College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
1
Hypersensitivity Reaction (HSR)
The main objectives of this lecture are:
Definition and classification of Hypersensitivity reaction (HSR).
The mechanism of type I HSR and anaphylaxis.
Diagnosis of Type I HSR.
The main points regarding treatment of Type I HSR.
The differences between anaphylaxis and the Anaphylactoid reaction
The term Hypersensitivity is a condition in which an immune response results in exaggerated or
inappropriate reactions that are harmful to the host. It
occurs in two steps:
o
First step is the First Exposure to the
antigen
which is known
Sensitization
.
o
Second step is Subsequent Exposure
( Re exposure to the antigen
)
Usually people have a genetic predisposition to react in an abnormal way to specific substances
which can produce HSR to their bodies. T helper cells are genetically more hypersensitive to
certain antigens.
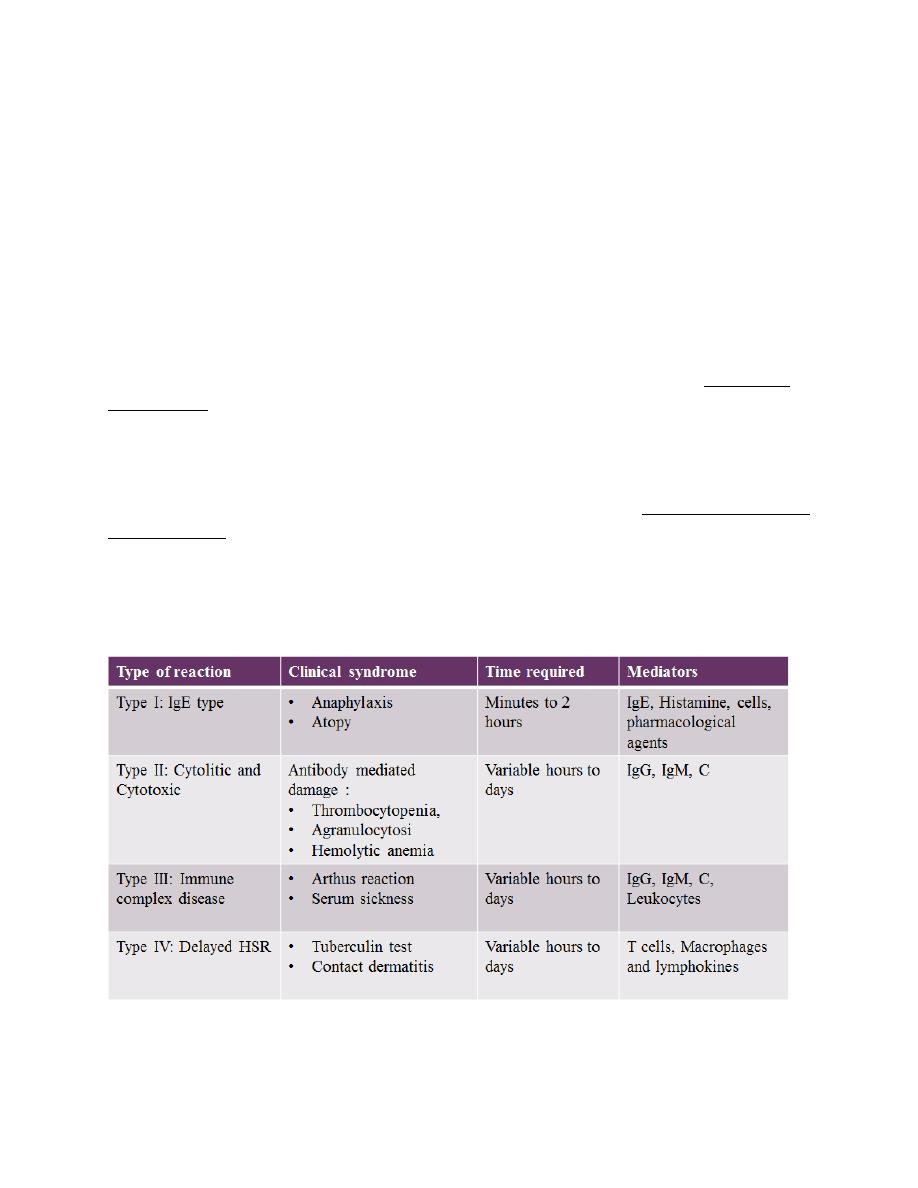
Classification: Gell & Coombs (1963):
College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
2
Note :
A particular disease may involve more than one type of HSR.
