• Child health servicesExpanded Program on Immunization
• Dr. Muslim N. SaeedFamily & Community Medicine Dept.• Fab 10th ,2021
• Expanded Program of Immunization (EPI)
• -Four to five million annual deaths could be prevented by 2015 through sustained and appropriate immunization efforts, backed by financial support.• -Vaccination is one of the most successful and cost-effective public health interventions.
• -Immunization: is the process whereby a person is made immune or resistant to an infectious disease, typically by the administration of a vaccine.
• -Vaccines stimulate the body’s own immune system to protect the person against subsequent infection or disease.
• -WHO recognized this more than three decades ago when they chose six diseases — tuberculosis, diphtheria, neonatal tetanus, whooping cough, poliomyelitis and measles — as the targets for an initiative called the Expanded Program on Immunization (EPI).
• Routine immunization is the basis of the EPI activities.
• -On a regular basis vaccines for measles, rubella, diphtheria, pertussis, tetanus, polio, hepatitis B and tuberculosis, are provided in health facilities all over the country. Vaccinations are given in static, out-reach and mobile health facilities.• -EPI was introduced & many countries adopted this program, among which Iraq since 1985. Through the application of EPI around the world, millions of death had been prevented . poliomyelitis is about to be eradicated, about two third of the developing countries have succeeded in eliminating neonatal tetanus.
• Objectives of EPI
• 1. Reduction in the morbidity and transmission of vaccine preventable diseases, such as pertussis , measles, hepatitis B.• 2. Reduction in mortality from vaccine preventable diseases.
• 3. Elimination and Eradication of certain diseases, such as smallpox, polio.
• 4. Improvement in national economy – less health care cost caring for sick children, less time off work of parents.
• Strategy of EPI
• 1. Provision of effective, safe and potent vaccines to the target population.
• 2. Universal accessibility & use of routine vaccination services through MOH/PHC Centers.
• 3. Improvement of vaccination services through:
• Training - Cold chain system - Introduction of new vaccines - Ensure adequate and reliable financing - Strengthening surveillance of target diseases.
• Low immunization rate
• -Low immunization rate and outbreaks of diseases cause a serious threat to non immune. children and adults in all countries worldwide.• -Rapid growth in international travel & mass population movement have increased potential for diseases to spread, not just across the national borders but to other countries as well.
• Causes of low immunization rate
• Many countries were unable to ensure adequate supplies of vaccines. They could not afford a cost of establishing the safe and efficient vaccine delivery system.• In developing countries, many children are still without immunization because they are living in remote area or they cannot reach the health services.
• Immunization drop-out rate is highest among poorest population who may fail to complete the full immunization schedule due to limited access or irregular provision of health services
• National Immunization Schedule/Iraq:
• - It is a recommended series of vaccination including the suggested timing of all doses.• - It including vaccines given over the child’s first year and tetanus vaccination is given to women of childbearing age.
• National Immunization schedule in Iraq
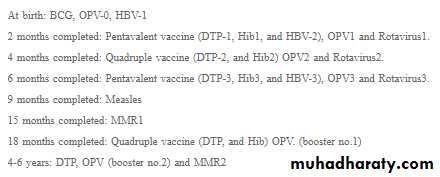
• National Immunization Schedule/Iraq: after 2011 before 2011
• Child Age Vaccine• -End of 1st week ------BCG+OPV0+HBV1
• -End of 2nd month-----DPT1+OPV1+HBV2
• -End of 4th month-------DPT2+OPV2
• -End of 6th month-------DPT3+OPV3+HBV3
• -End of 9th month------ Measles
• -End of 15th month--------MMR
• -End of 18th month------DPT+OPV (1st booster)
• -School entry (4-6) years ----DPT+OPV (2nd booster)
• -MMR= measles, mumps, rubella. -OPV= oral polio vaccine
• Forms of immunization
• 1-Active immunization:• Development of sensitized lymphocytes and active antibodies by giving
• immunogenic material from organism (viral/bacterial protein, killed viral particles,
• or changed virus/bacterial particles). Protects for many years. Ex: injectable polio
• vaccine.
• A- Live virus immunization:
• Uses live, but modified, non-pathogenic (live attenuated virus/bacterial particles).
