Lecture -9-
Anatomy of the liver , gall
bladder and biliary tree
Dr.Raya Abdul Ameer
MBCHB.CABHS/RAD

The Liver
The liver is a peritoneal organ
positioned in the right upper
quadrant of the abdomen. It is the
largest visceral structure in the
abdominal cavity , and the largest
gland in the human body.
An accessory digestion gland, the liver
performs a wide range of functions,
such as synthesis of bile, glycogen
storage and clotting factor production.
• Location :
• Rt upper abdomen
• Beneath diaphragm
• Under cover of Rt. Costal margin
• Under cover of Rt. Hemi diaphragm, which separates it
from :
1. Pleura
2. Lungs
3. Pericardium
4. Heart
• Extends to under cover of Lt. hemi diaphragm

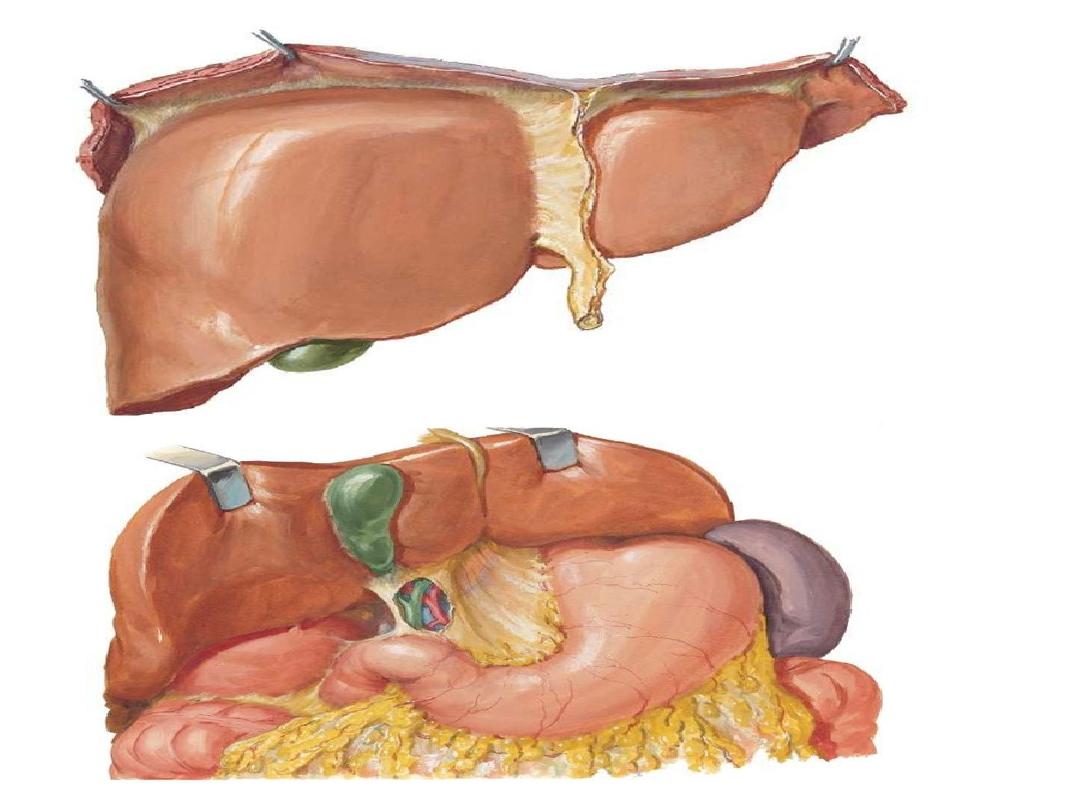
• Liver Surfaces
The external surfaces of the liver are described by their
location and adjacent structures. There are two liver surfaces –
the diaphragmatic and visceral:
• Diaphragmatic surface
– the anterosuperior surface of the
liver.
•
It is smooth and convex, fitting beneath the curvature of
the diaphragm.
•
The posterior aspect of the diaphragmatic surface is not covered by
visceral peritoneum, and is in direct contact with the diaphragm itself
(known as the ‘bare area’ of the liver).
• Visceral surface
– the posteroinferior surface of the liver.
•
With the exception of the fossa of the gallbladder and porta hepatis,
it is covered with peritoneum.
•
It is moulded by the shape of the surrounding organs, making it
irregular and flat.
•
It lies in contact with the right kidney, right adrenal gland, right colic
flexure,
transverse
colon,
first
part
of
the
duodenum, gallbladder, oesophagus and the stomach.

Ligaments of the Liver
There are a number of ligaments that attach the liver to the surrounding
structures. These are formed by a double layer of peritoneum.
• Falciform ligament
– this sickle-shaped ligament attaches the
anterior surface of the liver to the anterior abdominal wall. Its free
edge contains the ligamentum teres, a remnant of the umbilical vein.
• Coronary ligament (anterior and posterior folds
) – attaches the
superior surface of the liver to the inferior surface of the diaphragm
and demarcates the bare area of the liver The anterior and posterior
folds unite to form the triangular ligaments on the right and left lobes
of the liver.
• Triangular ligaments (left and right):
•
The left triangular ligament is formed by the union of the anterior
and posterior layers of the coronary ligament at the apex of the
liver and attaches the left lobe of the liver to the diaphragm.
•
The right triangular ligament is formed in a similar fashion adjacent
to the bare area and attaches the right lobe of the liver to the
diaphragm
.

• Lesser omentum
– Attaches the liver to
the lesser curvature of the stomach and
first part of the duodenum. It consists of
the hepatoduodenal ligament (extends
from the duodenum to the liver) and the
hepatogastric ligament (extends from the
stomach to the liver). The hepatoduodenal
ligament surrounds the portal triad.
• In addition to these supporting ligaments,
the posterior surface of the liver is secured
to the inferior vena cava by hepatic veins
and fibrous tissue.

