Lecture 5
Dr. Suroor Mohamed

Objectives :
1-Describe the muscle metabolism process?
2- Discuss the muscle fatigue ? How is done?
3- Types of muscle contraction ?

Muscle Cell Metabolism
Source of ATP:ATP are Available in the sarcoplasm, Creatine phosphate, Glucose
*** Cells store glucose in the sarcoplasm in the form of glycogen. The cell must break apart
the glycogen molecules to release the individual glucose molecules this is called
glycogenolysis
***The breakdown of glucose, called
glycolysis,
occurs in the sarcoplasm of the muscle cell
and does not require oxygen, it is anaerobic. Glycolysis produces pyruvic acid, and a small
amount of ATP.
The majority of the ATP used by muscles is formed by aerobic processes in the mitochondria,
the muscle cell depends on aerobic glycolysis during which oxidative phosphorylation
becomes more important
*** During intense exercise, when the supply of oxygen cannot keep up with metabolic
demand of the cells, pyruvic acid produced during glycolysis is converted to lactic acid.
Lactic acid accumulates in the muscle resulting in the burning sensation during short
duration,high intensity muscular exercise such as lifting weights.
Lactic acid is quickly removed from the muscle and taken to the liver where it is converted
to glucose.

Muscle disorders
Muscle hypertrophy
results from an increase in the number of actin and myosin
filaments in each muscle fiber. When the number of contractile proteins increases
sufficiently, the myofibrils split within each muscle fiber to form new myofibrils. It is
mainly this great increase in the number of additional myofibrils that causes muscle
fibers to hypertrophy not increase in number of muscle fibers (muscle cells).
Muscle atrophy
When a muscle remains unused for a long period, the rate of decay
of the contractile proteins occurs more rapidly
than the rate of replacement
؛
therefore muscle atrophy occurs.
Atrophy begins almost immediately when a muscle loses its nerve supply because it
no longer receives the contractile signals that are required to maintain normal muscle
size.

