محاضرات فسلجة القلب
د عبد الحسن النيازي
اختصاص االمراض الباطنية
دكتوراه في الفسلجة الطبية
L1
Circulatory system is frequently divided into:
1. Cardiovascular system, which consists of the heart, blood vessels, and
blood.
2. Lymphatic system, which consists of lymphatic vessels and lymphoid
tissues within the spleen, thymus, tonsils, and lymph nodes.

The cardiovascular system (CVS)
The cardiovascular system consists of the heart, 60000 to 100000 km of
blood vessels, and blood. The main functions of the cardiovascular
system are to delivers oxygen and nutrients needed for metabolic
processes to the tissues, carries waste products from cellular metabolism
to the kidneys and other excretory organs for elimination, and circulates
electrolytes and hormones needed to regulate body functions. The heart
pressurizes blood and provides the driving force for its circulation
through the blood vessels. Blood is propelled away from the heart in the
arteries and returns to the heart in the veins. The exchange of materials
between blood and interstitial fluid occurs across capillaries in the
microcirculation.
At rest, the blood volume about 5 Liters is distributed as follows:
11% (0.55 L) in the Arteries and Arterioles
5% (0.25 L) in the Capillaries
17% (0.85 L) in the Heart and Lungs
67% (3.35 L) in the Veins
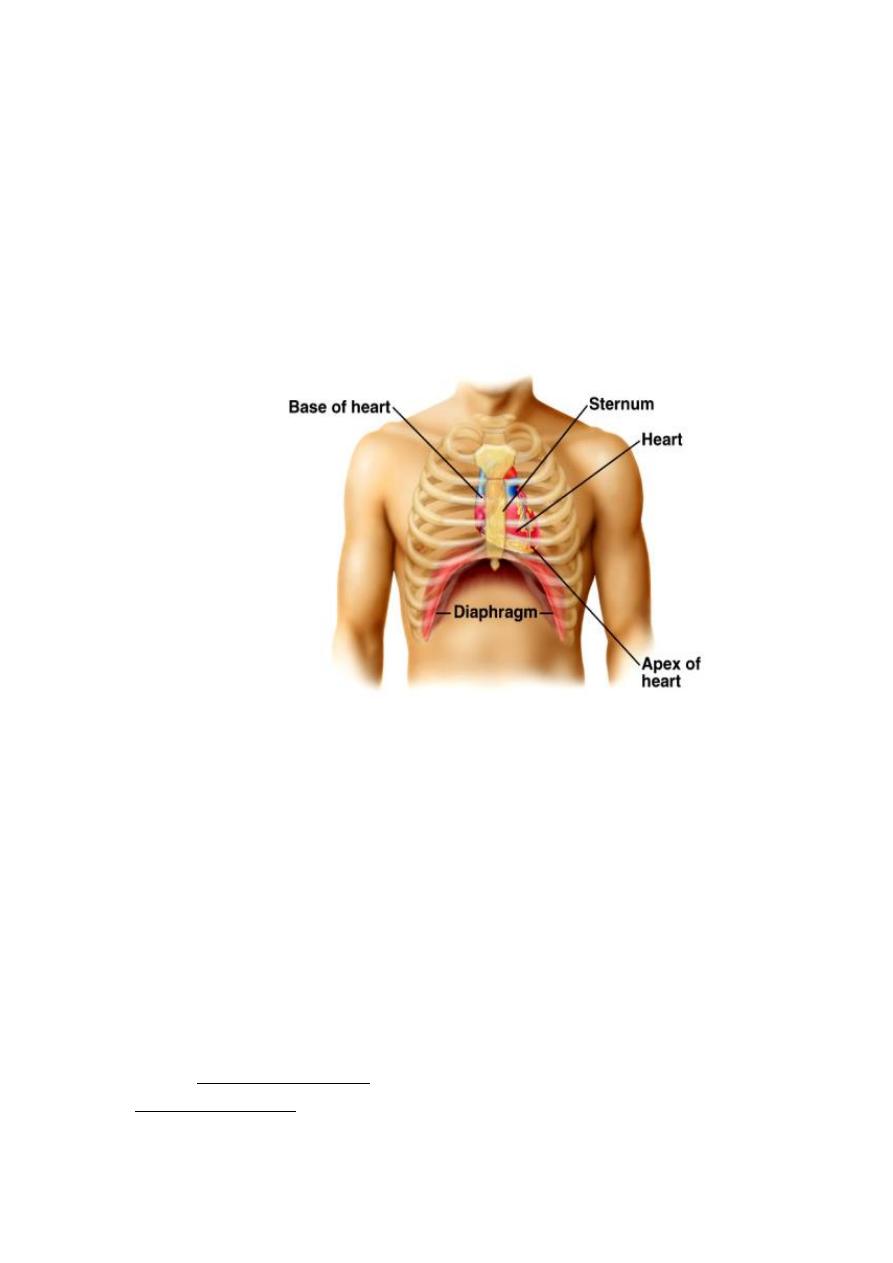
The heart
The heart is hollow cone-shaped four-chambered muscular pump
approximately the size of a fist, enclosed in a fibrous sac (the
pericardium). It lies in thoracic cavity in the space between the lungs. It
lies little more to the left than the right and present a base above and apex
bellow
Figure: location of heart.
The heart is separated by septum into right and left pump. The right pump
consists of right atrium and right ventricle. The right atrium is the
reservoir serving the right ventricle, which pumps blood to the pulmonary
circulation via the pulmonary artery. The left pump consist of left atrium
and left ventricle. The left atrium is the reservoir serving the left
ventricle, which pumps blood, via the aorta, to all other organs in the
body through the systemic circulation.
