1
HEMODYNAMIC DISORDERS
Prof. Dr. Maha Shakir Lec.2
Edema
Definition
: edema is an accumulation of interstitial fluid within
tissues.
Extravascular fluid can also collect in body cavities such as:
a) Hydrothorax
– fluid accumulation in pleural cavity in a
pathologic amount.
b) Hydropericardium
– pathologic amount of fluid accumulated in
the pericardial cavity.
c) Hydroperitoneum (ascites)
– fluid accumulation in peritoneal
cavity.
d)
Anasarca
– is a severe & generalized edema of the body with
profound subcutaneous tissue swelling and accumulation of fluid
in body cavities.
Mechanism of edema formation:
Approximately 60% of lean body weight is water, two thirds of
which is intracellular. Most of the remaining water is found in
extracellular compartments in the form of interstitial fluid; only
5% of the body’s water is in blood plasma.
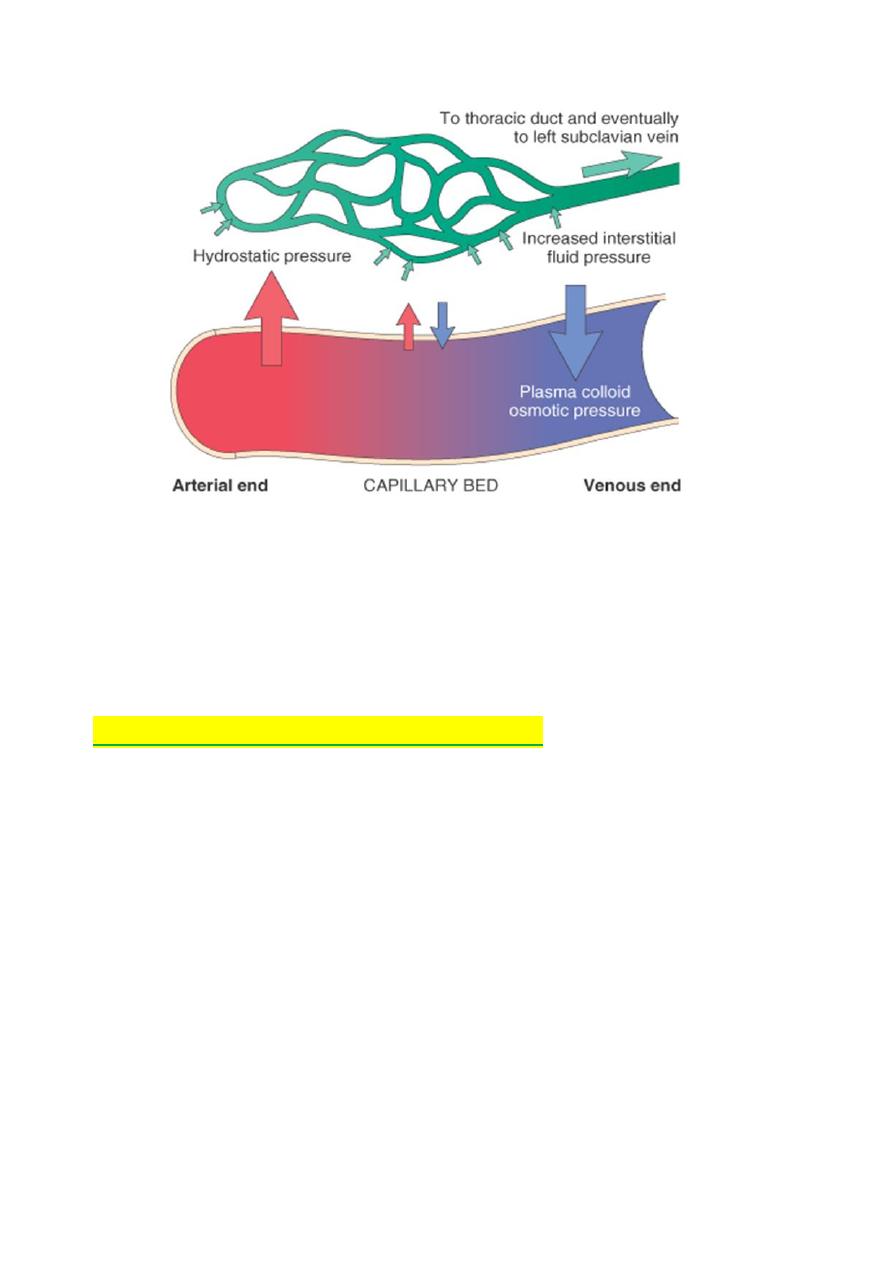
The capillary endothelium acts as a semi permeable membrane
and highly permeable to water & to almost all solutes in plasma
with an exception of
proteins
. Proteins in plasma and interstial
fluid are especially important in controlling plasma & interstitial
fluid volume.