subjective sensation of the feeling of tiredness after prolonged activity, where the muscles are
unable to contract forcefully, The movements will be jerky instead of being smooth
Caused by changes occurring in the muscle fibers , Severe cases →muscle damage
Fast muscles fatigued more easily but posture controlling muscles get fatigued very
slowly Not all motor units in the muscle are stimulated at the same time , Alternately
contracting motor units delays muscle fatigue , Called asynchronous muscle contraction and this
helps in the sustained contraction of postural muscles
Muscle fatigue: causes
Nerve
Continuous stimulation of brain by impulses from muscle causing neuronal fatigue
Neuromuscular junction
Inadequate release of Ach at the neuromuscular junction
Muscle
Depletion of ATP and creatine phosphate within muscle fibers
Depletion of nutrients like glycogen
Inadequate release of Ca
2+
from the sarcoplasmic reticulum
Hypoxia
Acidosis due to increase in the lactic acid content (inhibits enzyme function)
Accumulation of K
+
(action potential)→ muscle fiber more excitable
Increase in temperature
Anticholinesterase
“ enzyme that destruct the Ach “
Reversible: physostigmine and neostigmine
Irreversible: Insecticides and nerve gas
Neuromuscular Blocking Drugs
Curare
Extracted from a plant (used by Red Indians → arrow poison)
Nondepolarizing block (D-tubocurarine-active princible)
High affinity for Ach receptor → no action → flaccid paralysis
Treatment by
Neostigmine →↑Ach
Botulinum toxin
Bacterial toxin (Clostridium botulinum) inhibits the release of Ach by
the nerve terminals → flaccid paralysis
الوهن العضلي
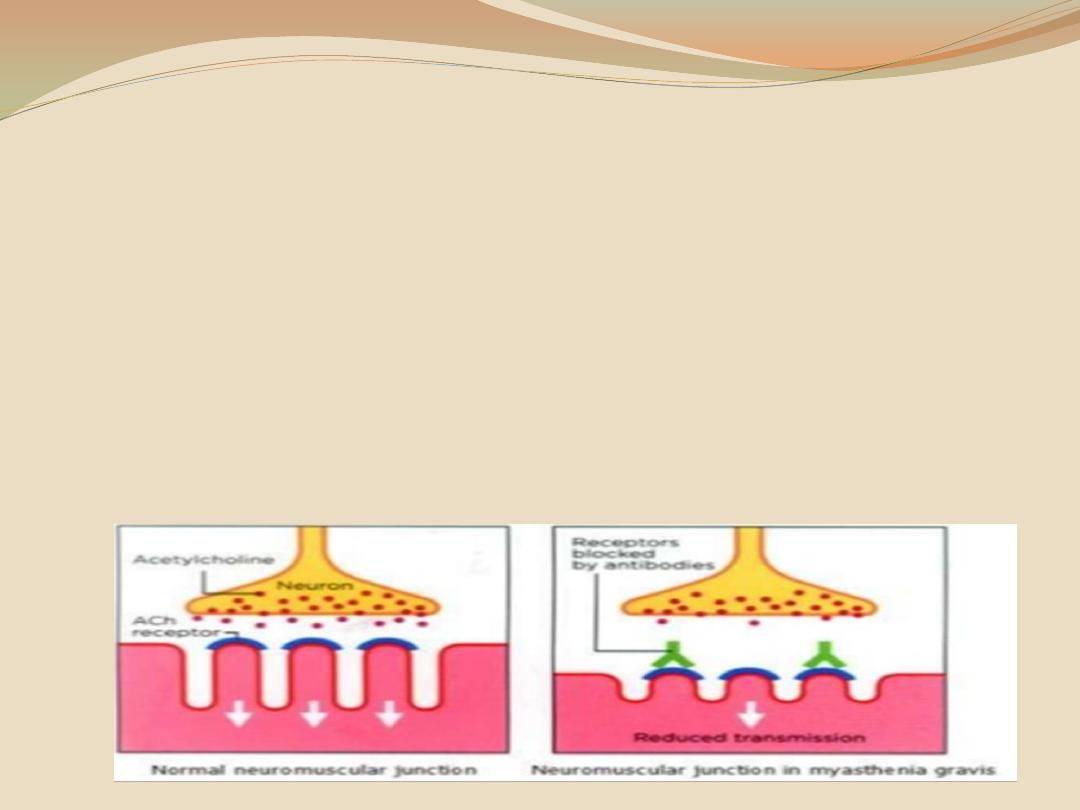
1-Myasthenia Gravis
Rare, serious and sometimes fatal disease (weakness & fatique)
Aetiology
:
Autoimmune disease
Antibodies which destroy the nicotinic Ach in NMJ , Antibodies (90% serum of patients)
Histologically, the number of subneuronal clefts is decreased and there is widening of the
synaptic cleft
In adults: 70% hyperplasia of thymus↑ thymic hormone → autoimmune response
Thymectomy is of benefit in these patients
Treatment
Neostigmine
High dose of cortisol