• The ligamentum. teres
passes into a fissure on the
visceral surface of the liver and joins the left branch of
the portal vein in the porta hepatis (
.
The ligamentum
venosum
,
a fibrous band that is
the remains of the ductus venosus, Is attached to the
left branch of the portal vein and ascends In a fissure
on the visceral surface of the liver to attach above to
the
inferior vena cava .
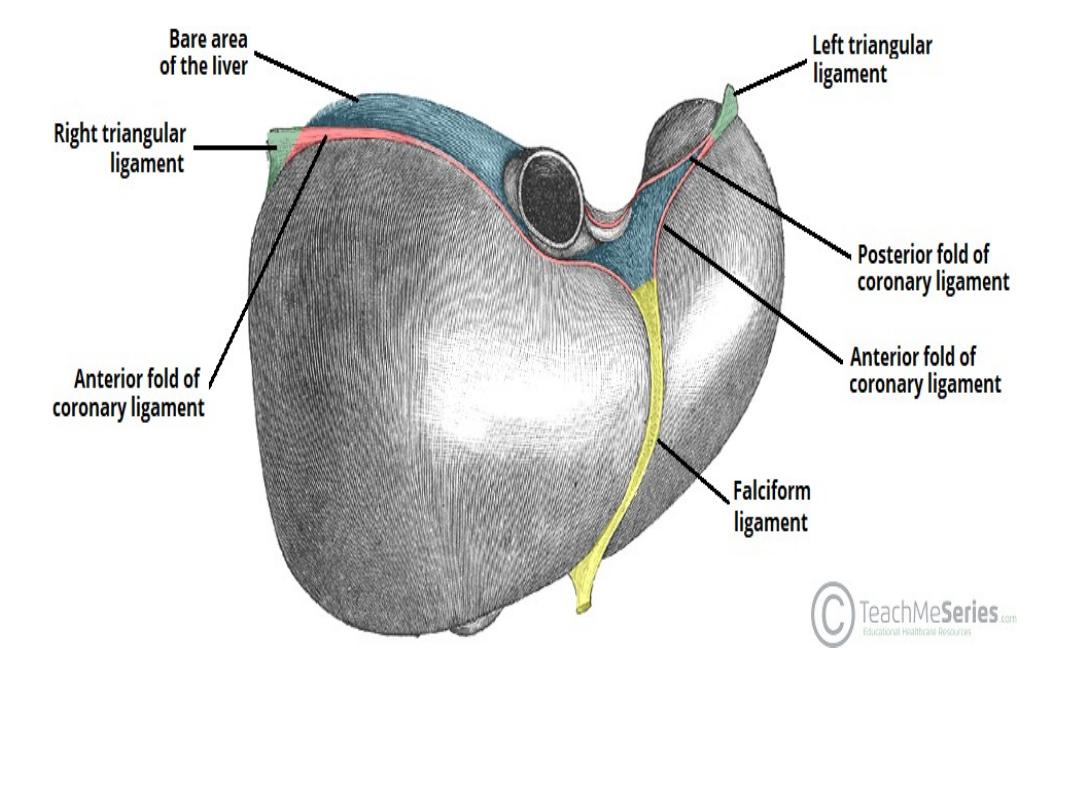
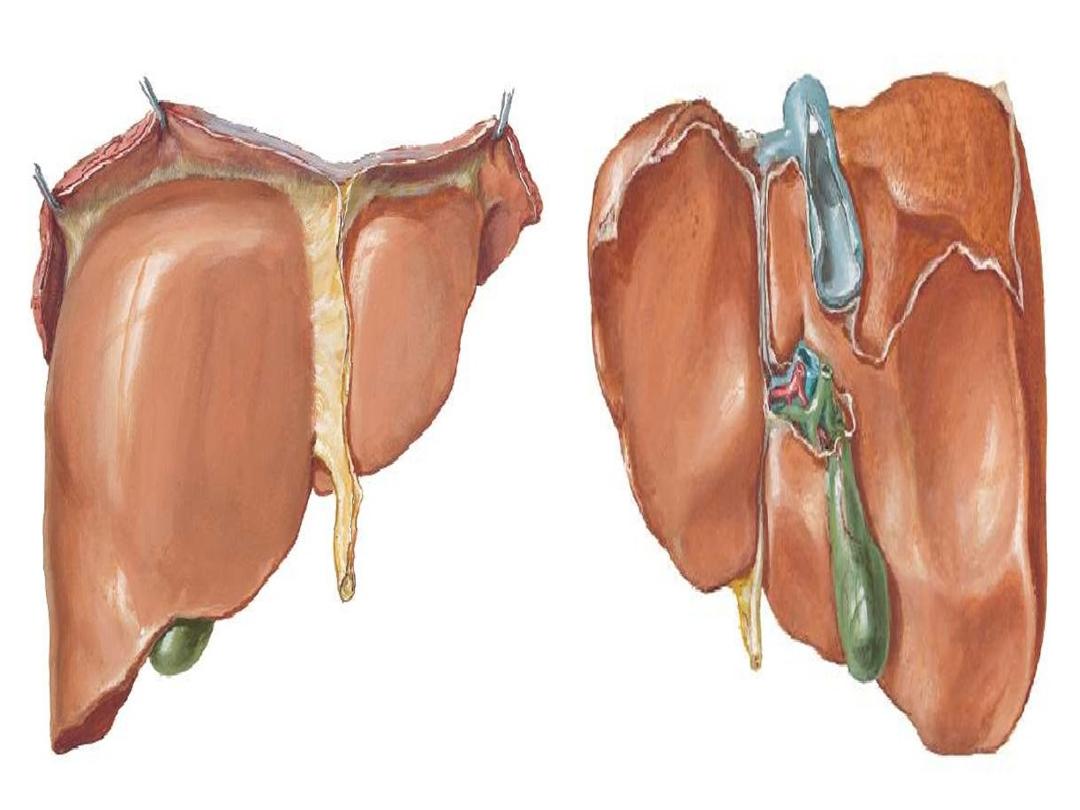
Diaphragmatic surface of the liver, demonstrating the three main
ligaments. The bare area of the liver lies between the anterior and
posterior folds of the coronary ligament.