Pericardium
The pericardium or pericardial sac is a double layered closed sac that
surround the heart. It consist of fibrous connective tissue outer layer
called fibrous pericardium, and a thin transparent inner layer called
serous pericardium
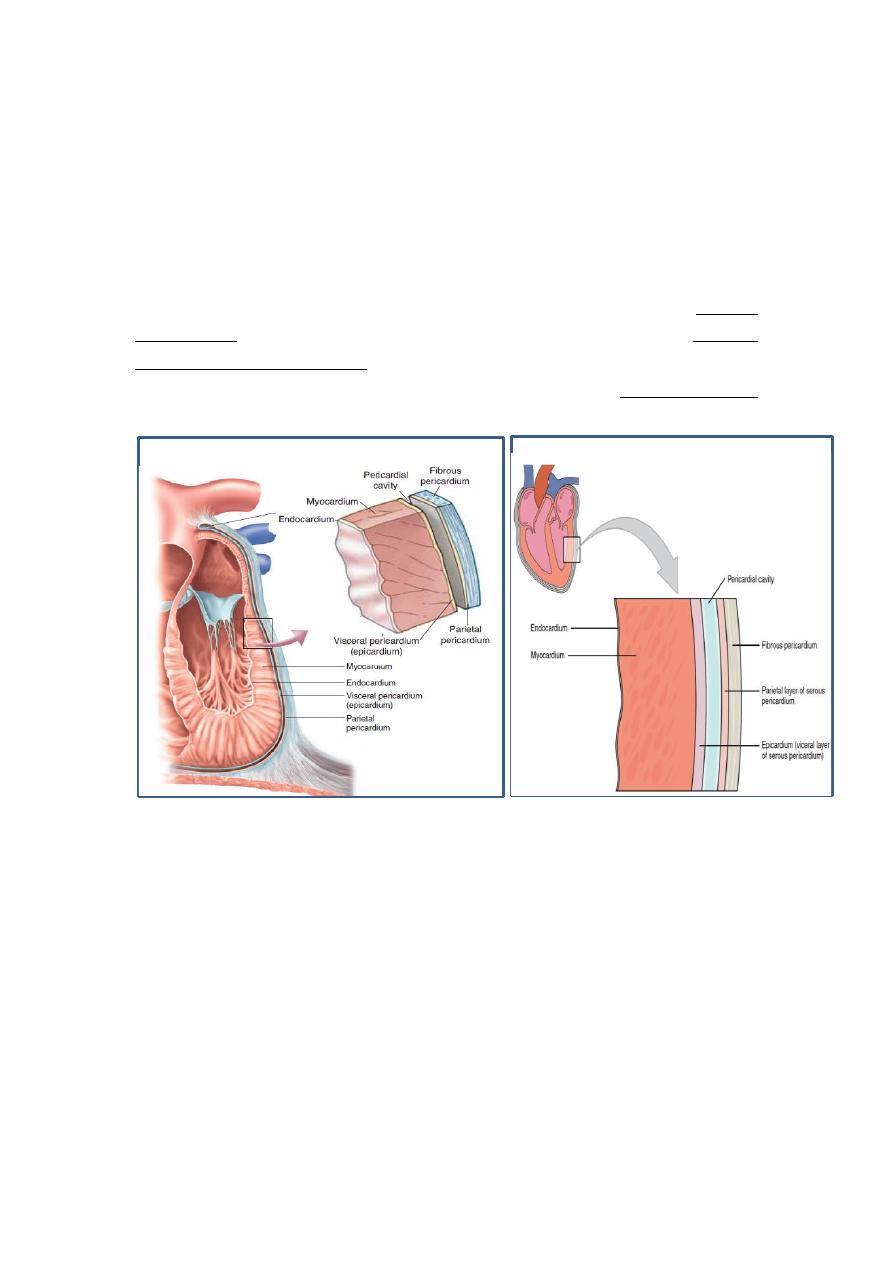
The fibrous pericardium prevent over distention of the heart and it is
continuous with tunica adventitia of great vessels above and is adherent
to diaphragm below.
The serous pericardium lining fibrous pericardium is the parietal
pericardium. And the part covering the heart surface is the visceral
pericardium or epicardium. The pericardial cavity between the visceral
and parietal pericardium is filled with a thin layer of pericardial fluid
which help to reduce friction as the heart moves within the pericardial
sac.
Heart wall
The heart wall consists of three layers: Epicardium, Myocardium and the
Endocardium.
1. Epicardium: is a thin serous membrane that constitute the smooth
outer surface of the heart.
2. Myocardium: is composed of cardiac muscle and is responsible for
the ability of the heart to contract.
3. Endocardium: this lines the chambers and valves of the heart. It is
thin smooth membrane that permits smooth flow of the blood
inside the heart.
Heart valves
For the heart to function effectively, blood flow must occur in a one-way
direction, moving forward through the chambers of the right heart to the
lungs and then through the chambers of the left heart to the systemic
circulation. This unidirectional flow is provided by the heart valves:
1. The atrioventricular (AV) valves control the flow of blood between the
atria and the ventricles. The thin edges of the AV valves form cusps, two
on the left side of the heart (i.e., bicuspid or mitral valve) and three on the
right side (i.e., tricuspid valve).
2. The aortic and pulmonic valves control the movement of blood out of
the ventricles. Because of their half moon shape, they often are referred to
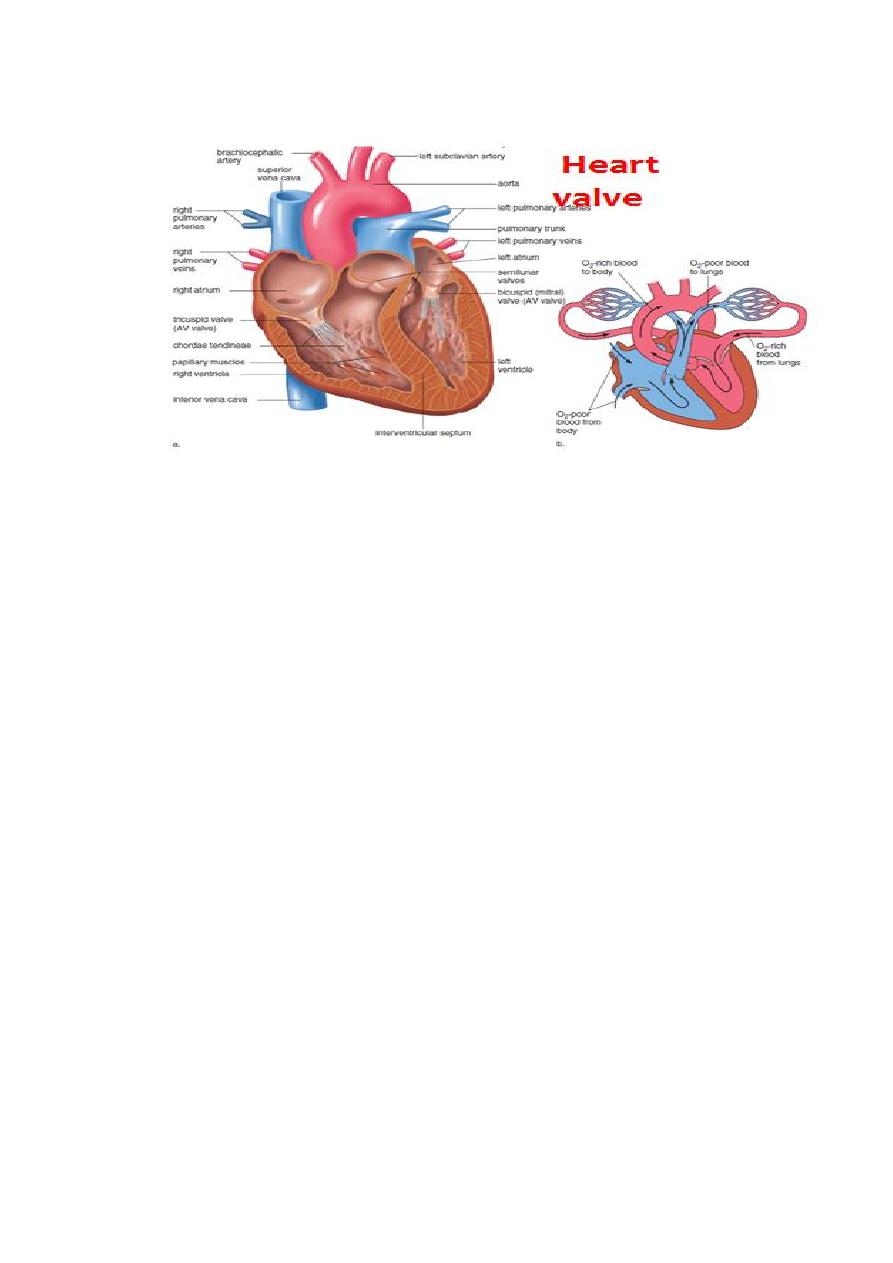
as the semilunar valves.