• Generally must be refrigerated to preserve potency. Examples – oral polio, measles.
• B-Toxoid immunization:
• Uses modified version of toxin that causes disease. Examples – tetanus, diphtheria.
• 2- Passive immunization:
• Giving preformed antibodies, from animal or human origin
• Protects for short period, usually months only. Examples – gamma globulin for hepatitis or measles protection, tetanus immune globulin, rabies immune globulin.
• -0r using Biosynthetic vaccines: (such as Hib /H influenza B) contain synthetic substances.
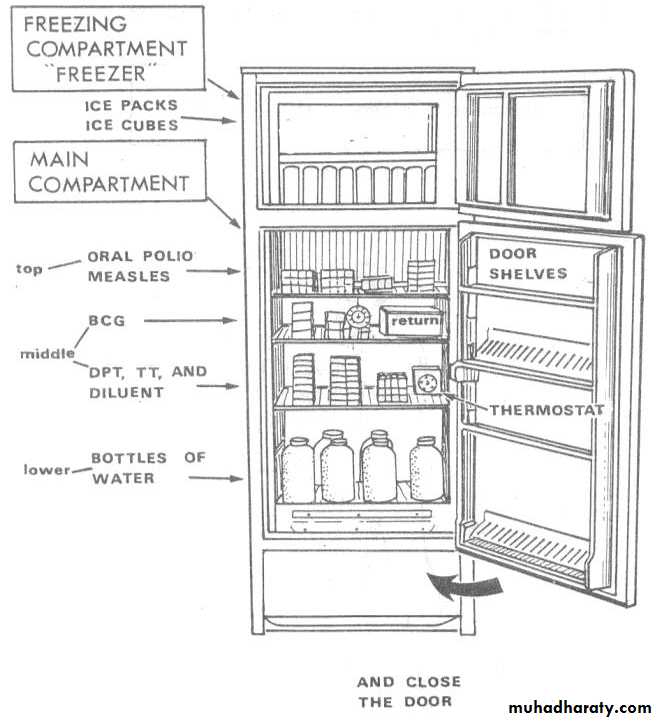
• Vaccine Handling & Storage (Cold Chain)
• “Cold Chain” is the system of transporting and storing vaccines. It refers to the process used to maintain optimal conditions during the transport, storage & handling of vaccines, starting at the manufacturer & ending with the administration of the vaccine to the client.• The optimum temperature for refrigerated vaccines is between +2°C and +8°C. For frozen vaccines the optimum temperature is -15°C or lower. In addition, protection from light is a necessary condition for some vaccines.
• Chain Management:
• Anyone handling vaccines is responsible for their potency, at each step in transport, storage and administration of vaccines.• Vaccines are delicate biological substances that can become less effective or destroyed if they are Frozen, Allowed to get too hot, Exposed to direct sunlight or fluorescent light.
• Vaccines should be maintained within the recommended temperature range.
• The optimum temperature for refrigerated vaccines is between +2°& +8°C .
• For frozen vaccines the optimum temperature is -15°C or lower.
• In addition, protection from light is a necessary condition for some vaccines.
• Importance of Maintaining the Cold Chain
• Vaccines are sensitive biological products which may become less effective, or even destroyed, when exposed to temperatures outside the recommended range.• Cold-sensitive vaccines experience an immediate loss of potency following freezing.
• Vaccines exposed to temperatures above the recommended temperature range experience some loss of potency with each episode of exposure.
• Repetitive exposure to heat episodes results in a cumulative loss of potency that is not reversible.
• Maintaining the potency of vaccines is important for several reasons:
• 1. Vaccine failures caused by administration of compromised vaccine may result in the re-emergence or occurrence of vaccine preventable disease.
• 2. Vaccines are expensive and can be in short supply resulting in lost opportunities to immunize.
• 3. Revaccination of people who have received an ineffective vaccine may cause a loss of public confidence in vaccines & the health care system.
• Temperatures falling outside the recommended range require immediate action to avoid loss of product.