Hepatic Recesses
The hepatic recesses are anatomical spaces between the
liver and surrounding structures. They are of clinical
importance as infection may collect in these areas, forming
an abscess.
• Subphrenic spaces
– located between the diaphragm
and the anterior and superior aspects of the liver. They
are divided into a right and left by the falciform ligament.
• Subhepatic space
– a subdivision of the supracolic
compartment (above the transverse mesocolon), this
peritoneal space is located between the inferior surface
of the liver and the transverse colon.
• Morison’s pouch
– a potential space between the
visceral surface of the liver and the right kidney. This is
the deepest part of the peritoneal cavity when supine
(lying flat), therefore pathological abdominal fluid such as
blood or ascites is most likely to collect in this region in a
bedridden patient.
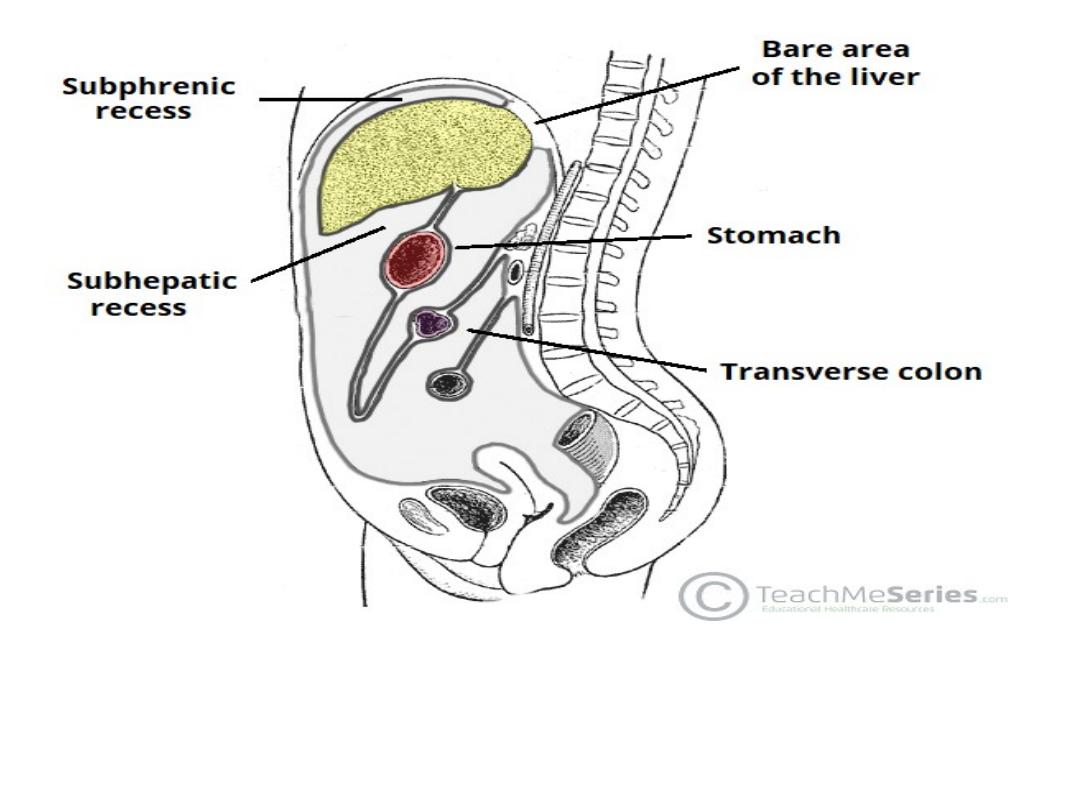
The subphrenic and subhepatic recesses. Note the bare area of
the liver

Anatomical Structure
• Macroscopic
• The liver is covered by a fibrous layer, known as Glisson’s
capsule. It is comprised of a large right lobe and smaller left
lobe.
• There are two further ‘accessory‘ lobes that arise from the
right lobe, which are located on the visceral surface of liver:
• Caudate lobe
– located on the upper aspect of the visceral
surface. It lies between the inferior vena cava and a fossa
produced by the ligamentum venosum (a remnant of the fetal
ductus venosus).
• Quadrate lobe
– located on the lower aspect of the visceral
surface. It lies between the gallbladder and a fossa produced by
the ligamentum teres (a remnant of the fetal umbilical vein).
• Separating the caudate and quadrate lobes is a deep,
transverse fissure – known as the porta hepatis. It transmits
all the vessels, nerves and ducts entering or leaving the liver
with the exception of the hepatic veins
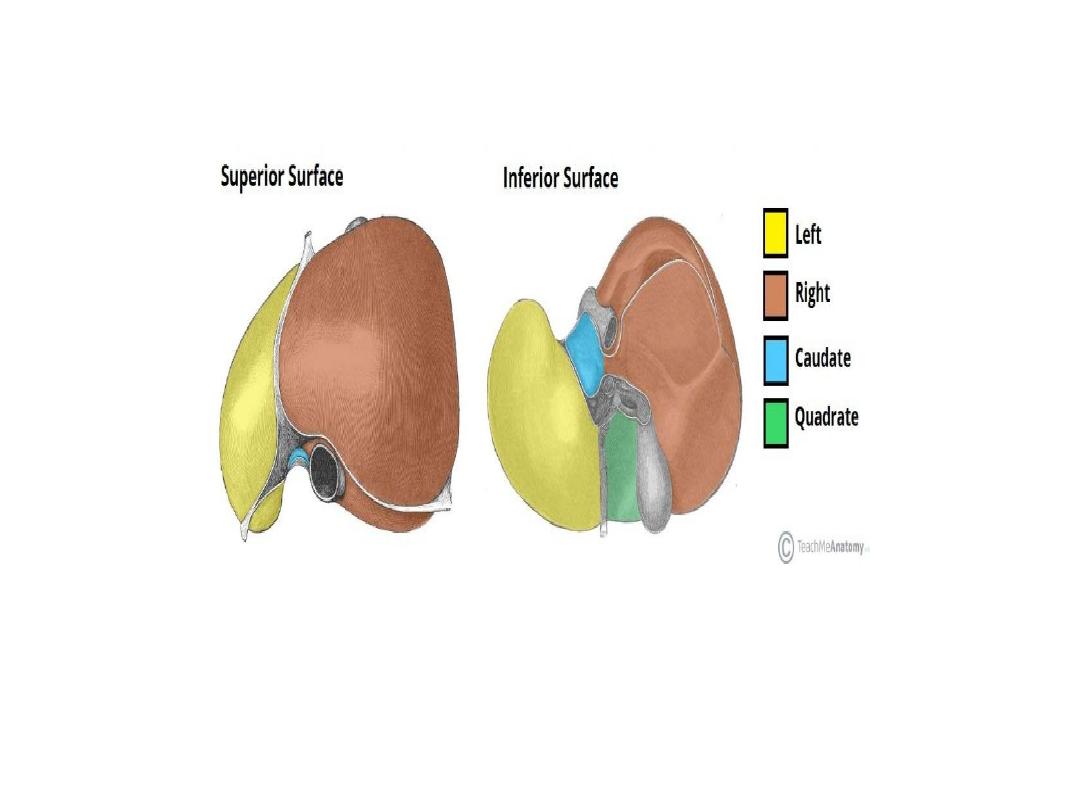
The anatomical lobes of the liver.