HSR occurs when an already sensitised individual is re-exposed to the same antigen.
Causes of tissue injury in HSR:
Release of vasoactive materials
Phagocytosis or lyses of cells
Activation of the complement system
Release of cytokines and cytolytic enzymes
TYPE I HSR:
The most common form of hypersensitivity is Gell and Coombs’ type I
It involves such everyday allergic conditions as hay fever, atopic eczema and urticaria in
addition to the rare and dangerous anaphylactic reactions to different materials as bee
stings, peanuts, penicillin, etc.
The underlying mechanism is a sudden degranulation of mast cells with the release of
inflammatory mediators, triggered by specific antibodies of the IgE class.
It is an example of acute inflammation induced by the presence of an
antigen
rather than
by injury or infection
Antigens that can trigger these reactions are known as ‘allergens’.
Allergens are often small molecular weight proteins (e.g. insect enzymes) or molecules
that bind to host proteins (e.g. penicillins).
People who suffer from allergy usually have raised levels of IgE in their blood and are
called ‘atopic’ that is usually inherited.
College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
3
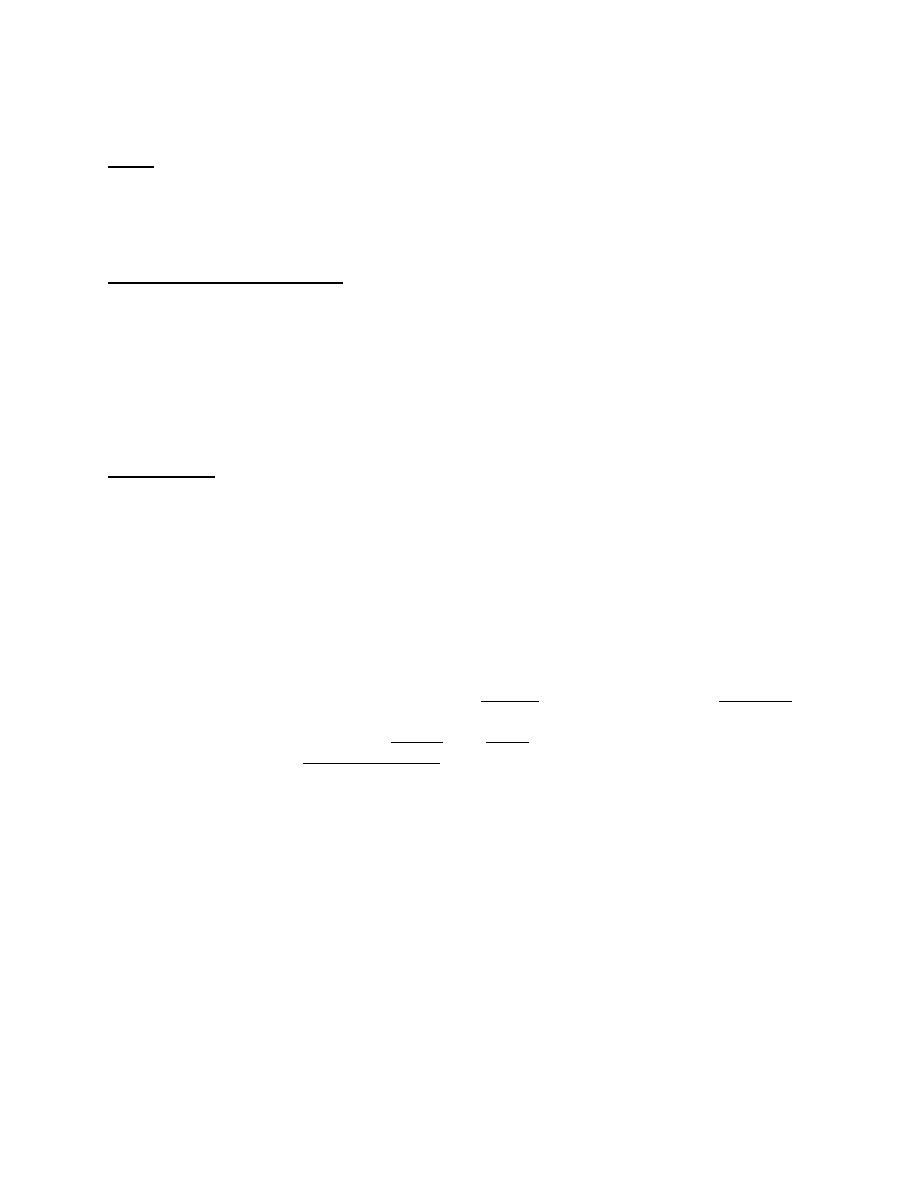
MECHANISM OF TYPE I HSR (1)
Requirements of type I hypersensitivity:
1- Allergens (antigens):
These allergens can be
Inhalants (house dust mites, pollens).
Ingestants (egg, fish, cheese, nuts).
Injectants (antibiotics).
Cotactants (wool, feather).
2-Cells:
Mast cells and basophils:
• They have Fc receptors for the reagenic IgE antibodies.
• Mast cells in the tissues and blood basophils are broadly similar, but there are differences
in the content of mediators.
• Mast cells are regulated by T lymphocytes via cytokine production as IL-4.

College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
4
Eosinophils
They have an important role in inflammation in the lung, which can lead to asthma.
They have important role in gut inflammatory diseases due to food allergies.
Similar to mast cells they release a variety of inflammatory mediators, and they are regulated by