L2
Function of the heart valves
The function of AV valves is to prevent backflow (prevent regurgitation;
leakage) of blood into the atria during ventricular contraction. Normally
they allow blood to flow from the atrium to the ventricle but prevent
backward flow from the ventricle to the atria.
The pulmonary and aortic
valves allow blood to flow into the arteries during ventricular contraction
(systole) but prevent blood from moving in the opposite direction during
ventricular relaxation (diastole).
All valves close and open passively. That is, they close when a backward
pressure gradient pushes blood backward, and they open when a forward
pressure gradient forces blood in the forward direction.
Heart sounds
In healthy adults, there are two
normal heart sounds often
described
as
a lub and
a dub (or dup), that occur in
sequence with each heartbeat.
These
are
the first
heart
sound (S
1
)
and second
heart
sound (S
2
), produced by the
respectively. In addition to these
normal sounds, a variety of
other sounds may be present
including
are generated by turbulent flow of blood, which may occur
inside or outside the heart. Murmurs may be physiological (benign) or
pathological
(abnormal).
Abnormal
murmurs
can
be
caused
restricting the opening of a heart valve, resulting in turbulence
as blood flows through it. Abnormal murmurs may also occur with
valvular insufficiency (regurgitation), which allows backflow of blood
when the incompetent valve closes with only partial effectiveness.
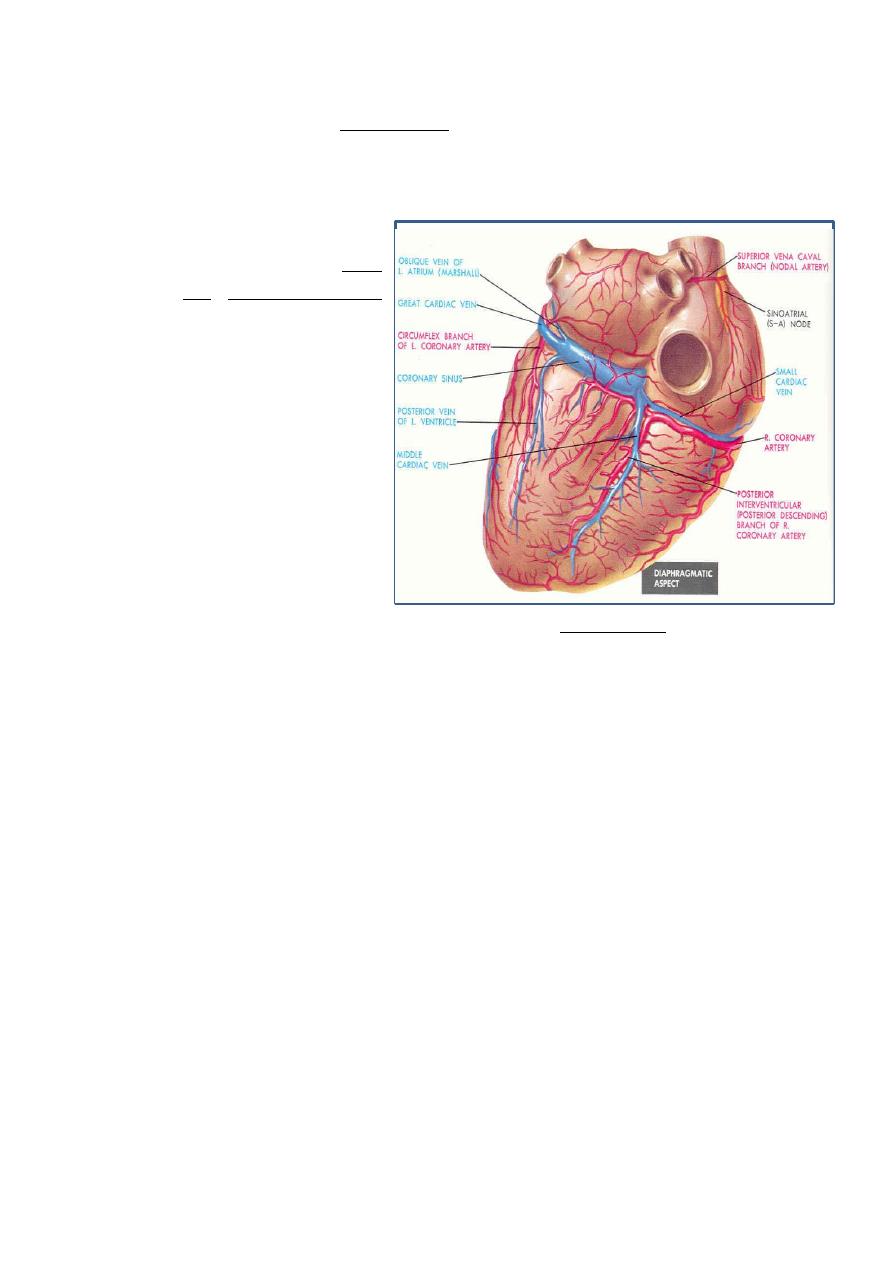
Coronary Circulation
The heart is supply with
arterial blood by the right
and left coronary arteries
which branched from aorta
just above the point where
the aorta leave the heart.
Coronary arteries receive
about 5% of blood pumped
from the heart. The coronary
arteries traverse the heart,
eventually
forming a vast
network of capillaries. Most
of the myocardium receives
blood from more than one
arterial branch. Furthermore there are many anastamoses or direct
connection between the arterial branches. The anastamoses are either
between branches of a given artery or between branches of different
arteries. So if one artery is block the area that primarily supplied by that
artery may still receive some blood through other arterial branch and
through anastamoses with other branches. Most of cardiac veins drain
into a single large vein, the coronary sinus, which drain into the right
atrium. A number of smaller cardiac vein empty into the cardiac vein, in
to the coronary sinus or directly into the right atrium.
Intrinsic Control of Heart beat
The parts of the heart normally beat in orderly sequence:
Contraction of the atria (atrial systole) is followed by contraction of the
ventricles (ventricular systole), and during diastole all four chambers are
relaxed.
