Immunology of organs
Tissues transplantation
Objectives
The objectives of this lecture are to know
1. The indications and methods of HLA-typing.
2. Preparations for transplantations.
3. Types of transplant rejection.
4. Graft Versus Host Disease.
Tissues transplantation
HLATyping
Indications:
1.Transplantation
2. Disease association
3. Paternity testing
4. Anthropological studies.
Methods used for HLA typing:
1. Serology: It is an antibody-antigen reaction based method using
monoclonal antibodies against the MHC antigens. It is quick and cheap,
but does not provide information about sequence variation in alleles and
incapable of detection of some differences in DR molecules.
Methods used for HLA typing:
2. Molecular PCR-based techniques: They depends either on amplifying
digested DNA, or labelled specific sequence by specific DNA probes for
detection of the DNA sequence of interest. They are more precise and
specific but needs well trained workers and highly sophisticated molecular
techniques and machines
lect:2
Dr. Khalid Waleed
M.B.ch.B., Msc., PhD. Immunology
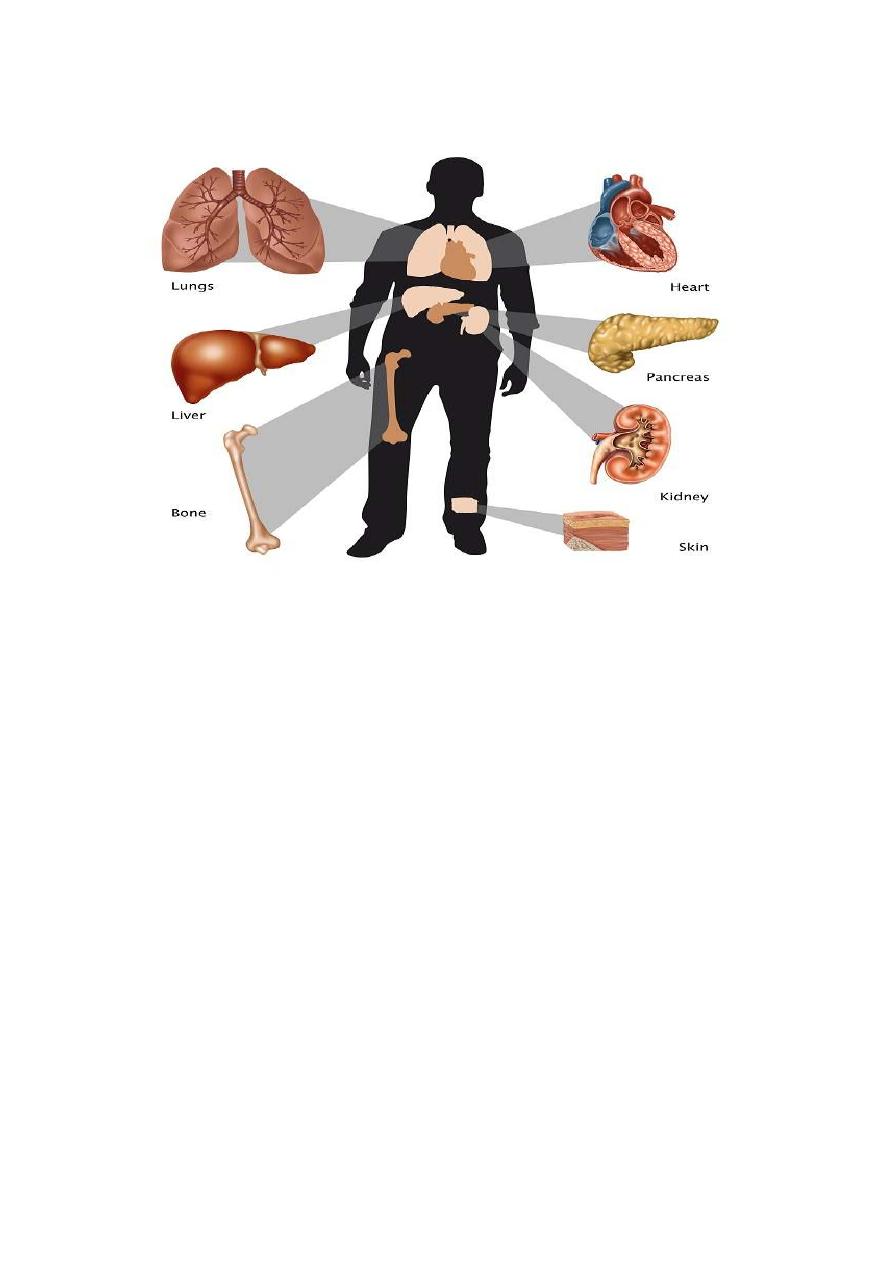
Organ transplantation
• Transplantation is the act of transferring cells, tissues, or organs
from one site to another.