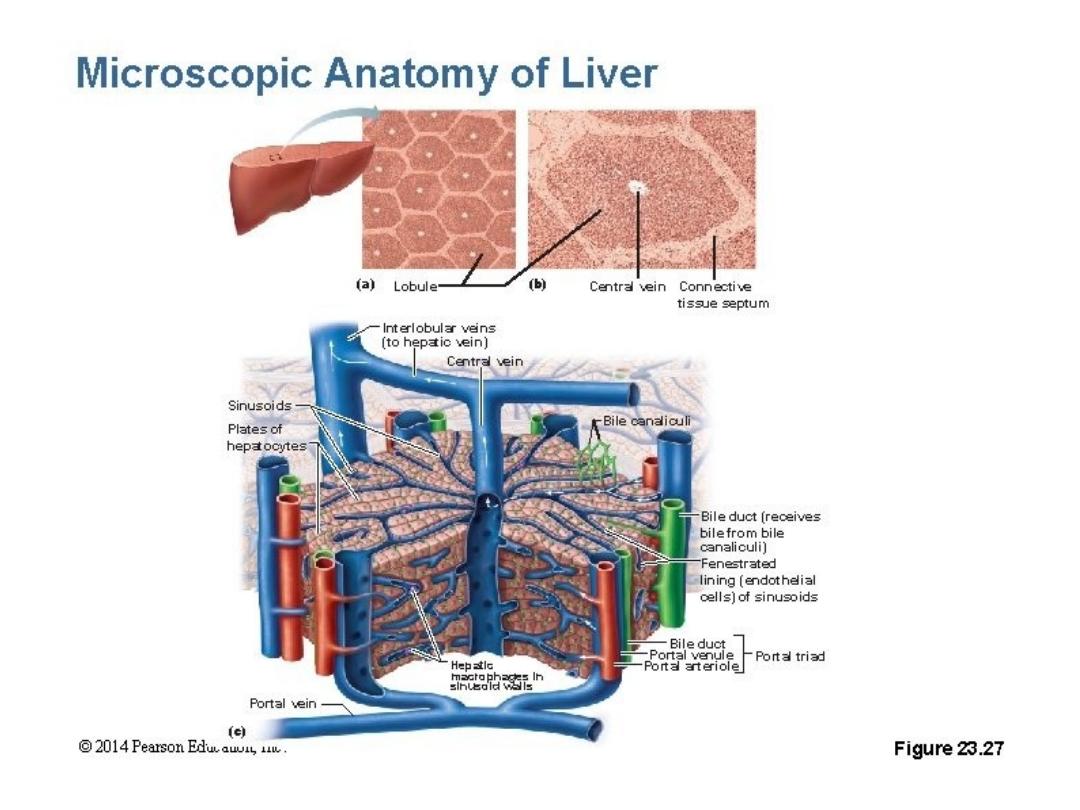
Microscopic
• Microscopically, the cells of the liver (known as
hepatocytes) are arranged into lobules. These are
the structural units of the liver.
• Each anatomical lobule is hexagonal-shaped and is
drained by a central vein. At the periphery of the
hexagon are three structures collectively known as
the portal triad:
• Arteriole – a branch of the hepatic artery entering
the liver.
• Venule – a branch of the hepatic portal vein
entering the liver.
• Bile duct – branch of the bile duct leaving the liver.
• The
portal
triad
also
contains lymphatic
vessels and vagus
nerve (parasympathetic)
fibres.

Important Relations
•
Anteriorly
: Diaphragm, right and left costal
margins, right and left pleura and lower
margins of both lungs, xiphoid process, and
anterior abdominal wall in the subcostal angle.
•
Posteriorly
: Diaphragm, right kidney, hepatic
flexure of the colon, duodenum, gallbladder,
Inferior vena cava, and esophagus and fundus
of the stomach.