The rhythmical contraction of the heart is due to the intrinsic conduction
system of the heart, which consists of:
1. SA (sinoatrial) node
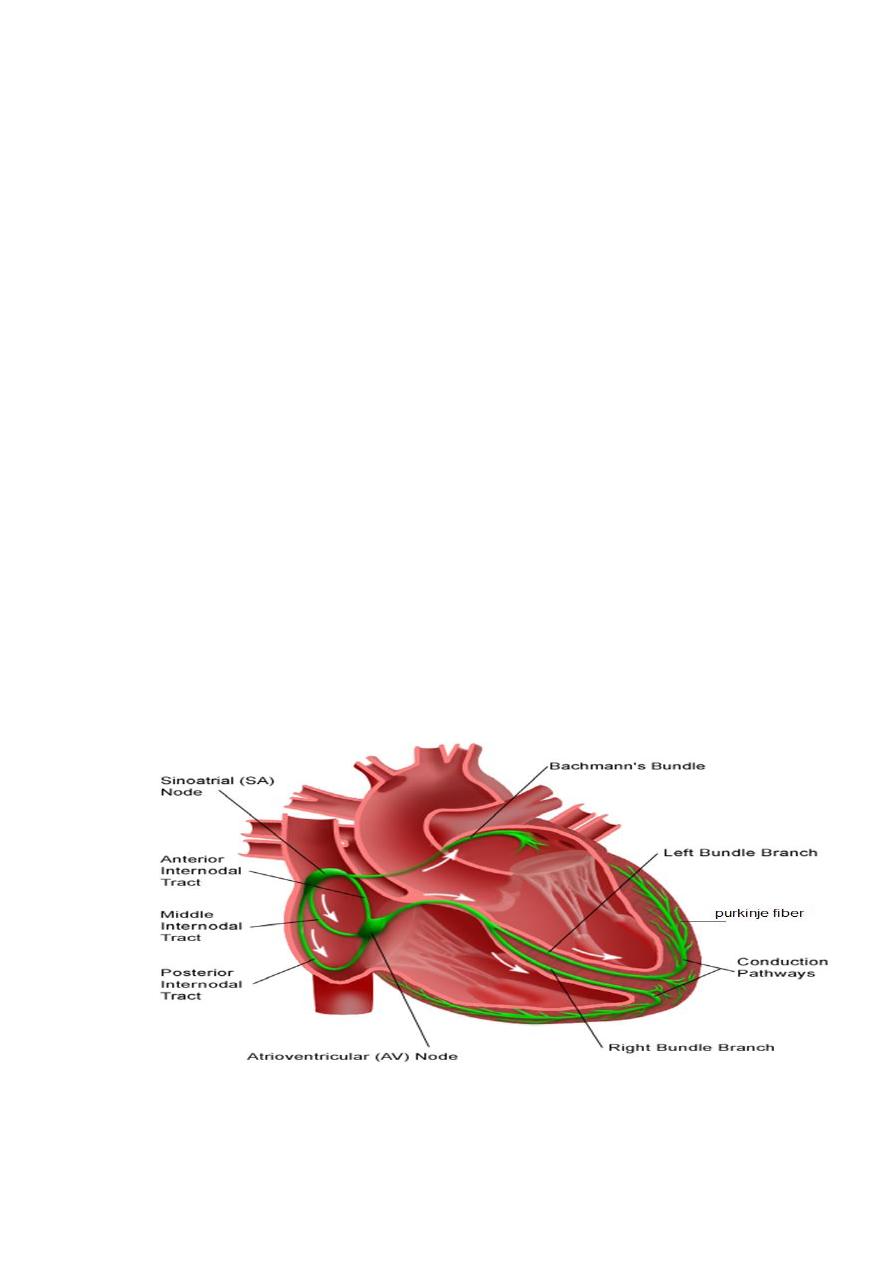
The sinoatrial (SA) node is the normal pacemaker of the heart and the
origin of each normal heartbeat. The SA node is a collection of
specialized myocytes near the site where the superior vena cava enters in
the wall of the right atrium. The depolarization begins in the sinoatrial
node (SA node), spread rapidly throughout the atria via gap junctions
between adjacent myocytes.
2. Atrioventricular Node (A-V node)
The atrioventricular (AV) node is the only electrical communication
between the atria and the ventricles. It is characterized by very slow
electrical conduction, ensuring that atrial contraction is completed before
the ventricles are activated. The AV node is continuous with the
atrioventricular bundle (bundle of His).
3. Atrioventricular bundle (bundle of His)
The AV bundle carry signals from atrium to the ventricles, in the
ventricles the AV bundle divide into right and left bundle branch, these
branches then divide into an extensive network of Purkinje fibers.
4. Purkinje fibers
Specialized conducting fibers that transmit electrical signals very rapidly
to all parts of the ventricular myocardium.
Spread of electrical signals along the heart
The electrical signal for contraction begins when the SA node fires an
action potential and the depolarization spreads to adjacent atrial cells
through gap junctions and through the internodal conducting pathways.
As action potentials spread across the atria, they encounter the fibrous
skeleton of the heart at the junction of the atria and ventricles. This
barricade prevents the transfer of electrical signals from the atria to the
ventricles. Consequently, the AV node is the only pathway through which
action potentials can reach the contractile fibers of the ventricles. The
electrical signal passes from the AV node through the AV bundle and
bundle branches to Purkinje fibers which transmit impulses very rapidly
to all part of ventricles.
Extrinsic Innervations of the Heart
The excitatory and conductive system of the heart receive innervations
from both division of autonomic nervous system. Although the basic
heart rate is set by the intrinsic conduction system, fibers of the
autonomic nervous system can modify the heart beat:
Sympathetic nervous system (the “accelerator”) increases both the rate
and the force of heartbeat. sympathetic stimulation increases the overall
activity of the heart.
Mechanism of the Sympathetic Effect. Stimulation of the sympathetic
nerves releases the hormone norepinephrine at the sympathetic nerve
endings. Norepinephrine in turn stimulates beta-1 adrenergic receptors,
which mediate the effects on heart rate. The precise mechanism by which
beta-1 adrenergic stimulation acts on cardiac muscle fibers is somewhat
unclear, but the belief is that it increases the permeability of the fiber
membrane to sodium and calcium ions.
The increase in permeability to calcium ions is at least partially
responsible for the increase in contractile strength of the cardiac muscle
under the influence of sympathetic stimulation, because calcium ions play
a powerful role in exciting the contractile process of the myofibrils.
Sympathetic Activity Summary:
heart rate = positive chronotropic effects
conduction of APs = positive dromotropic effects
contractility = positive inotropic effects
Parasympathetic nervous system slows the heart rate and force of
contraction.
Mechanism of the Vagal Effects. The acetylcholine released at the vagal
nerve endings greatly increases the permeability of the fiber membranes
to potassium ions, which allows rapid leakage of potassium out of the
conductive fibers. This causes increased negativity inside the fibers, an
effect called hyperpolarization, which makes this excitable tissue much
less excitable.
Parasympathetic Activity Summary:
heart rate = negative chronotropic effects
conduction of APs = negative dromotropic effects
contractility = negative inotropic effects
Abnormal Pacemakers “Ectopic” Pacemaker.
A pacemaker elsewhere than the sinus node is called an “ectopic”
pacemaker. An ectopic pacemaker causes an abnormal sequence of
contraction of the different parts of the heart and can cause significant
debility of heart pumping, this sometimes occurs in the A-V node or in
the Purkinje fibers when one of these becomes abnormal. In either case,
the pacemaker of the heart shifts from the sinus node to the A-V node or
to the excited Purkinje fibers. Under rarer conditions, a place in the atrial
or ventricular muscle develops excessive excitability and becomes the
pacemaker. Another cause of shift of the pacemaker is blockage of
transmission of the cardiac impulse from the sinus node to the other parts
of the heart.

L3
The cardiac cycle
The cardiac cycle is described as the cardiac events that occur from the
beginning of one heartbeat to the beginning of the next. Because of the
special arrangement of the conducting system from the atria into the
ventricles, there is a delay of more than 0.1 second during passage of the
cardiac impulse from the atria into the ventricles. This allows the atria to
contract ahead of ventricular contraction, thereby pumping blood into the
ventricles before the strong ventricular contraction begins. Thus, the atria
act as primer pumps for the ventricles, and the ventricles in turn provide
the major source of power for moving blood through the body’s vascular
system.
Each cardiac cycle has two phases: diastole, the time during which
cardiac muscle relaxes, and systole, the time during which the muscle
contracts. The duration of cardiac cycle a heart rate of 75 beat/min is
about 0. 8 second (0.5 second for diastole and 0.3 second for systole).
The long duration of diastole has important physiologic and clinical
implications. Why?