• The malfunction of an organ system can be corrected with
transplantation of an organ (eg, kidney, liver, heart, lung, or
pancreas) from a donor.
•
The clinical era of transplantation began in 1954, when Dr. Joseph
Murray and colleagues performed the first successful renal transplant
on the genetically identical Herrick twins
• However, the immune system remains the most threatening barrier to
transplantation as a routine medical treatment.
• The immune system has developed effective mechanisms to fight
foreign agents. These mechanisms are involved in the rejection of
transplanted organs, which are recognized as foreign by the
recipient's immune system.
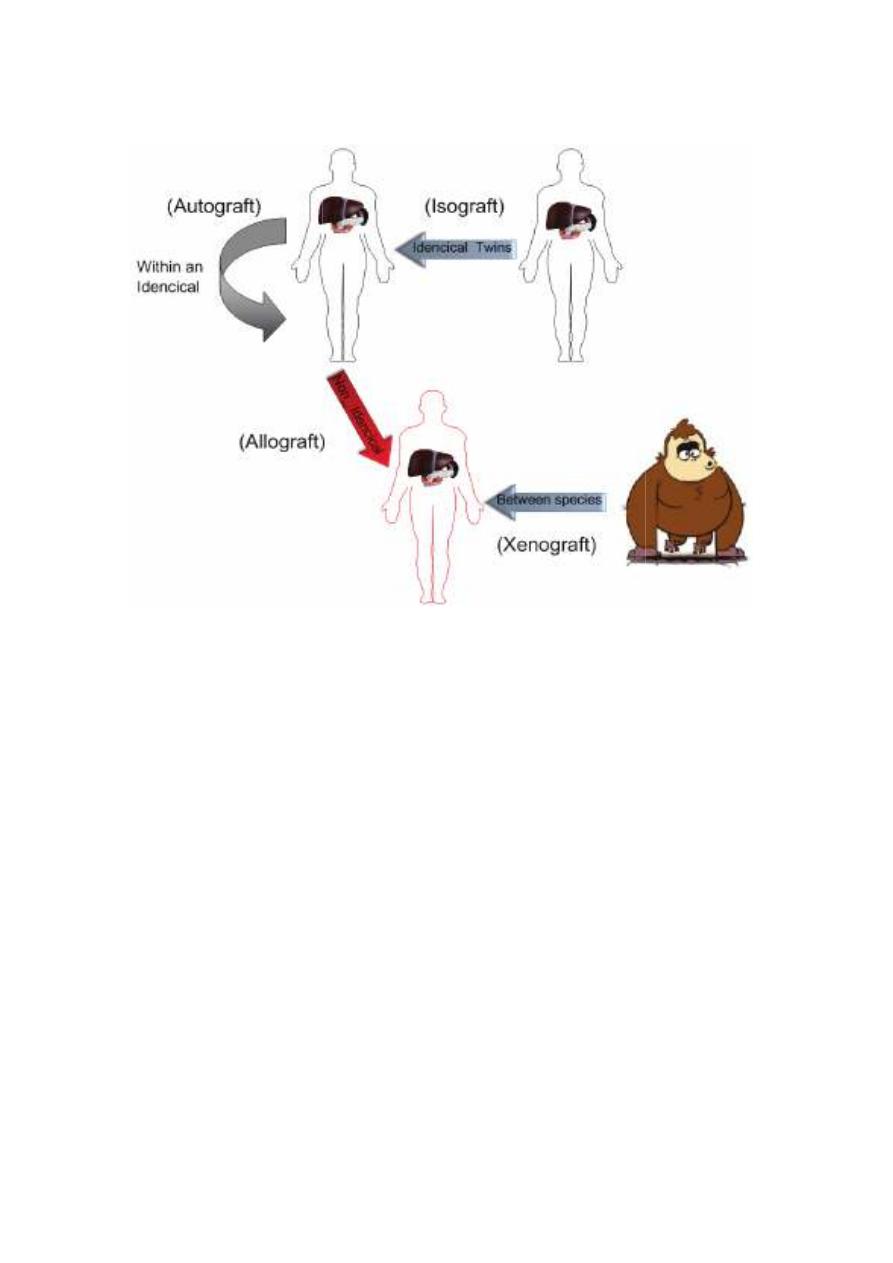
Types of transplant or graft
Preparations for transplantations
1. ABO & Rh compatibility test.
2. Screening for reaction between leuco
donor.