Vasculature
The liver has a unique dual blood supply:
• Hepatic artery proper (25%) – supplies the non-
parenchymal structures of the liver with arterial
blood. It is derived from the celiac trunk .
• Hepatic portal vein (75%) – supplies the liver with
partially deoxygenated blood, carrying nutrients
absorbed from the small intestine. This is the
dominant blood supply to the liver parenchyma, and
allows the liver to perform its gut-related functions,
such as detoxification.
• Venous drainage of the liver is achieved through
hepatic veins. The central veins of the hepatic lobule
form collecting veins which then combine to form
multiple hepatic veins. These hepatic veins then open
into the inferior vena cava.
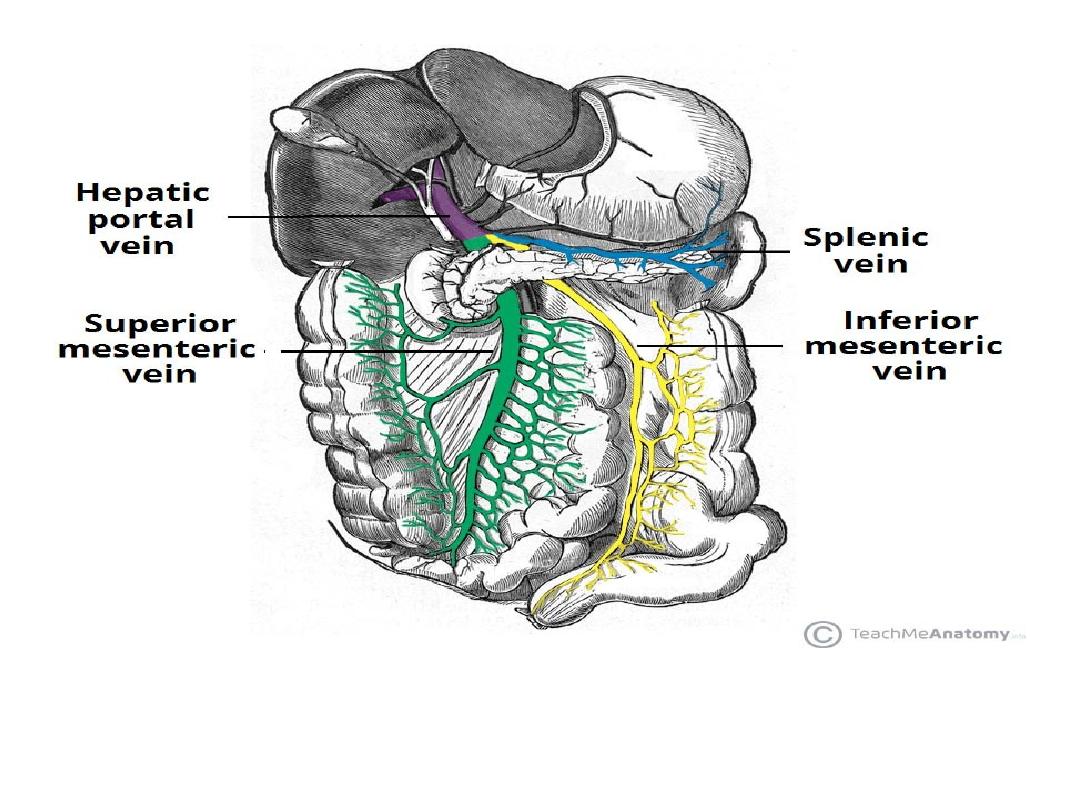
An overview of the venous portal system – draining into the
hepatic portal vein.
Nerve Supply
• The parenchyma of the liver is innervated by the hepatic plexus, which
contains sympathetic (coeliac plexus) and parasympathetic (vagus nerve)
nerve fibres. These fibres enter the liver at the porta hepatis and follow the
course of branches of the hepatic artery and portal vein.
• Glisson’s capsule, the fibrous covering of the liver, is innervated by branches
of the lower intercostal nerves. Distension of the capsule results in a sharp,
well localised pain.
Lymphatic Drainage
• The lymphatic vessels of the anterior aspect of the liver drain
into hepatic lymph nodes. These lie along the hepatic
vessels and ducts in the lesser omentum, and empty in the
colic lymph nodes which in turn, drain into the cisterna chyli.
• Lymphatics from the posterior aspect of the liver drain
into phrenic and posterior mediastinal nodes, which join
the right lymphatic and thoracic ducts.

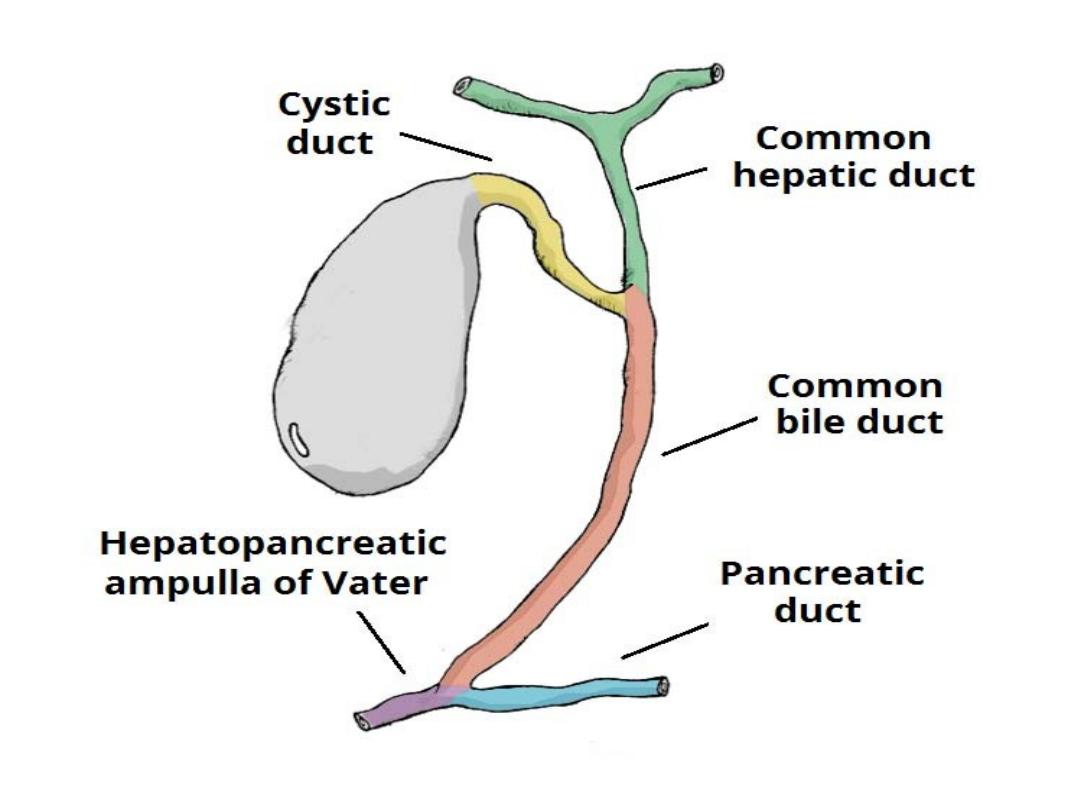
Biliary Tree
• The biliary tree is the system of ducts that drain and store bile and
deliver bile to the small intestine.
• Bile is secreted by the liver cells at a constant rate of about 40 mL per
hour. When digestion is not taking place,
• the bile is stored and concentrated in the gallbladder;
• later, it is delivered to the duodenum.
• The biliary tree consists of the right and left hepatic ducts, the common
hepatic duct, the bile duct, the gallbladder, and the cystic duct.
• The smallest interlobular tributaries of the bile ducts are situated in the
portal canals of the liver; they receive the bile canaliculi. The
interlobular ducts join one another to form progressively larger ducts
and eventually, at the porta hepatis, form the right and left
hepatic ducts.
• The right hepatic duct drains the right lobe of the liver and the left
duct drains the left lobe, caudate lobe, and quadrate lobe.

