
Conversion of
amino acids to
specialized products
●
In addition to serving as building blocks for proteins, amino
acids are precursors of many nitrogen-containing
compounds that have important physiologic functions.
●
These molecules include
porphyrins, neurotransmitters,
hormones, purines, and pyrimidines
.
2

PORPHYRIN METABOLISM
3
●
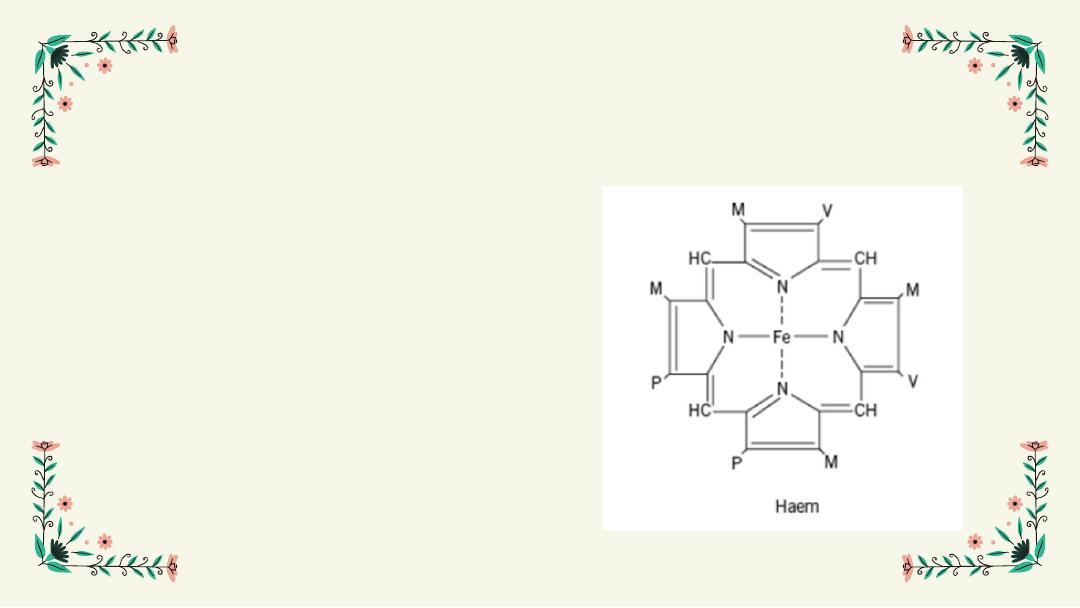
Porphyrins are cyclic compounds that readily bind metal
ions, usually ferrous (Fe
2+
) or ferric (Fe
3+
) iron.
●
The most prevalent metalloporphyrin in humans is heme,
consists of one Fe
2+
coordinated in the center of
tetrapyrrole ring of protoporphyrin IX.
4
●
Heme is the prosthetic group for hemoglobin (Hb), myoglobin,
the cytochromes, the cytochrome P450 (CYP) monooxygenase
system, catalase, nitric oxide synthase, and peroxidase.
●
These hemeproteins are rapidly synthesized and degraded.
●
6–7 g of Hb is synthesized each day to replace heme lost
through the normal turnover of erythrocytes.
●
The synthesis and degradation of the associated porphyrins and
recycling of the iron are coordinated with the turnover of
hemeproteins.
5
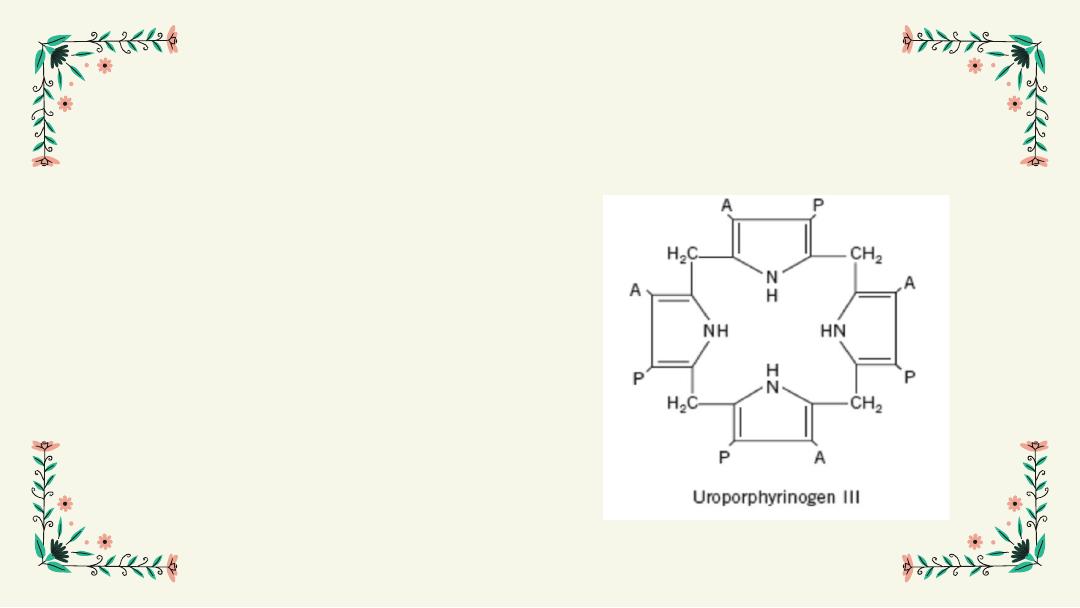
Structure of Porphyrin
Porphyrins are cyclic planar
molecules formed by the linkage
of four pyrrole rings through
methenyl bridges
6

