at high school entry (15y).
• Influenza vaccine.
• Hepatitis A and B: if not received during childhood.
• Pneumococcal vaccine: for adolescents with chronic illnesses (HIV, B-cell immune deficiency) and those with cardiovascular and pulmonary disease.
• HPV vaccine: all females 11-12 years of age should receive the 3 dose series
• Rubella: unimmunized females.
Maternal & Child health servicesMCH services
Maternal & Child Heath (MCH) (including family planning):MCH Definition:
It is that aspect of health which is concerned with the special needs & problems of mother & child.
-It includes care for pregnant women and family planning, growth monitoring and development of infant and children.
-Mothers and children are both vulnerable groups of the community.
Women in the childbearing period (15-49 years) constitute about 25% of the population.
-Children on the other hand constitute about 40% to 45% of the population in developing countries. This group is characterized by relative high mortality and morbidity rates.
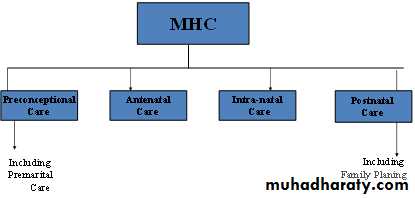
MCH includes: 1- Maternal care. 2- Child care 3- Family planning
Importance of MCH services:
• Most of the problems of MCH are preventable.• Provide services to about two third of population.
• Improve socioeconomic development.
• Mother & children are high risk group; they are vulnerable group with special needs.
• Good site for training and health education.
• Important for future of the nations, since mothers are responsible for health promotion and culture of children and family welfare.
Maternal Health Care
Phases of maternal care:
• Pre-conception care: It is continued care for female, through all stages of growth and development, & until the time of conception (It is care of women before pregnancy).• Premarital Care:
Health care given to men and women before they get married and is an essential part of adolescent health care. It include:
a) Health education concerning:
Proper nutrition, Healthy lifestyle, Safe sex, sexually transmitted diseases.
b) History taking: regarding hereditary diseases.
c) Physical examination: for evaluation of health status and nutritional status, and screening of suspected cases.
d) Investigation includes:
-Blood for: ABO group &RH, Hb% level, VDRL, HIV test, test for hepatitis.
-Chest X ray: to exclude pulmonary T.B.
e) Preventive services (immunization): Rubella vaccine is important before the female become pregnant (pregnancy should be avoided for the next 3 months after vaccination).
f) Counseling: Genetic counseling, family planning counseling (if requested by couples).
• III. Antenatal Care ( prenatal care ) ANC:
is complete health supervision of the pregnant women in order to maintain, promote & protect health & wellbeing of the mother, fetus and the newborn infant.General objectives of antenatal care:
“The general objective of ANC is to prepare the mother both physically and psychologically to give birth to a healthy newborn and to be able to care for it.”
When the Antenatal care started?
Antenatal care started as soon as pregnancy is confirmed
Confirmation of pregnancy:
-History of missed period in otherwise normal cycle
-Symptoms of pregnancy: nausea, vomiting heartburn, hyperacidity.
-pregnancy test.
Standards of ANC: (initial visit and subsequent visits)
The initial visit (first visit) :The first antenatal visit should take place as early as possible during the first trimester , as soon as the pregnancy is confirmed.
The initial visit should include:
1. Booking procedures (registration).
2. Physical examination.
3. Investigation.
4. Health education.
Instructions: including frequency of visits
Registration (Booking):
When primi-gravida visits MCH center for the first time a health record [file with serial number] is initiated to register all events concerning present pregnancy & it`s outcome .
o Importance of record - keeping:
1. To be used as reference data in next pregnancies
2. For collection of statistical data used as health indicator for assessment & evaluation of MCH services.
-History: (personal, family, medical, drug , allergy, blood transfusion., surgical, menstrual, obstetrical )
-EDD is calculated accordingly , use of contraception , if she is lactating now.
Obstetrical history: history of all previous pregnancies in chronological order.
2) Physical examination: general and systemic.Abdominal (Obstetric) examination, pelvic exam.
3) Investigations:
1-Blood analysis: complete blood picture.
- ABO grouping & Rh.
- Screening for diabetes, RBS, 2HPP (2 hours post prandial), GTT if needed.
- VDRL
2-Urine analysis : GUE for albumin urea , microscopic examination for bacteriurea & pus cell . culture & sensitivity (C&S) if recommended
-Arrange for pelvic ultrasound: if the women is not sure of gestational age or if her period is not reliable .
Schedule of antenatal care visits:
For low – risk pregnancy the following schedule of visits should be followed:-up to 28 weeks gestation every 4 weeks
-28 – 36 weeks gestation every 2 weeks
-After 36 weeks gestation every one week
In a low–risk pregnancy with no complication , a minimum number of antenatal visits is five visits, including the booking visit, is acceptable.
-The quality of care is more important than the frequency of visits.
At- Risk approach in ANC
This approach provides care for those who need it in a flexible but more skilled care is given to those at higher risk .
Objectives of At – risk approach in antenatal care :
1) Early detection of risk factors during pregnancy .