• Hepatic Ducts
• The right and left hepatic ducts emerge from the
right and left lobes of the liver in the porta hepatis
• After a short course, the hepatic ducts unite to
form the common hepatic duct
The common hepatic duct is about 1.5 in. (4 cm)
long and descends within the free margin of the
lesser omentum. It is joined on the right side by the
cystic duct from the gallbladder to form the common
bile duct.

Bile Duct
• The bile duct (common bile duct) is about 3 in. (8 cm)
long.
In the first part of its course
, it lies in the right free
margin of the lesser omentum in front of the opening into
the lesser sac. Here, it lies infront of the right margin of
the portal vein and on the right of the hepatic artery
In the second part of its course
, it is situated behind the
first part of the duodenum to the right of the
gastroduodenal artery . In the third part of its course, it
lies in a groove on the posteriorsurface of the head of the
pancreas Here, the bile duct comes into contact with the
main pancreatic duct.

The bile duct ends below by piercing the medial wall of the
second part of the duodenum about halfway down its
length
The main pancreatic duct usually joins it, and together,
they open into a small ampulla in the duodenal wall called
the hepatopancreatic ampulla (ampulla of Vater).
• The ampulla opens into the lumen of the duodenum by
means of a small papilla, the major duodenal papllla. The
terminal parts of both ducts and the ampulla are
surrounded by
circular muscle, known as the sphincter of
the hepatopancreatic ampulla (sphincter of Oddi).
• Occasionally,the bile and pancreatic ducts open
separately into the duodenum.
• Gallbladder
• The gallbladder is a pear-shaped sac lying on the
undersurface of the liver
• It has a capacity of 30 to 50 mL and
• stores bile, which it concentrates by absorbing water.
• The gallbladder is divided into the fundus, body, and
neck
The fundus
is rounded and projects below the inferior margin
of the liver,where it comes in contact with the anterior
abdominal wall at the level of the tip of the ninth right costal
cartilage.
• The body
lies in contact with the visceral surface of the
liver and is directed upward, backward, and to the left.
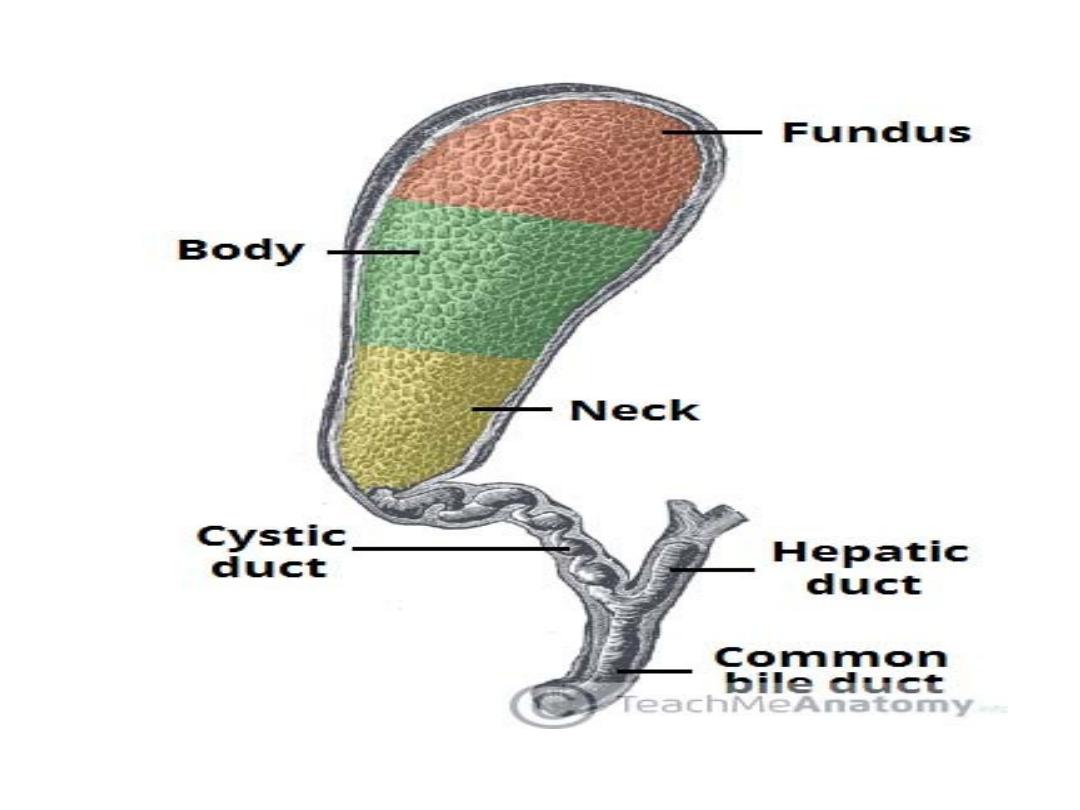

• The neck
becomes continuous with the cystic
duct, which turns into the lesser omentum to join
the common hepatic duct, to form the bile duct.
• The peritoneum completely surrounds the
fundus of the gallbladder and binds the body
and neck to the visceral surface of the liver.