During systole, contraction of the cardiac muscle compresses the
intramyocardial vessels specially through the subendocardial vessels.
Thus, subendocardial region is in increased risk of ischemia and
infarction specially when diastolic pressure is low, and when a rapid heart
rate decreases the time spent in diastole, because the perfusion of the
subendocardial plexus occur mainly during diastole.
The main phases of cardiac cycle are:
1. Early diastole, the ventricular mass relaxes and the intraventricular
pressure falls below atrial pressure. This causes for the inflow
(Tricuspid/Mitral) valves to open. The atria have been distended by
continuous venous return during the preceding systole, so initially blood
is forced rapidly from the atria into the ventricles (rapid filling phase).
About 70% of ventricular filling occur in this phase.
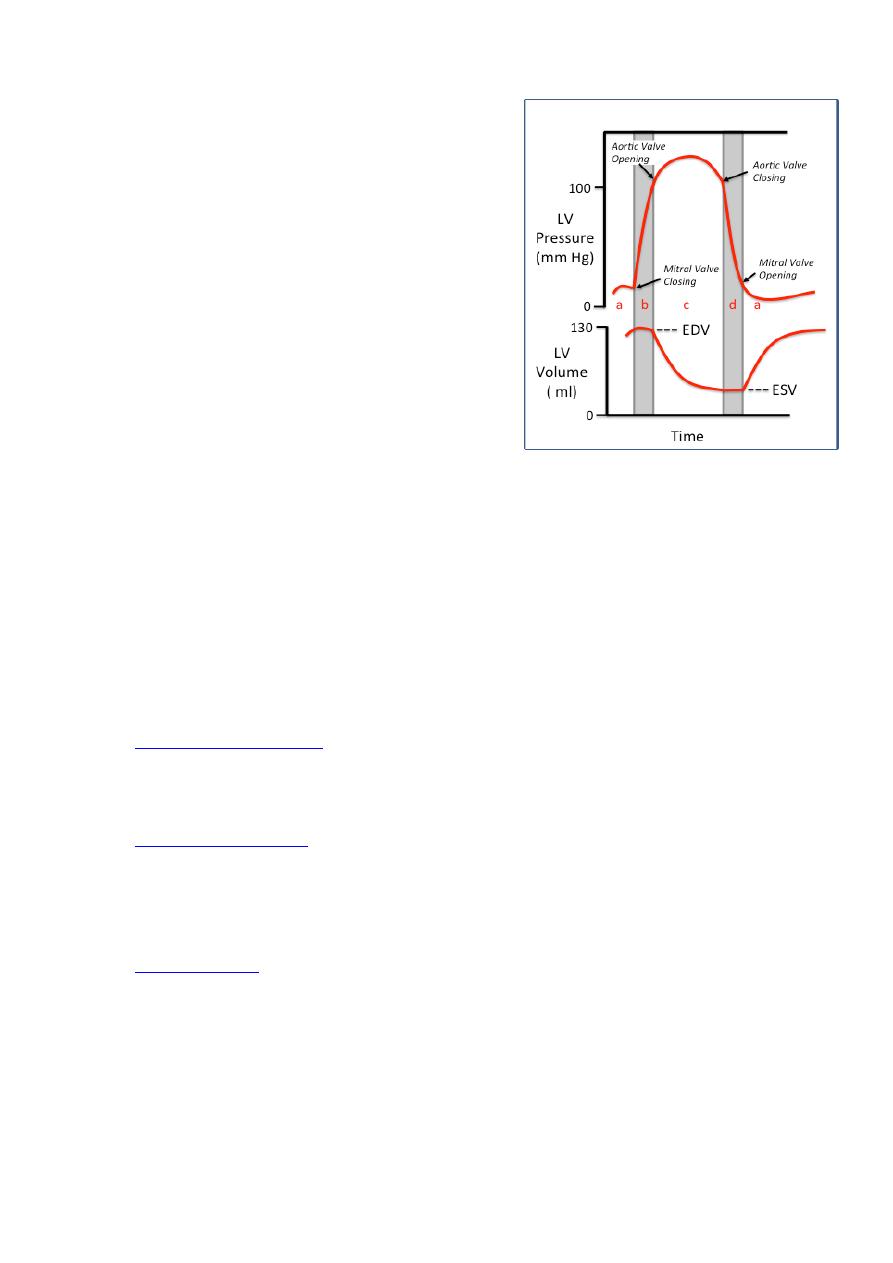
2.Atrial systole, is the contraction of the
atria, forcing a small extra amount of blood
into the ventricles.
3.Isovolumetric contraction, after a delay
of about 100-150ms the ventricles begin to
contract. As intraventricular pressure rises,
the mitral and tricuspid valves, closes
producing the first heart sound.
4. Ejection period,
the intraventricular pressure rises rapidly
until it exceeds the diastolic pressure in the
arteries, when the outflow (Aortic/Pulmonary) valves open. There is then
a rapid ejection period, where both intraventricular and arterial pressure
rise to a maximum.
5. Isovolumetric relaxation, towards the end of systole intraventricular
pressure falls and once below the arterial pressure the outflow valves
close creating the second heart sound.
When the intraventricular pressure falls below atrial pressure the
atrioventricular valves open and the whole process starts again.
The cardiovascular system consists of two pumps (left and right
ventricles) and two circuits (pulmonary and systemic) connected in series.
is the amount of blood pumped out by either the left
or right ventricle in 1 minute, and because the left and right pump are
connected in series, they CO are equal in both side. CO is the product of
heart rate (HR) and stroke volume (SV).
(SV) is defined as the volume of blood pumped out by one
ventricle with each beat. It is about 70 ml.
The normal value in adult is about 5 L/min. It is more in males than
females.

CO = HR X SV
Using normal resting values for heart rate (75 beats/min) and stroke
volume (70 ml/beat), the average adult cardiac output can be computed
CO = 75 X70 = 5250 ml/min
End diastolic volume
End diastolic volume (EDV), the amount of blood that collects in a
ventricle during diastole and just before contraction. It is normally about
120 ml.
End systolic volume
End systolic volume (ESV), the volume of blood remaining in a ventricle
after it has contracted. It is approximately 50 ml.
SV = EDV - ESV
SV = 120 - 50 = 70 ml.
Factors controlling cardiac output
Cardiac output is the product of heart rate and stroke volume.
Accordingly the factors which effect heart rate or stroke volume will play
important role in controlling cardiac output.
Heart rate, the heart rate is controlled primarily by the cardiac
innervation,
sympathetic
stimulation
increasing
the
rate
and
parasympathetic stimulation decreasing it. Heart rate can also be
influenced by other factors:
-Hormones, epinephrine and norepinephrine released from the adrenal
medullae during exercise and stress increase both heart rate and
contractility.
-Body temperature, increased body temperature, as occurs during a fever
or strenuous exercise, increases heart rate by enhancing the metabolic rate
of cardiac cells.
-Age, newborns have higher heart rates (120 beats/ min) than adults. The
heart rate slows down gradually during childhood, until it reaches the
adult rate of around 72 beats/min.

-Gender, females tend to have higher resting heart rates than males.
-Physical fitness, regular exercise tends to slow the resting heart rate.
Well-trained athletes have slower resting heart rates (40–60 beats/min)
but have normal resting cardiac outputs. Why
Because their hearts are enlarged, giving them larger stroke volumes.