2) Scoring of detected risks and hazards to classify At – Risk cases (high – risk groups) that need either:
o Just more care and follow up observation, for progress and early interference when necessary .
o Referral for specialized investigations and or management .
o In – patient care , and hospital delivery .
High – risk pregnancy
The term "high-risk pregnancy" describes a case where a pregnant woman has one or more factors that could put her or the fetus at risk for health problems.The following are five risk categories associated with a high risk pregnancy :
1- Personal & menstrual history .
2- Obstetrical history .
3- Past history ( medical & or surgical )
4- Family history .
5- Current conditions .
Major Risk Factors with High- Risk pregnancy:
1) Personal & menstrual history Age less than 18 years (15years).
Age more than 35 years.
Lives far from hospital facility.
Positive consanguinity.
Smoking.
Long duration of marriage with infertility & use of ovulation induction.
Unknown LMP.
2) Obstetrical history:
Parity ≥ 5.
No spacing. Previous IUFD or neonatal death.
Previous small for gestational age(SGA) or (LGA).
Previous congenital anomalies.
Recurrent first trimester abortion.
Previous hypertensive disorders.
Previous circulage or C/S delivery
gone into premature labor or had a premature baby
has had a baby with a birth defect, especially heart or genetic problems.
3) Past history
Hypertension, Heart disease, diabetes, lupus, asthma, a seizure disorder, or another longstanding medical problem. Previous blood transfusion
Previous Rh iso immunization or hydrops-fetalis
4) Family history
Twin or multiple pregnancy of mother & sister.
Diabetes mellitus (D.M)
5) Current condition:
• Maternal weight ˃ 90 kg (obesity ) or ˂ 45 kg .
• Maternal stature ≤ 150 cm.• Excessive weight gain: > 2 kg first trimester, > 7 kg second trimester, > 4 kg third trimester .
• Color : pallor, Jaundice.
• Blood pressure ≥ 140 / 90 mm Hg.
• Excessive amniotic fluid.
• Heamoglobin < 11 gm / dI.
• Rh negative.
• Vaginal bleeding in early pregnancy.
• Third trimester vaginal bleeding.
• Rubella exposure.
Periodic visits (subsequent visits):
-At each visit the following procedures & examination should be performed : History:
- Record new complaints
- Ask about alarming signs.
Examination:
- General: (Weight, Blood pressure, Edema of lower limbs.)
- Abdominal: (Fundal height (fundal level), Fetal lie (longitudinal, transverse, oblique), Fetal presentation (cephalic, breech), FH (fetal heart).
Laboratory investigation:
- screening for diabetes at 28 week of pregnancy .
- Urine examination for protein , glucose & ketones
Hb% & PCV
Immunization: tetanus toxoid (TT ) is needed to prevent tetanus neonatorum.
Health education.
Alarming Symptoms & Signs:
-Pregnant women should be advised to seek immediate medical care if they experience any of the following symptoms or signs
Vaginal bleeding or discharge, Sever edema.
Abnormal gain or loss of weight, Decrease or cessation of fetal movement .
Severe, persistent or recurrent headache, Visual disturbance (blurred vision)
Epigastric pain, Fever, Respiratory discomfort or dyspnea & Convulsion.
The following Schedule is used in Iraq:
Natal Care
Natal Care: is the care provided to pregnant women during labor.Objective of natal care
Helping the pregnant women to have normal delivery .
Providing emergency service when needed .
Care of baby at birth.
Place of delivery:
-Home delivery: if deliveries expected to be normal , can be carried at home by birth attendant.
-Hospital delivery: Developed countries prefer hospital delivery of all pregnant , in developing countries , it is limited to :
-Pregnant who desire it.
-When high risk labor is expected
-When difficulty arises during home delivery .
Postnatal Care
Care of mother after delivery. it is for 6weeks after delivery (puerperium period).
Usually done at the health center or home visit
First examination: 2-3weeks after delivery.
Second examination: 4-6weeks after delivery.
Aim: to detect &cure minor problems result from birth.
- Its components are:
o Postpartum examination
o Medical care
o Follow up
o Health education
o Family planning services
o Psychological and social support
- In postpartum exam., the mother is examined for:
General condition. Body Temperature , any rise of body Temp. by 1C° or more should be investigated.
Breast & nipple and whether lactation is practiced
Abdomen for involution of uterus.
Bleeding or discharge .
Any other complaint.
Follow up: mother is examined on periodic visits to MCH center :
At the end of 3rd week maximum to check:
- General condition: if anemic ferrous sulfate is given.
- Supplementation of Vit A ( 200,000 IUs ).
- If she had puerperal infection and if she had managed properly.
Six weeks after delivery to check :
- Measurement of weight & Bp.
- abdominal & pelvic examination is performed to check for the involution of uterus and repair of tears if any.
- Assessment of the women's mental health is performed .
Health education:
- Adequate nutrition for lactating mother .- Child feeding , ensuring breast feeding , and practices of weaning .
- Dietary supplementation .
- Child care in health & disease.
- Physical exercise and it`s value (pelvic floor exercise).
- Postpartum birth control .