2-Lambert-Eaton Syndrome
Muscle weakness: autoantibodies against voltage-gated Ca
2+
channels in
the nerve ending at the neuromuscular junction
االرتجاف
1) Fibrillation
●
Abnormal excitability of the muscle (fine, irregular contractions of the
individual fibers)
Due to denervation hypersensitivity.
Seen for several weeks after injury and then ceases as the muscle cells
atrophy
Contractions are not visible (recorded by EMG using needle
electrodes)
Disappeared if the motor nerve regenerate
2) Fasciculation
These are jerky, visible contractions (twitching) of groups of muscle
fibers as a result of pathologic discharge of spinal motor neurons
It is seen in diseases affecting the anterior horn cells
For example, in poliomyelitis, the anterior horn cell is destroyed and there will
be spontaneous discharge of impulses causing fasciculation.
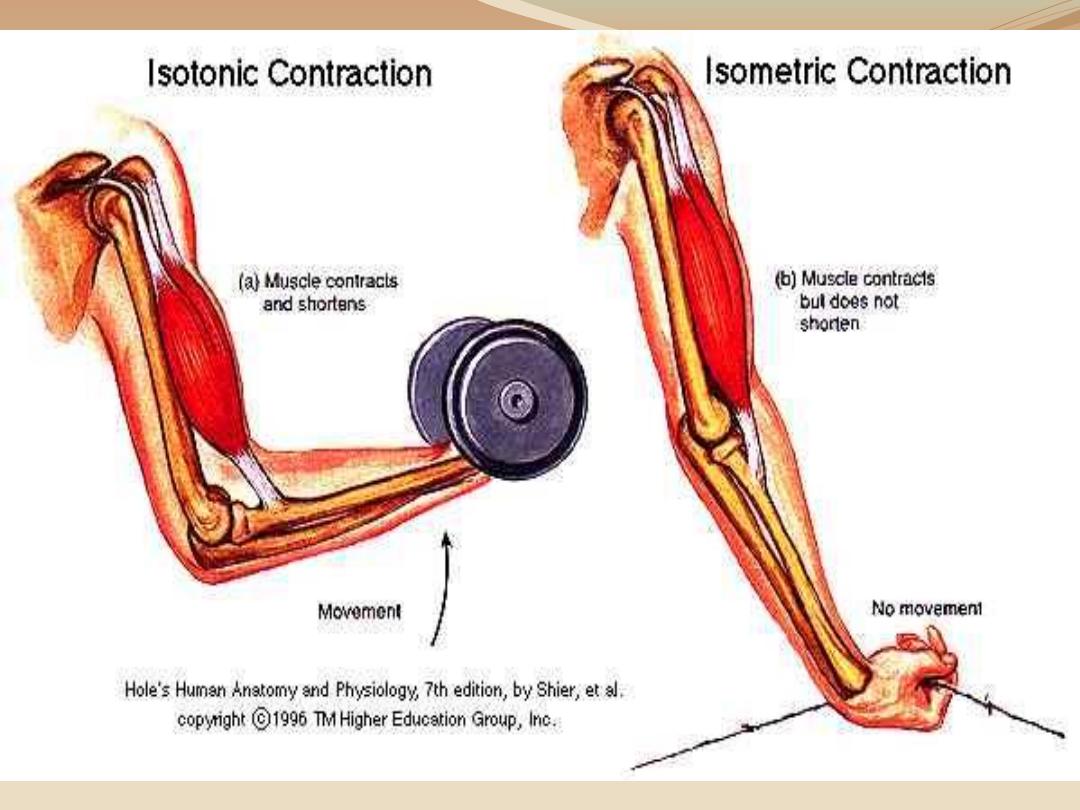
Isotonic contraction
Contraction of muscle with approximation of the ends of the muscle
(shortening of muscle) .This Contraction is usually against a constant load
Change in length of the muscle but tension remains constant
External work is done only in isotonic muscle contraction
Lifting a small weight by bending the elbow, the contraction of the
biceps muscle can be seen
Isometric contraction
Contraction of muscle without an appreciable decrease in the length of the
whole muscle
Length constant but the tension rises
Due to the formation of cross bridges between actin and myosin
The shortening produced by the contractile component is
compensated by the stretching of the series elastic component. So the
length does not change
No external work is done by the muscle but the muscle becomes hard, hot
and expends energy
Trying to lift a very heavy weight from the ground the muscle will not
shorten and the weight does not move, but the tension rises
considerably.
Differences between isotonic and isometric contraction
Isometric contraction
Isotonic contraction
1 No shortening of the muscle
Shortening of the muscle
2
No movement occurs
Movement
4 Tension in the muscle rises
No rise in tension in muscle
5 Shortening of the contractile
component is compensated
by stretching of the series
elastic component, so length
remains same
Shortening of contractile
component is not associated with
stretching of series elastic
component
6 Heat released is less
Heat released is more
3 No external work is done
External work is done