3. HLA typing; 2 loci compatibility as A & B preferably with DR.
4- Check the donor and the recipien
infections, which can be transmitted and /or reactivated
suppressive therapy.
5. Vaccination against common bacterial and viral diseases.
6. Antibiotics umbrella as penicillins or cephalosporins with
aminoglycosides specially the new ones.
7. Splenectomy is preferable.
8. Use of immunosuppressive a
Types of transplant or graft
Preparations for transplantations
1. ABO & Rh compatibility test.
for reaction between leucocytes of recipient and serum of
3. HLA typing; 2 loci compatibility as A & B preferably with DR.
Check the donor and the recipient to detect presence of dormant
infections, which can be transmitted and /or reactivated under immune
5. Vaccination against common bacterial and viral diseases.
6. Antibiotics umbrella as penicillins or cephalosporins with
aminoglycosides specially the new ones.
7. Splenectomy is preferable.
8. Use of immunosuppressive agents
cytes of recipient and serum of
3. HLA typing; 2 loci compatibility as A & B preferably with DR.
t to detect presence of dormant
under immune
6. Antibiotics umbrella as penicillins or cephalosporins with
Immunosuppressive Agents
Immunosuppressive therapy is used to prevent or treat graft rejection by
non-specifically interfering with the induction or expression of the
immune response. The following agents or measures are in use:
1. Immunosuppressive medicines:
A. Cyclosporine A is an antibiotic produced by a fungus. It prevents T
cells activation and blocks the accompanying cytokine production.
B. FK–506 (Tacrolimus) , rapamycin (Sirolimus) or Everolimus are
relatively new immunosuppressive drugs with action similar to
cyclosporine.
C. Corticosteroids are given in big doses; they act on blocking IL-1 & 2
release and cytokines receptor expression and suppressing macrophages.
D. Anti-mitotic medicines as Azathioprine and Methotrexate, which
inhibit DNA synthesis and block the growth of T cells.