Factors affect Stroke volume
1. Preload. Is the load that determines the initial length of the resting
muscle before contraction. The level of the preload is represented by the
end-diastolic volume (EDV) i.e., by the venous return
2. Contractility is defined as the contractile strength achieved at a given
muscle length. An increase in contractility is due to a greater Ca
2+
influx
into the cytoplasm from the extracellular fluid and the SR. Enhanced
contractility results in ejection of more blood from the heart.
3. Afterload is the pressure that the ventricles must overcome to open the
aortic and pulmonary valves and force blood into blood vessels. Afterload
is determined by:
• The aortic pressure (arterial systolic blood pressure).
• The arterial wall rigidity (arteriosclerosis).
• Blood viscosity (polycythemia).
Increased afterload leads to decrease SV as in hypertension.
L4
Ejection fraction
The contractility of the myocardium determines the ejection fraction of
the heart, which is the ratio of the volume of blood ejected from the left
ventricle per beat (stroke volume) to the volume of blood in the left
ventricle at the end of diastole (end-diastolic volume):
Ejection fraction = SV / EDV
Under normal resting conditions in which the end-diastolic volume is 120
to 130 ml and the stroke volume is 70 ml/beat, the ejection fraction is 55
to 60%.
During exercise when sympathetic stimulation to the heart is increased,
the ejection fraction may increase to more than 80% resulting in greater
stroke volume and cardiac output.
Cardiovascular diseases
-Varicose veins
Varicose veins are veins that have become tortuous and dilated because
of incompetent (leaky) valves. More than 15% of adults suffer from
varicose veins, usually in the lower limbs. Several factors contribute,
including heredity and conditions that hinder venous return, such as
prolonged standing in one position, obesity, or pregnancy.
-Hypertension
Hypertension, or high blood pressure, is probably the most common of all
health problems in adults and is the leading risk factor for cardiovascular
disorders. Hypertension commonly is divided into the categories of
primary and secondary hypertension. In primary, or essential,
hypertension, which accounts for 90% to 95% of all hypertension, the
chronic elevation in blood pressure occurs without evidence of other
disease. In secondary hypertension, the elevation of blood pressure results
from some other disorder, such as kidney disease.

Angina pectoris
Angina pectoris (chest pain) is the most common symptom of chronic
ischemic heart disease. Angina is caused by an imbalance between the
oxygen supply and oxygen demand of the cardiac muscle. Myocardial
oxygen demand increases during exercise and emotional stress. If
coronary blood flow does not increase proportionately to meet this
demand, then the affected tissue becomes ischemic and pain develops.
This ischemia and pain may be treated pharmacologically with
nitroglycerin, a drug that causes vasodilation and an increase in blood
flow. However, this effect occurs not only in the coronary arteries, but
also in blood vessels throughout the body. Therefore, in addition to
improving coronary blood flow, administration of nitroglycerin may
decrease systemic blood pressure. Most frequently, this drug is
administered in the sublingual form and its effects are apparent within 1
to 3 minutes.
Heart failure
Heart failure occurs when the heart can't pump enough blood to meet the
metabolic needs of the body. Heart failure results in intravascular and
interstitial volume overload and poor tissue perfusion. Although the most
common cause of heart failure is coronary artery disease, it also occurs in
infants, children, and adults with congenital and acquired heart defects.
Heart failure may be classified according to the side of the heart affected
(left- or right-sided heart failure) or by the cardiac cycle involved
(systolic or diastolic dysfunction).
Left-sided heart failure. This type of heart failure occurs as a result of
ineffective left ventricular contractile function. As the pumping ability of
the left ventricle fails, cardiac output falls. Blood is no longer effectively
pumped out into the body; it backs up into the left atrium and then into
the lungs, causing pulmonary congestion, dyspnea, and activity
intolerance. If the condition persists, pulmonary edema and right-sided
heart failure may result. Common causes include left ventricular
infarction, hypertension, and aortic and mitral valve stenosis.
Right-sided heart failure. Right-sided heart failure results from
ineffective right ventricular contractile function. Consequently, blood is
not pumped effectively through the right ventricle to the lungs, causing

blood to back up into the right atrium and into the peripheral circulation.
The patient gains weight and develops peripheral edema and
engorgement of the kidney and other organs. It may be due to an acute
right ventricular infarction or a pulmonary embolus. However, the most
common cause is profound backward flow due to left-sided heart failure.
Systolic dysfunction. Systolic dysfunction occurs when the left ventricle
can't pump enough blood out to the systemic circulation during systole
and the ejection fraction falls.
Diastolic dysfunction. Diastolic dysfunction occurs when the ability of
the left ventricle to relax and fill during diastole is reduced and the stroke
volume falls.
Cardiac Arrest
This results from cessation of all electrical control signals in the heart.
That is, no spontaneous rhythm remains.
Cardiac arrest may occur during deep anesthesia, when many patients
develop severe hypoxia because of inadequate respiration. The hypoxia
prevents the muscle fibers and conductive fibers from maintaining normal
electrolyte concentration differentials across their membranes, and their
excitability may be so affected that the automatic rhythmicity disappears.
In most instances of cardiac arrest from anesthesia, prolonged
cardiopulmonary resuscitation (many minutes or even hours) is quite
successful in re-establishing a normal heart rhythm.

L5
Electrocardiography
The ECG is a recording of the electrical activity of the heart. The
electrical currents generated by the heart spread through the body to the
skin, where they can be sensed by appropriately placed electrodes,
amplified, and viewed on an oscilloscope or chart recorder. A standard
ECG is obtained by placing an electrode on each limb and at six specific
locations on the anterior chest wall. In a lead, one electrode is regarded as
the positive side of a voltmeter and another is the negative side.
The normal electrocardiogram is composed of P wave, QRS complex,
and T wave. The QRS complex is three separate waves: the Q wave, the
R wave, and the S wave.
P wave
The P wave represents atrial depolarization. In normal ECGs, the P-wave
precedes the QRS complex. The shape of a P-wave is usually smooth and
rounded.
PR interval
The PR interval is the time between the onset of atrial depolarization and
the onset of ventricular depolarization.
QRS complex
The QRS complex represents the ventricular depolarization.
ST segment
The ST segment is the line that from the end of the QRS complex to
beginning of the T wave.
T wave
T wave produced by ventricular repolarization.