Normally, any outflow of fluid into the interstitium from the
arteriolar end of the microcirculation is nearly balanced by inflow
at the venular end. Therefore, normally, there is very little fluid in
the interstitium. Tissue lymphatics drain much of the excess fluid
back to the circulation by way of thoracic duct.
2
So causes of Edema are:
1) Increased Hydrostatic pressure
2) Decrease plasma Oncotic pressure
3) Increased vascular permeability
4) Lymphatic channels obstruction
5) Sodium retention
We will discuss each of the above sequentially.
1) Increased Hydrostatic pressure
Increases in hydrostatic pressure are mainly caused by
disorders that impair venous return.
•
Local increases
in intravascular pressure caused, for
example, by deep venous thrombosis in the lower extremity can
cause edema restricted to the distal portion of the affected leg.
•
Generalized increases
in venous pressure, with resultant
systemic edema, occur most commonly in congestive heart
failure
Several factors increase venous hydrostatic pressure in patients
with congestive heart failure:
•
The reduced cardiac output leads to systemic venous
congestion and resultant increase in capillary hydrostatic
pressure.
•
reduction in cardiac output results in hypoperfusion of the
kidneys, triggering the renin-angiotensin-aldosterone axis and
inducing
sodium
and
water
retention
(secondary
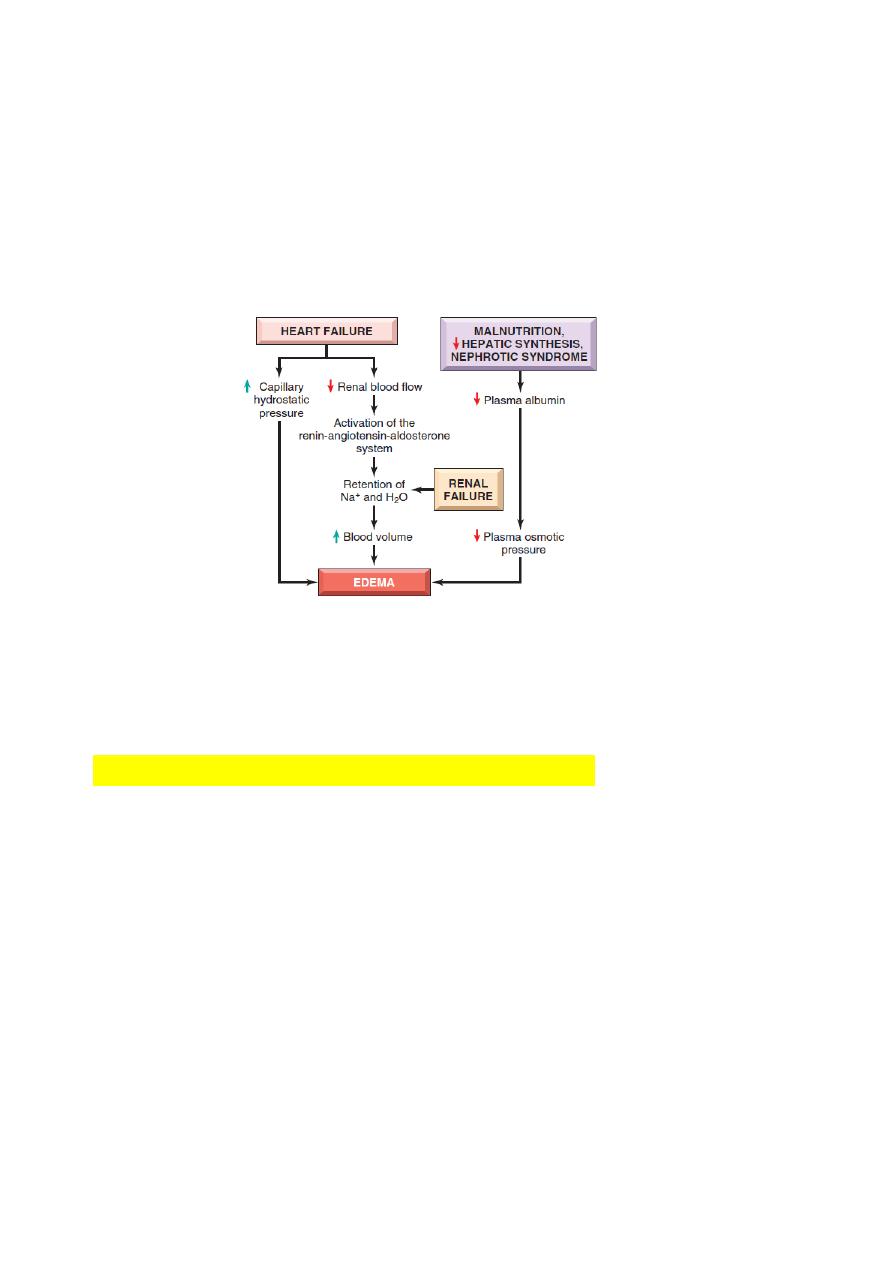
3
hyperaldosteronism) leads to increase blood volume and
worsening of edema .
a vicious circle of fluid retention, increased venous hydrostatic
pressures, and worsening edema ensues.