All used in prevention, but Cortisones is also used in treatment.
2. Anti-lymphocyte or anti-thymocyte globulin or anti-CD3 monoclonal
antibodies. These agents lyse T cells and can block their functions. Used
in prevention and treatment.
3. Antibody to block co-stimulatory molecules.
4. Total lymphoid irradiation while shielding the marrow, lungs and other
vital organs before engraftment.
5. Antigen specific immunosuppression by induction of tolerance to the
graft antigen.
Transplant rejection
Mechanism of rejection
The immune response toward a transplanted organ consists of both
cellular (lymphocyte mediated) and humoral (antibody mediated)
mechanisms. Although other cell types are also involved, the T cells are
central in the rejection of grafts. The rejection reaction consists of
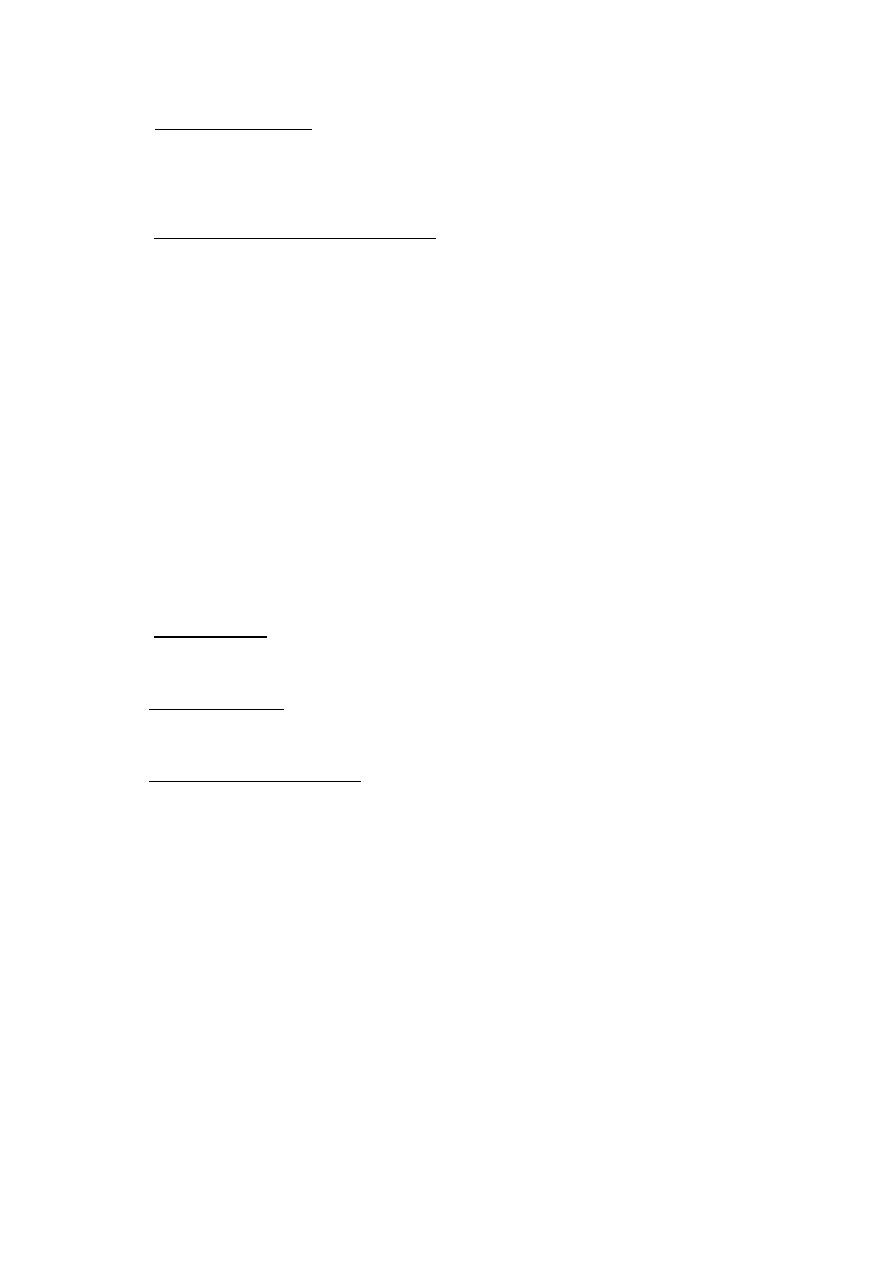
A- Sensitization stage
In this stage, the CD4 and CD8 T cells, via their T-cell receptors,
recognize the alloantigens expressed on the cells of the foreign graft.
B- Effector stage: this stage includes:
1- Induction of ischemia due to nonspecific inflammatory response
2-Induction of delayed type hypersensitivity.
3- Induction of antibody immune response by B-cells.
4- Increase expression of T-cell derived cytokines, and this promotes
macrophage infiltration, allograft tissue damage.
5- CD8-positive T-cells mediate cell-mediated cytotoxicity reactions and
apoptosis leading to cytolysis of cells.
6-Activation of the natural killer (NK) cells is important in transplantation
because of their potent cytolytic activity.
Types of graft rejection:
1. Hyper acute: This occurs rapidly post transplantation. It may need
minutes to hours. The graft should be removed.
2. Acute rejection: This occurs after 10 – 30 days post transplantation. It is
mainly cell mediated.
3. Chronic or late rejection: This occurs slowly over a period of months or
years. It may be cell mediated or antibody mediated or both.