• Relations
• Anteriorly and superiorly
– inferior
border of the liver and the anterior
abdominal wall
• Posteriorly
– transverse colon and
the proximal duodenum .
• Inferiorly
–
biliary
tree
and
remaining parts of the duodenum

• Blood Supply
• The cystic artery, a branch of the right hepatic artery
supplies the gallbladder.
• The cystic vein drains directly into the portal vein.
• Several very small arteries and veins also run between the liver and
gallbladder
• Lymph
Drainage
• The lymph drains into a cystic lymph node situated near the neck of
the gallbladder. From here, the lymph vessels pass to the hepatic
nodes along the course of he hepatic artery and then to the celiac
nodes.
• Nerve
Supply
• Sympathetic and parasympathetic vagal fibers form the celiac plexus.
The gallbladder contracts in response to the hormone cholecystokinin,
which is produced by the mucous membrane of the duodenum on the
arrival of fatty food from the stomach

• Cystic Duct
• The cystic duct is about 1.5 in. (3.8 c m) long and connects the
neck of the gallbladder to the common
hepatic duct to form the bile duct
• It usually is somewhat S-shaped and descends for
a variable distance in the right free margin of the lesser
omentum.
• The mucous membrane of the cystic duct is raised
to form a spiral fold that is continuous with a similar
fold in the neck of the gallbladder. The fold is commonly
known as the spiral valve.
The function of the spiral valve is to keep the lumen constantly
open.
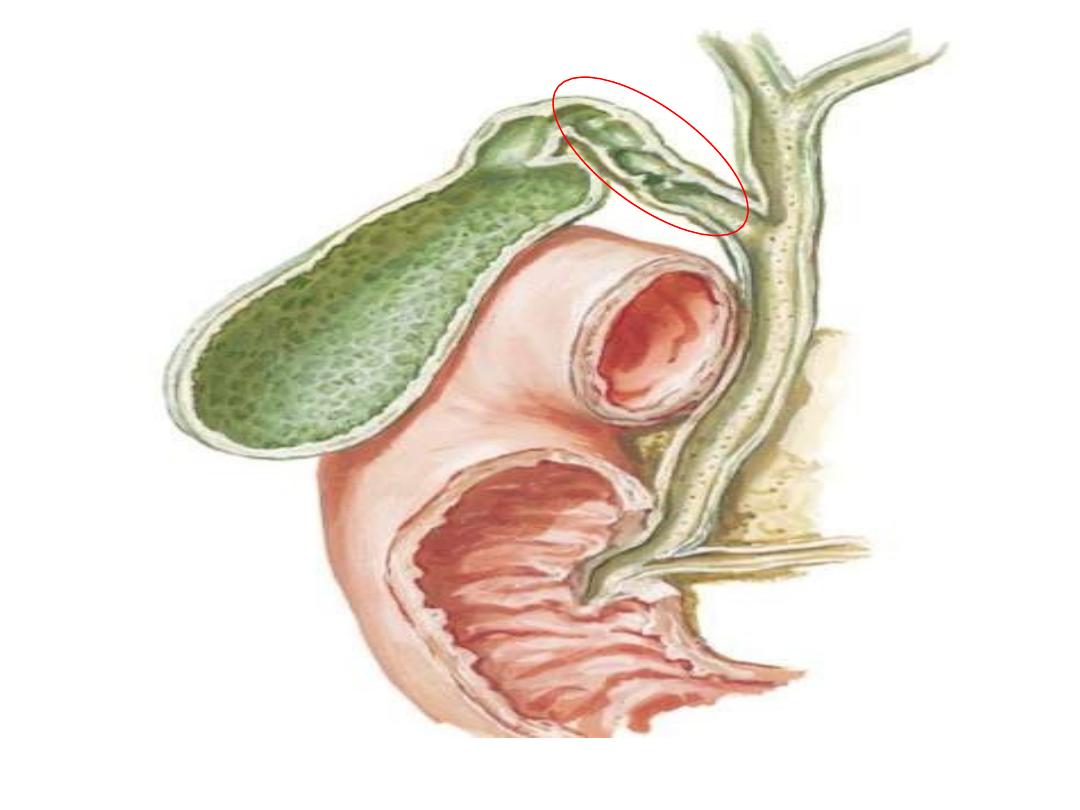