slow muscles
Number of muscle fibers per motor unit is high
All the units do not contract simultaneously (asynchronous contraction)
Gastrocnemius (2000-3000 muscle fibers in some motor units)
Not easily fatigued
These muscles are important in posture controlling
Red muscle (high myoglobin content, greater & large number of
mitochondria)
Fast muscles
In muscles concerned with fine, precise, graded movements
Only 3-6 fibers per motor unit
Muscles of larynx has only 2-3 muscle fibers per motor unit
Each spinal motor neuron innervates only one kind of muscle fiber
(muscle fibers in a motor unit are of the same type)
All the muscle fibers of a motor unit contract and relax together
Fibers not found together (dispersed throughout the muscle)
White
muscle (
low myoglobin content)
Types of skeletal muscles and muscle fibers

Muscle tone
Small amount of tension maintained in the muscles at
rest due to weak involuntary contraction of motor units
There is alternate contraction and relaxation of small groups
of motor units at rest and their activity is maintained by
neurons in the brain and spinal cord
Motor point:
Point on the skin which when stimulated
by an active electrode gives the maximum contraction of
the muscle
Area of entry of the nerve into the muscle
Neurovascular hilus: nerve and blood supply entery to a
muscle
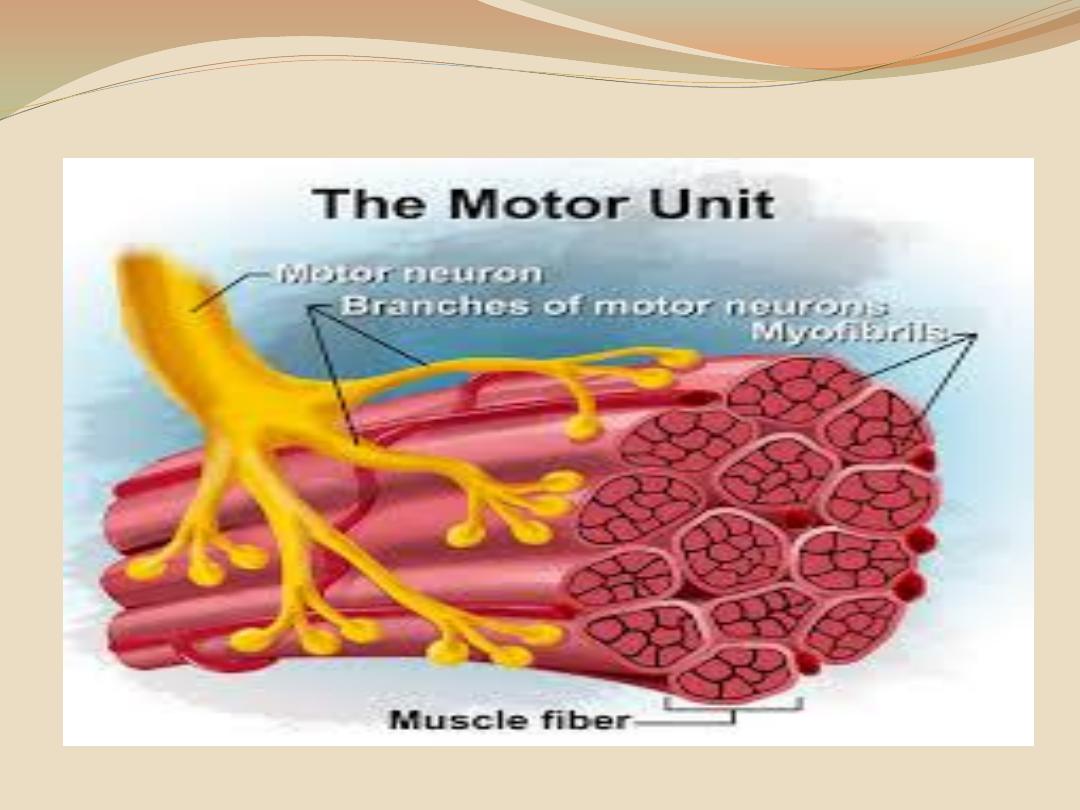
motor unit:
A single motor neuron with all the muscle
fibers supplied by its terminal branches