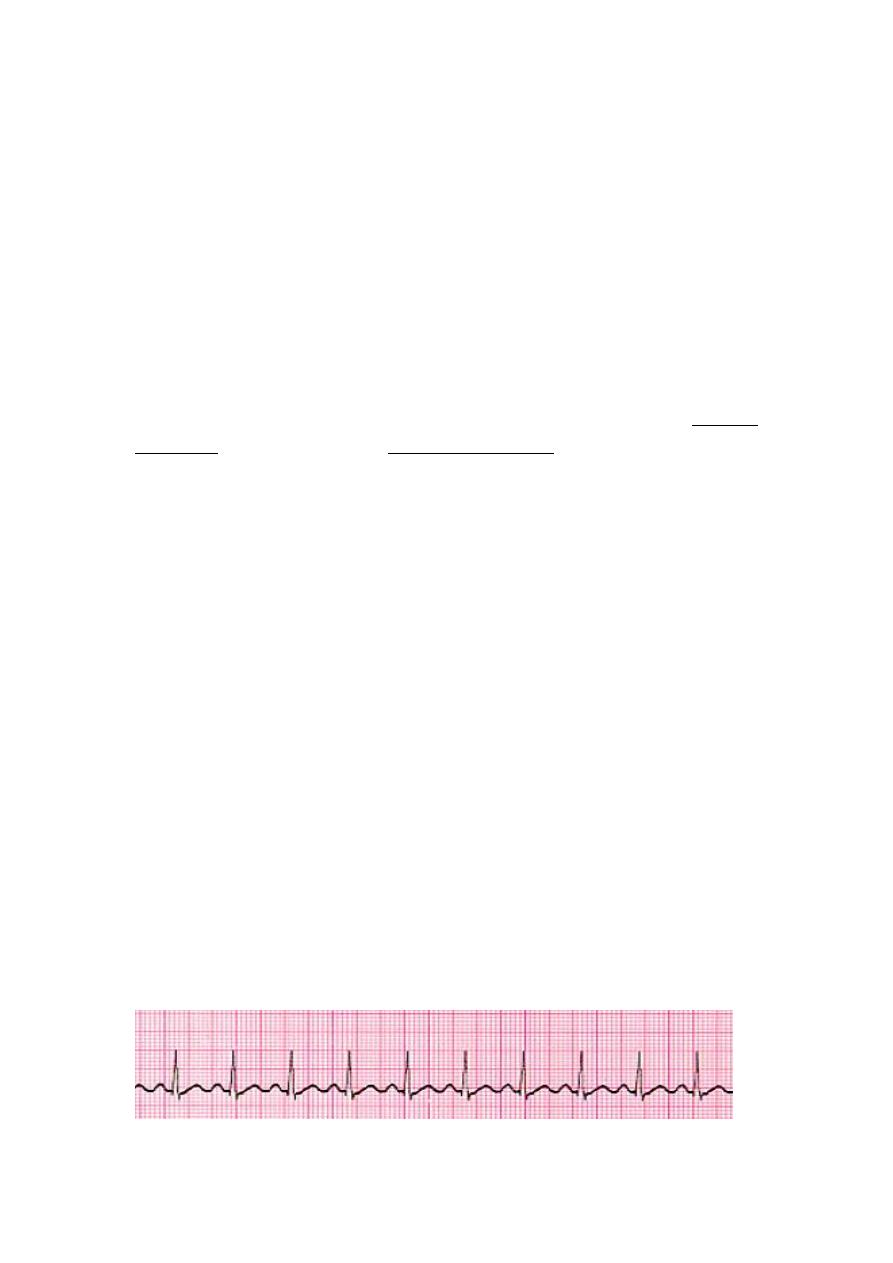
QT interval
The QT interval is measured from the beginning of the QRS complex to
the end of the T wave and represents the total time taken for
depolarization and repolarization of the ventricles.
Cardiac arrhythmias
The normal cardiac impulse starts at the sinoatrial node; passes through
the atria to the AV node, where it slows; and then continues down the
His-Purkinje system to the ventricular myocardium, where the wave of
depolarization terminates because there is no further tissue to depolarize.
Most arrhythmias can be described as either abnormalities of impulse
formation or abnormalities of impulse conduction.
1.Abnormalities of impulse formation result in an inappropriately fast
firing rate of either the normal sinus pacemaker cells or an ectopic
pacemaker focus.
2.Abnormalities of impulse conduction may result in delayed or
accelerated conduction.
Cardiac arrhythmias are commonly divided into two categories:
1. The supraventricular arrhythmias include those that are generated in
the SA node, atria, AV node, and junctional tissues.
2. The ventricular arrhythmias include those that are generated in the
ventricular conduction system and the ventricular muscle.
Examples of cardiac arrhythmias
1.Tachycardia
Tachycardia, defined as heart rate faster than 100 beats /min. ECG: is
normal except the rate is fast. Causes: increased body temperature,
stimulation of the heart by the sympathetic nerves.
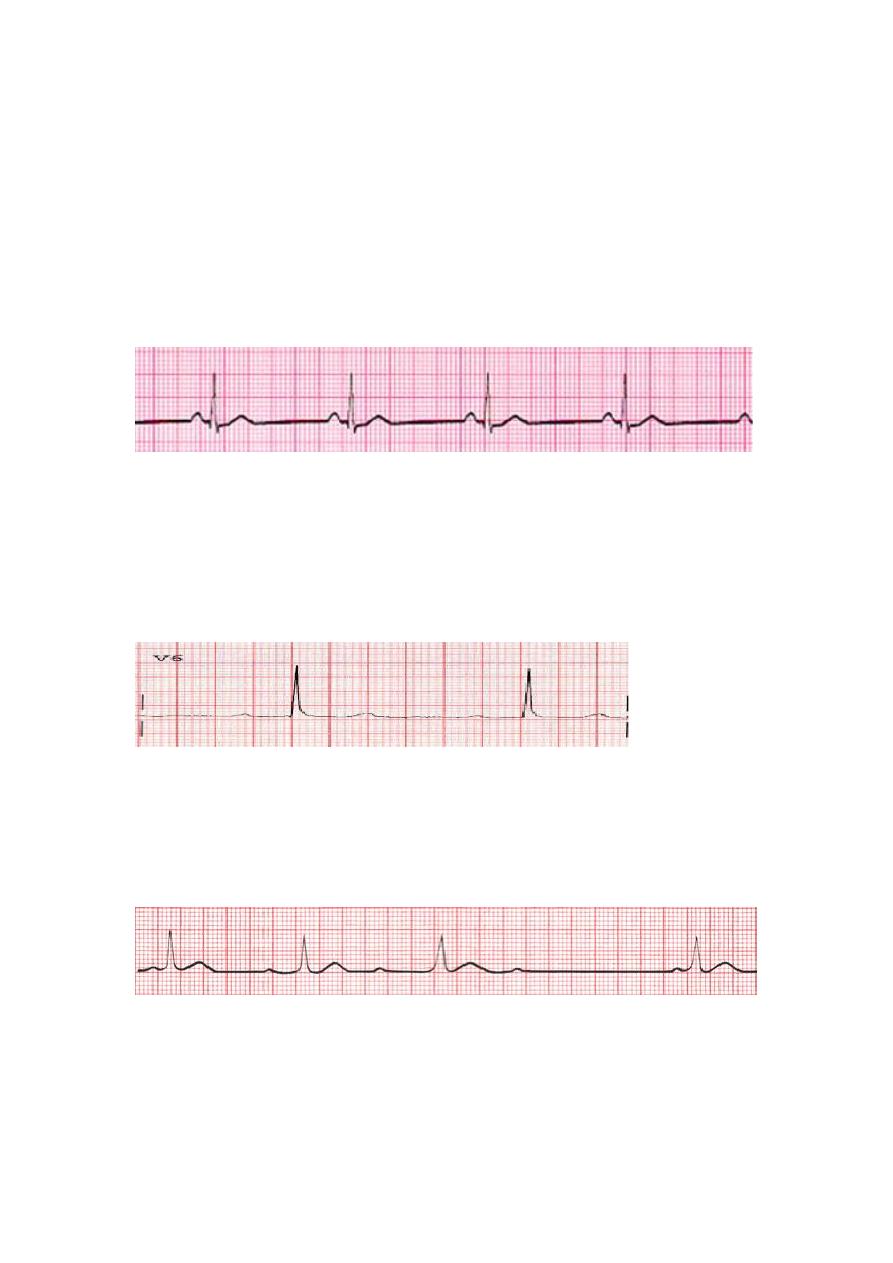
2.Bradycardia
bradycardia, defined as heart rate fewer than 60 beats/ min. ECG: is
normal except the rate is slow. Causes, Athlete’s heart or Vagal
stimulation.