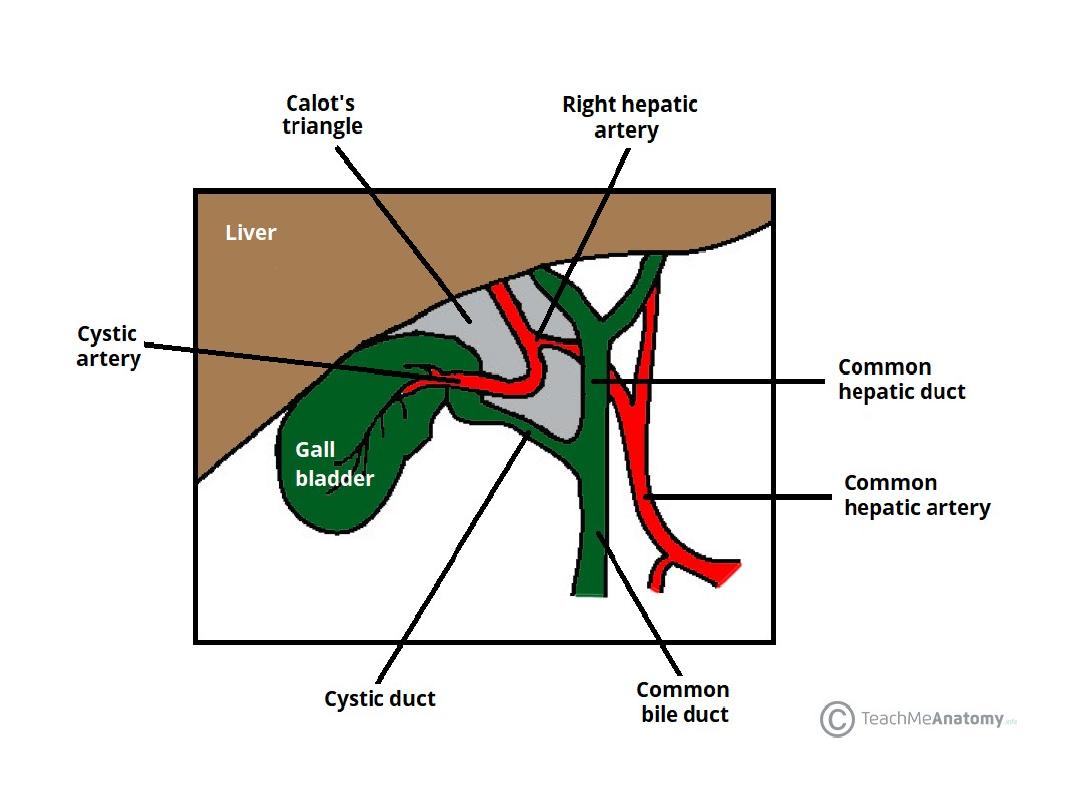
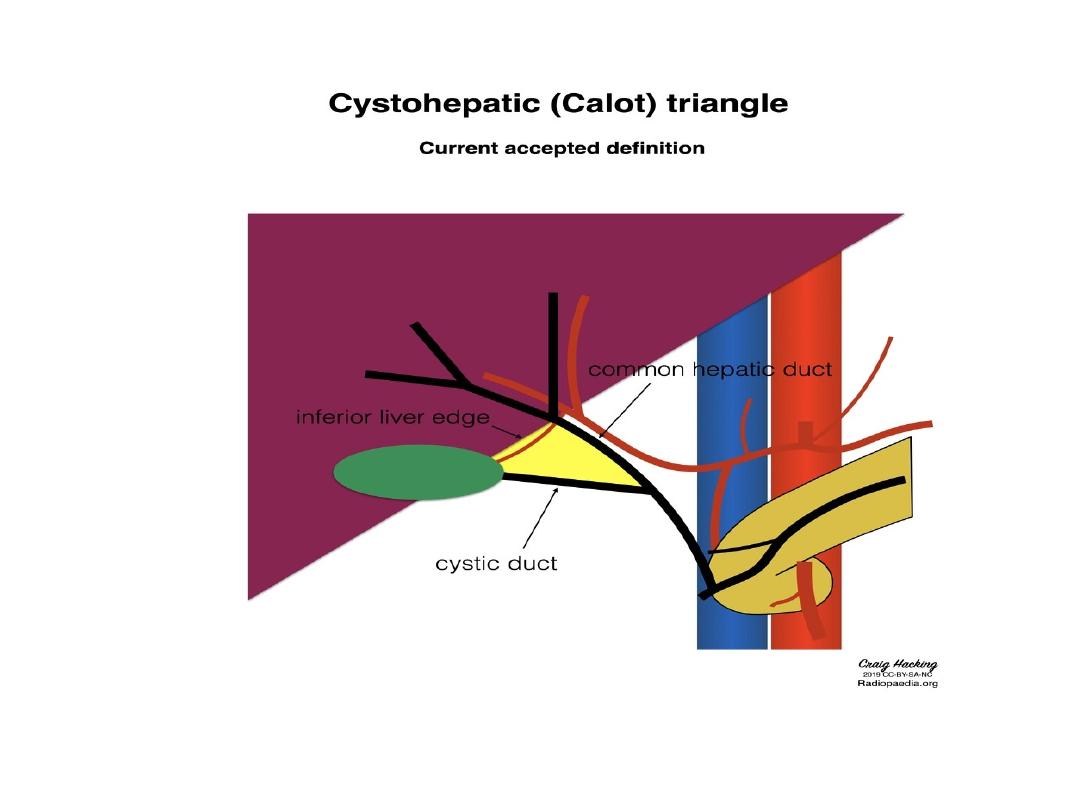
• Calot’s
triangle (cystohepatic
triangle) is a small anatomical space
in the abdomen.
• It is located at the porta hepatis of
the liver – where the hepatic ducts
and
neurovascular
structures
enter/exit the liver.

• Borders
• Calot’s triangle is orientated so that its apex is
directed at the liver. The borders are as follows:
• Medial – common hepatic duct.
• Inferior – cystic duct.
• Superior – inferior surface of the liver.
• The above differ from the original description of
Calot’s triangle in 1891 – where the cystic
artery is given as the superior border of the
triangle. The modern definition gives a more
consistent border (the cystic artery has
considerable variation in its anatomical course
and origin).

• Contents
• The contents of the Calot’s triangle
include:
• Right hepatic artery – formed by the
bifurcation of the proper hepatic artery into
right and left branches.
• Cystic artery – typically arises from the
right hepatic artery and traverses the
triangle to supply the gall bladder.
• Lymph node of Lund – the first lymph
node of the gallbladder.
• Lymphatics

• The triangle of Calot is of clinical importance
during laparoscopic cholecystectomy (removal
of the gall bladder).
• In this procedure, the triangle is carefully
dissected by the surgeon, and its contents and
borders identified. This allows the surgeon to
take into account any anatomical variation and
permits safe ligation and division of the cystic
duct and cystic artery.