Heme biosynthesis
7
●
The major sites of heme biosynthesis are the
liver
, which synthesizes a
number of heme proteins (particularly the cytochrome P450 proteins), and
the
erythrocyte-producing cells of the bone marrow
, which are active in
Hb synthesis.
●
In the liver, the rate of heme synthesis is
highly variable
, responding to
alterations in the cellular heme pool caused by fluctuating demands for
hemeproteins.
●
In contrast, heme synthesis in erythroid cells is relatively
constant
and is
matched to the rate of globin synthesis.
●
Over 85% of all heme synthesis occurs in erythroid tissue.
●
In erythroid cells, heme synthsis is controlled by erythropoietin and the
availability of intracellular iron
8
The initial reaction and the last
three steps in the formation of
porphyrins occur in mitochondria,
whereas the intermediate steps of
the biosynthetic pathway occur in
the cytosol.
Mature red blood cells (RBC)
lack mitochondria and are unable
to synthesize heme.
9
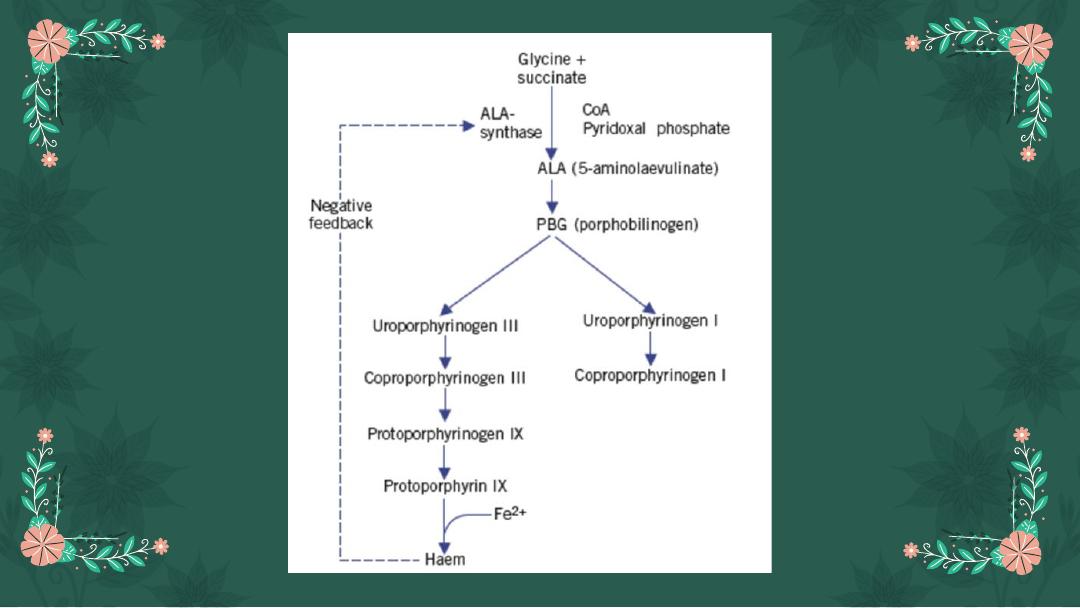
Heme (hemin) effects
●
When porphyrin production exceeds the availability of the apoproteins
that require it, heme accumulates and is converted to hemin by the
oxidation of Fe²⁺ to Feᵌ⁺
●
Hemin decreases the amount (and, thus, the activity) of ALA synthase
by repressing transcription of its gene, increasing degradation of its
mRNA, and decreasing import of the enzyme into mitochondria.
11

Porphyrias
●
Porphyrias are a rare group of inherited (or sometimes acquired)
defects of haem synthesis,
●
Caused by deficiency of one of the enzymes of the haem synthetic
pathway resulting in the accumulation and increased excretion of
porphyrins or porphyrin precursors
●
Each porphyria results in the accumulation of a unique pattern of
intermediates caused by the deficiency of an enzyme in the heme
synthetic pathway.
●
Porphyria, derived from the Greek for purple, refers to the red-blue
color caused by pigment-like porphyrins in the urine of some patients
with defects in heme synthesis.
13
Clinical manifestations
●
The porphyrias are classified as
erythropoietic or hepatic
, depending
on whether the enzyme deficiency occurs in the erythropoietic cells of
the bone marrow or in the liver.
●
Hepatic porphyrias can be further classified as acute or chronic.
●
Individuals with an enzyme defect leading to the accumulation of
tetrapyrrole intermediates show photosensitivity—that is, their skin
itches and burns when exposed to visible light.
14
a
.Chronic porphyria: Porphyria cutanea tarda
●
the most common porphyria, is a chronic disease of the liver and
erythroid tissues.
●
The disease is associated with a deficiency in
uroporphyrinogen
decarboxylase,
but clinical expression of the enzyme deficiency is
influenced by various factors, such as hepatic iron overload, exposure
to sunlight, and the presence of hepatitis B or C, or HIV infections.
●
Clinical onset is typically during the fourth or fifth decade of life.
●
Porphyrin accumulation leads to cutaneous symptoms , and urine that
is red to brown in natural light , and pink to red in fluorescent light.
15
b.
Acute hepatic porphyrias:
●
(acute intermittent porphyria, hereditary coproporphyria, and variegate
porphyria) are characterized by acute attacks of gastrointestinal,
neurologic/psychiatric, and cardiovascular symptoms.
●
This type lead to accumulation of
ALA and porphobilinogen.
16
c.
Erythropoietic porphyrias:
●
(congenital erythropoietic porphyria and erythropoietic
protoporphyria) are characterized by skin rashes and blisters
that appear in early childhood.
17
18
Thank you