The athlete's heart is larger and considerably stronger than that of a
normal person, which allows the athlete's heart to pump a large stroke
volume.
3. Atrioventricular block
Impairment of impulse conduction from atria to ventricle
• First degree block (Prolonged P-R Interval)
ECG: normal a part from increased P-R interval to greater than 0.20 S.
• Second-degree heart block
The ECG show a progressive lengthening of the PR interval and finally
there is failure of impulse transmission to ventricle (P wave not followed
by QRS complex).
• Complete A-V block (third degree block).
This condition characterized by complete block of the impulse
transmission from the atria into the ventricles. The ventricles establish
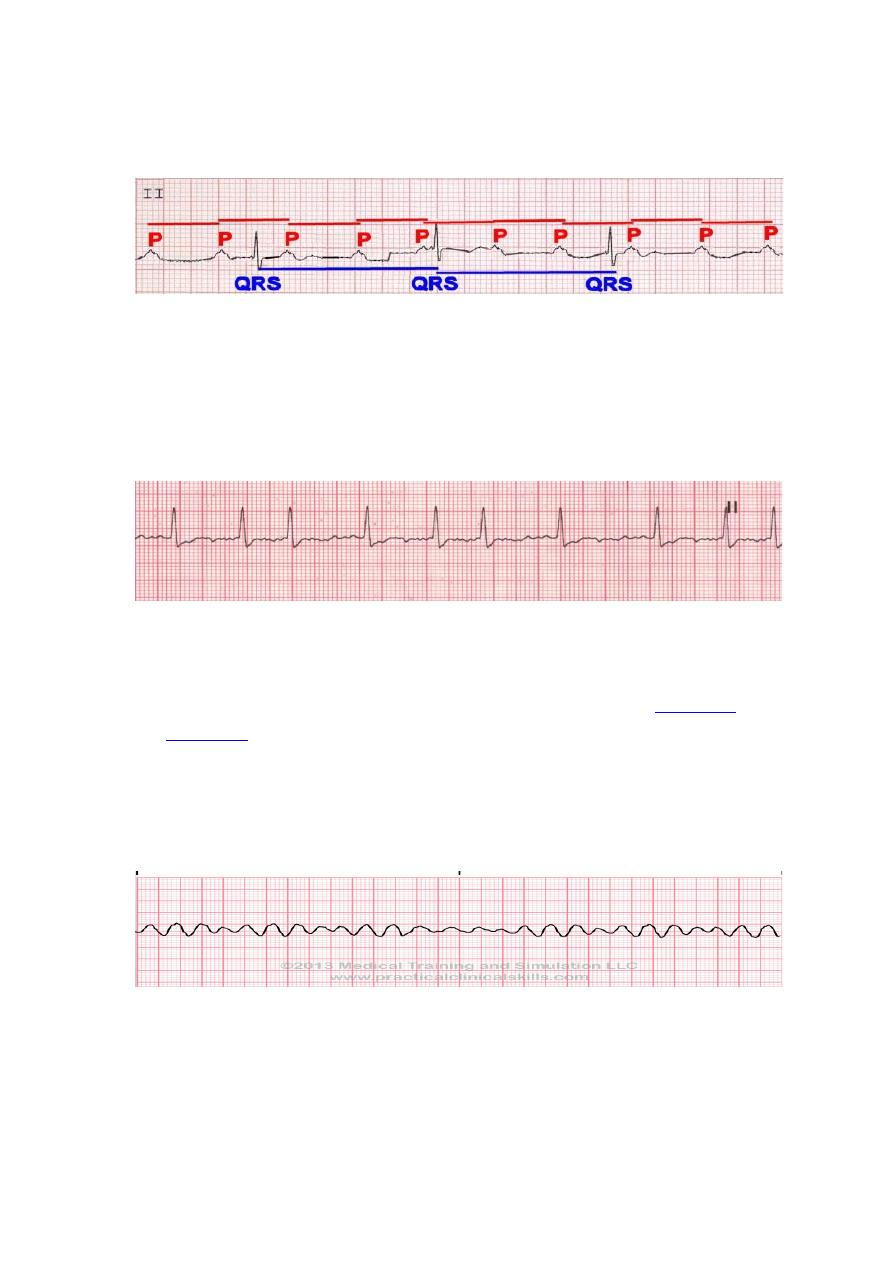
their own pulse rate, usually originating in the A-V node or A-V bundle.
ECG: P waves become dissociated from the QRS-T complexes.
4. Atrial Fibrillation
In atrial fibrillation, the atria beats very rapidly (300-500/min) in a
completely irregular and disorganized fashion. The ventricles beat at a
completely irregular rate, usually 80-160/min. The QRS-T complexes are
usually normal.
5.Ventricular Fibrillation
Ventricular fibrillation is a condition in which there is uncoordinated,
totally irregular and ineffective contraction of the
. The fibrillating ventricles cannot pump blood effectively,
and circulation of the blood stops. Therefore, in the absence of
emergency treatment, ventricular fibrillation that lasts more than a few
minutes is fatal. The most frequent cause of ventricular fibrillation is
myocardial infarction, sudden electrical shock of the heart.
Electroshock Defibrillation of the Ventricles
Although a moderate alternating-current voltage applied directly to the
ventricles almost invariably throws the ventricles into fibrillation, a
strong high-voltage alternating electrical current passed through the

ventricles for a fraction of a second can stop fibrillation by throwing all
the ventricular muscle into refractoriness simultaneously.
This is accomplished by passing intense current through large electrodes
placed on two sides of the heart. The current penetrates most of the fibers
of the ventricles at the same time, thus stimulating essentially all parts of
the ventricles simultaneously and causing them all to become refractory.
All action potentials stop, and the heart remains quiescent for 3 to 5
seconds, after which it begins to beat again, usually with the sinus node
or some other part of the heart becoming the pacemaker.
Link to pharmacology.
Cardiac glycosides (digoxin) are an important class of therapeutic agents
used to increase the contractility of failing hearts.
Digoxin’s primary mechanism of action involves inhibition of the (
), mainly in the myocardium. This inhibition causes an increase in
intracellular sodium levels, resulting in a reversal of the action of
the
which
normally
imports
three
extracellular sodium ions into the cell and transports one intracellular
calcium ion out of the cell. The reversal of this exchange causes an
increase in the intracellular calcium concentration that is available to the
contractile proteins. Increased intracellular calcium lengthens phase 4 and
phase 0 of the
, which leads to a decrease in heart
rate. Increased amounts of Ca
2+
also leads to increased storage of
, causing a corresponding increase
in the release of calcium during each action potential, this leads to
increased contractility (the force of contraction) of the heart.
? inotropic effect
? chronotropic effect
? dromotropic effect
Review: A 50-year-old man has a blood pressure of 140/85 and weighs
200 lb. He reports that he is not feeling well, his EKG has no P-waves, he
has a heart rate of 46, and the QRS complexes occur regularly. What is
his likely condition?

A) First-degree heart block
B) Second-degree heart block
C) Third-degree heart block
D) Sinoatrial heart block
E) Sinus bradycardia