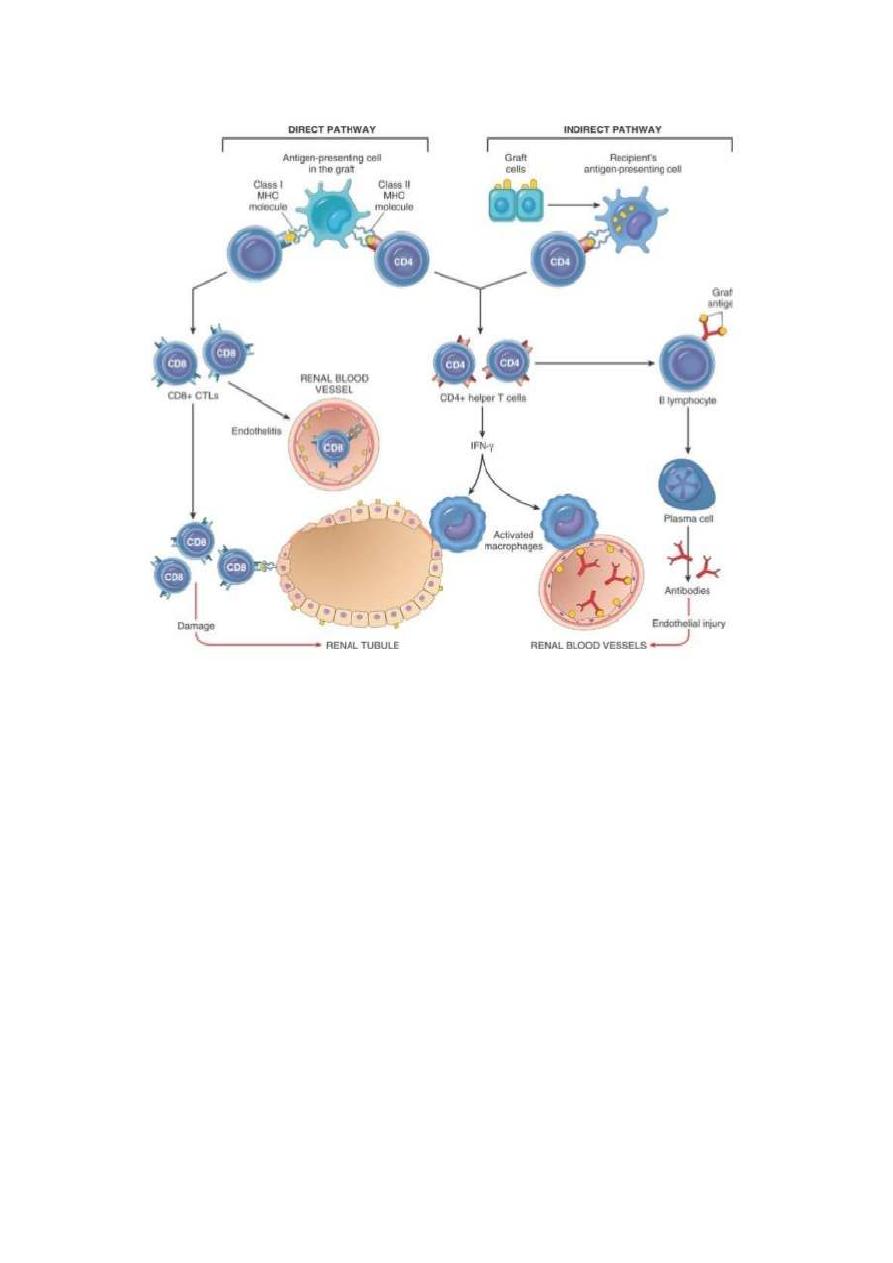
What is Graft Versus Host Disease ?
Graft Versus Host Disease (GvHD) is an immunological response
caused by mature donor T cells contaminating the Haetopoeitic stem cell
(HSC) inoculum, which recognize HLA differences expressed by host
antigen-presenting cells (APCs) and tissues.
Cytokines released from host cells after a patient chemotherapy or
radiotherapy conditioning create an inflammatory environment that
enables the generation of a response of infused donor T cells against host
antigens .
This initiates a cascade of T-cell activation events, which results in
proliferation, release of additional inflammatory cytokines, and the

generation of effector T cells that can infiltrate target tissue, particularly
the lymphoid system, intestinal tract, skin, and liver and mediate the
destruction of host cells in those organs.
Types of GVHD
1.
Acute Graft-Versus-Host Disease
It may occur as early as 1 week after HSCT and is potentially fatal.
Clinical manifestations of aGvHD are skin rash,diarrhea and liver
abnormalities.
2.
Chronic Graft-Versus-Host disease
symptoms that persist or appear after 100 days since the time of
transplantation. These clinical manifestations include
• hyperpigmentation, hyperkeratosis, skin atrophy, ulcerations), tissue
fibrosis
• fibrosis of exocrine glands
• fibrosis of lungs and liver.
• Its fatal
Treatment:
The GvHD is very serious condition. It has mortality up to 90%. The best
treatment is combination of Methotrexate + corticosteroids + Anti-sera.
Prevention of GvHD:
1. Anti-CD3 monoclonal antibodies to remove T cells from grafted tissue
as the bone marrow.
2. The blood or blood products should be irradiated prior giving to the
recipient.
3. Take all the measures necessary before transplantation to prevent GvHD
rather than treating it.
Graft Versus Host Disease (GvHD)