Unless cardiac output is restored or renal water retention is
reduced (e.g., by salt restriction or treatment with diuretics or
aldosterone antagonists), this downward spiral continues.
Renal failure also cause edema because of retention of Na and
water leads to increase blood volume (increase hydrostatic
pressre).
2) Decrease plasma Oncotic pressure
Reduction of plasma albumin concentrations leads to
decreased colloid osmotic pressure of the blood and loss
of fluid from the circulation.
Under normal circumstances, albumin accounts for almost half of
the total plasma protein.
Common causes of reduced plasma osmotic pressure
.
•
Albumin lost from the circulation.
•
Or albumin synthesized in inadequate amounts.
Nephrotic syndrome
is the most important cause of albumin loss
from the blood. the glomerular capillaries become leaky, leading
to the loss of albumin (and other plasma proteins) in the urine
and the development of generalized edema.

4
Reduced albumin synthesis occurs in the setting of
severe liver
disease (e.g., cirrhosis) and protein malnutrition.
low albumin levels lead in a stepwise fashion to edema, reduced
intravascular volume, renal hypoperfusion, and secondary
hyperaldosteronism.
Increased salt and water retention by the kidney not only fails to
correct the plasma volume deficit but also exacerbates the
edema, because the primary defect—low serum protein—
persists.
3) Increased Vascular permeability:
Increased vascular permeability usually occurs due to
acute
inflammation
.
In inflammation, chemical mediators are produced. Some of
these mediators cause increased vascular permeability which
leads to loss of fluid & high molecular weight albumin and
globulin into the interstitium.
Such edema (i.e. that caused by increased vascular
permeability) is called
inflammatory edema
.
Inflammatory edema differs from non inflammatory edema by the
following features:
a) Inflammatory edema (exudate)
•
Due to inflammation-induced increased permeability and
leakage of plasma proteins.
•
Forms an exudate [protein rich]
•
Specific gravity > 1.012
b) Non-inflammatory oedema (transudate)
•
A type of edema occurring in hemodynamic derangement
(i.e. increased plasma hydrostatic pressure & decreased plasma
oncotic pressure.)
•
Formed transudate [protein poor]
•
Specific gravity < 1.012.
4) Lymphatic channels obstruction
Edema may result from lymphatic obstruction that compromises
resorption of fluid from interstitial spaces. Impaired lymphatic
drainage and consequent
lymphedema
It usually results from a localized obstruction caused by an
inflammatory
or
neoplastic
condition.
For example,
5
•
the parasitic infection
filariasis
can cause massive edema of
the lower extremity and external genitalia (so-called
“elephantiasis”) by producing inguinal lymphatic and lymph node
fibrosis.
•
Infiltration and obstruction of superficial lymphatics by
breast cancer may cause edema of the overlying skin; the
characteristic finely pitted appearance of the skin of the affected
breast is called
peau d’orange
(orange peel).
•
Lymphedema also may occur as a complication of
therapy.
in women with breast cancer who undergo axillary lymph node
resection
and/or
irradiation
, both of which can disrupt and
obstruct lymphatic drainage, resulting in severe
lymphedema of
the arm.
5) Sodium and water retention:
Excessive retention of salt (and its obligate associated water)
can lead to edema by
increasing hydrostatic pressure
(because
of expansion of the intravascular volume) and
reducing plasma
osmotic pressure.
Excessive salt and water retention are seen in
a wide variety of diseases that compromise renal function,
including poststreptococcal glomerulonephritis and acute renal
failure
Causes of sodium and water retention:
1- excessive salt intake with renal insufficiency.
2- increased tubular reabsorption of sodium
3-Renal hypo perfusion
4-Increased renin- angiotensin- aldosteron secretion.
Morphology of edema
Gross examination:
clearing and separation of the extracellular matrix (ECM)
elements. edema most commonly encountered in subcutaneous
tissues, lungs, and brain.
Subcutaneous edema
can be diffuse but usually accumulates
preferentially in parts of the body where hydrostatic pressures
are highest. Thus, edema typically is most pronounced in the legs
with
dependent edema
. Finger pressure over edematous
subcutaneous tissue displaces the interstitial fluid, leaving a
finger-shaped depression; this appearance is called
pitting
edema.
Edema resulting from renal dysfunction or nephrotic syndrome

6
often manifests first in
loose connective tissues (e.g., the eyelids,
causing periorbital edema).
Pulmonary edema
, the lungs
often are two to three times their
normal weight, and sectioning
shows frothy, sometimes blood-
tinged fluid consisting of a
mixture of air, edema fluid, and
extravasated red cells.
Brain edema
can be localized (e.g., because of abscess
or
tumor) or generalized, depending on the nature and extent
of the
pathologic process or injury.
With generalized edema, the
sulci are narrowed as the gyri swell
and become flattened against
the skull.