• The cold chain (vaccine preservation): Many equipments are needed in transfer& storage of vaccines like freezers, refrigerators, cool boxes, vaccine carriers, cold rooms & thermometers
• Methods used to detect heat exposure;
• 1. Cold chain monitor; (CCM): a card with special color index is supplied with each vaccine pack, if the color changes to a certain degree it means that the vaccine is exposed to higher temp. than allowed and this vaccine pack must not be used.• 2. Vaccine viral monitor (VVM); a sticker present on the vaccine vial with two lines, purple and white, when the vaccine is exposed to heat the white line become purple too, this vaccine must be discarded.
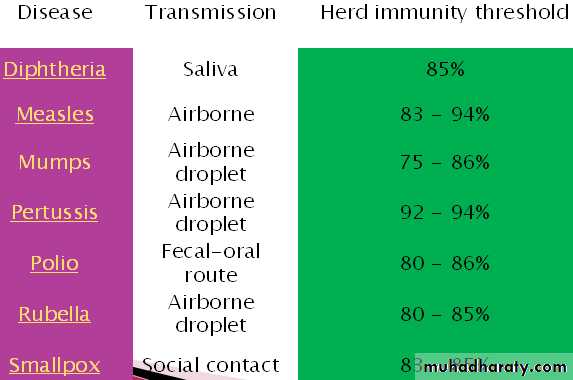
• Herd immunity
• -If the vast majority of the population is immune to a particular agent, the ability of that pathogen to infect another host is reduced; the cycle of transmission is interrupted, and the pathogen cannot reproduce and dies out.• -This concept, called community immunity or herd immunity, is
• important to disease eradication because if the number of susceptible individuals can be reduced to a small number through vaccination, the pathogen itself can also be eliminated.
• BCG vaccine
• Protects against tuberculosis, primarily in children• Given by intradermal injection in arm at the insertion of the deltoid. usually produces an inflammatory reaction and small scar
• 60 – 80% effective in preventing TB in infants, but protection decreases significantly after 2-3 years. Much less effective in adults.
• Adverse effects: local reaction of inflammation - regional lymphadenopathy
• Contra- indications:
• o Premature and low birth weight infants, so given later when infants discharged from neonatal care unit and his weight is 2500 gm.
• o Baby with immune deficiency.
• o Sever intractable diseases like septicemia & RDS.
• o Neonatal jaundice is not a contraindication for vaccination.
• Triple Vaccine – DPT
• Protects against diptheria, tetanus & pertussis.• Require minimum of 3 doses & 1 booster for full immunization
• Adverse effects: - Fever and malaise - Swelling at injection site
• - Severe problems closely following DPT immunization happen very rarely. These include a serious allergic reaction, prolonged seizures, a decrease in consciousness.
• - Most of the reactions to DPT injection are thought to be from the pertussis component.
• Contra-indications: Acute febrile illness. , Disease of the nervous system. , Severe reaction to a previous dose. DT given instead.
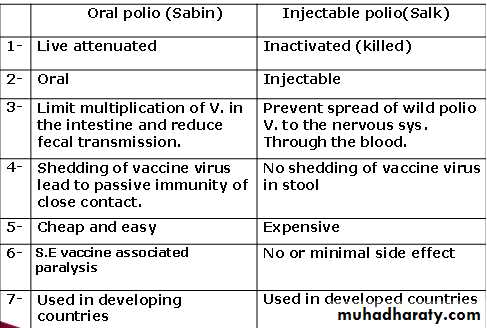
• Oral Polio:
• Protects against polio, which is a viral infection, begins in GI tract, that eventually lead to permanent damage to long nerves of the body and complete or partial paralysis.• Live, attenuated (weakened) virus in vaccine.
• Requires minimum of three doses and one booster for maximum public immunity
• Provides “herd” immunity within a community.
• Given by oral administration.
• Adverse effects - very rare incidence of vaccine-related
• polio (<1 per million children).
• Contrindications: Acute fébrile illness, Immunosuppression
• MMR (Measles, Mumps, Rubella) vaccine:
• Live attenuated, freeze dried, given by subcutaneous injection over the deltoid muscle at age of 15 months, it boosters immunity against measles and gives long lasting immunity against mumps and German measles infections.• Rubella vaccine:
• Live attenuated freeze dried vaccine given to female at child bearing age subcutaneous injection, give long lasting immunity against German measles, given to girls below age of 15 years, contraindicated during pregnancy or females intend to be pregnant.
• Hepatitis B Vaccine:
• Protects against hepatitis B, but not against other forms of hepatitis (A, C, D).• Requires total of 3 doses, first two one – two months apart, and 3rd at least 4 months later. I.M injection
• Protection is usually lifelong.
• Vaccine should be given to children in all countries with high or intermediate prevalence
• like Iraq. In countries with low prevalence it should be given only to high risk groups.
• Adverse effects: Mild fever and soreness at injection site.
• Tetanus Toxoid for pregnant women:
• Protects against tetanus of newborn child (called in some countries the “7th Day Disease” because many children died at one week of age with neonatal tetanus).• Primary goal is to increase level of anti-tetanus antibody in mother, which is then passively transferred to the fetus through placenta.
• If mother never immunized against tetanus, must receive at least 2 doses (0.5 ml of tetanus toxoid) during pregnancy (beginning with 4th month of pregnancy), with subsequent doses after delivery.
• With previous tetanus immunizations, give single booster dose with each pregnancy.
• No known adverse effect of tetanus toxoid on developing fetus.
• Haemophilus influenzae type B vaccine (Hib)
• Developed for the prevention of invasive disease caused by H. influenzae type b bacteria.
• Vaccinations against (Hib) have decreased early childhood meningitis significantly in developed countries and recently in developing countries.
• Influenza vaccine:
• o Protects against currently circulating strain of influenza A and/or B.
• o Is a killed virus vaccine, not live.
• o Because strain of influenza changes from year to year, vaccine must be reformulated each year, Usually given at start of “flu season” in October (northern hemisphere).
• Postponing vaccination to later time:
• Moderate illness with fever >38• Current high dose use of oral or injected corticosteroids
• Conditions which are NOT contraindications to immunization:
• Minor illness (URI) with fever < 38.5 - Asthma, respiratory allergies
• Prematurity (>1500 gm) – Malnutrition - Breastfeeding
• Family history of seizures or patient history of febrile convulsions
• Use of antibiotics or inhaled steroids - Chronic liver, renal, or heart disease
• Stable neurologic conditions such as cerebral palsy or Down’s syndrome.
• Contraindications to killed vaccines and toxoids;
• Diphtheria; full dose is contraindicated in individuals more than 6 years, reduced• dose is given in such conditions Td.
• Pertussis; any abnormality in CNS like Spina Pefida or history of convulsion in a child, in
• acute febrile illness & in severe local or general reaction to a previous pertussis vaccine.
• Contraindications to live vaccines;
• General contraindications;
• - Within three of another live vaccine - During pregnancy - Acute febrile illness.
• - Immunological dysfunction like hypogamaglobinemia - Malignant diseases.
• - Steroid therapy, immunosuppression and radiotherapy.
• Specific contraindications;
• - Oral poliomyelitis; diarrhea and vomiting.
• - BCG; premature & LBW babies, local septic condition.
• - Rubella vaccine; Pregnancy
• Vaccination of special groups
• Immuno-compromised children
• Children with leukemia, Hodgkins, cancer, chemotherapy, HIV/AIDS
• should NOT receive live virus vaccines, such as measles, oral polio,
• May receive inactivated virus vaccines (DPT, injected polio vaccine, hepatitis B, pneumococcal, HiB) or passive immunization (gamma globulin).
• Splenectomised children or adults –
• Need pneumococcal, HiB, meningococcal vaccine as soon as possible after surgery.
• Sickle cell anemia – need pneumococcal vaccine; should have yearly influenza vaccine.
• High risk for meningitis (ie, Haj travelers, preschool or nursery children and adult attendants) – need meningococcal immunization.
• Health promotion and patient education regarding immunization:
• Parents may need to be reminded of the value of immunization of children to protect them against serious diseases to protect the family and community against these diseases.• Counsel parents about common potential side effects of vaccinations – mild fever, pain or soreness at injection site, delayed fever or rash with measles immunization.
• Give specific suggestions for dealing with adverse reactions of vaccination :
• a) acetaminophen dose for fever or fussiness of child
• b) observe rash for disappearance in 2-3 days
• c) cold compress to injection site if swollen or sore
• Inform parent of time of next scheduled immunization.