T-cell-derived cytokines mainly IL-5.
They are prominent with PMN, in the ‘late phase’ reaction of allergic asthma that follows up
to 24 hours after the immediate response.
3. Reagenic IgE:
Is an anti-body, immunoglobulin (Ig) isotype E, and synthesized by plasma cells.
IgE has an essential role in Type I HSR and immunity to parasites.
IgE mediates allergic response by binding to FC receptors mainly found on the surface of
mast cells and basophils.
Fc receptors for IgE are also found on eosinophils, monocytes, macrophages and
platelets.
IgE antibodies interact with the allergens. This interaction leads to degranulation of the
bound mast cells and release of the variety of pre-formed, and newly formed, mediators
of inflammation and hypersensitivity.
IgE normally constitutes less than 1/10 000 of total Ig. Its level can rise up to 30 times
higher, and specific antibody levels 100 times higher, in allergic or worm-infested
patients.
In atopic patients, allergens induces more production of ‘Th2 type’ cytokines: IL-4, IL-5,
IL-13, etc., that up regulate IgE production, but very little of the Th1 cytokines such as
IFNγ which down regulate IgE production.
4. Mediators of allergy and anaphylaxis
Primary mediators
Pre-formed contents of Mast cells & Basophils:
•
Histamine
•
Serotonin
•
Eosinophils chemotactic factor of anaphylaxis (ECF-A)
•
Neutrophil chemotactic factor (NCF)
•
Heparin
•
Various proteolytic enzymes.
Secondary mediators
Newly formed after stimulation of mast cells, Basophils & other leucocytes:
•
Leukotriene as slow reacting substance of anaphylaxis (SRSA)
•
Prostaglandins
•
Platelet activating factors (PAF)

College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
5
Primary mediators:
Histamine
:
• Most important vaso-active amine of Human anaphylaxis, formed from histidine,
found in granules of mast cells.
• Released into skin, causes burning & itching.
• Causes vasodilatation & hyperemia by an axon reflex (Flare) and edema by
increasing capillary permeability (Weal).
• Induces smooth muscle contraction of different tissues & organs.
Serotonin (5-HT):
• Base derived by decarbolxylation of Tryptophan.
• Found in intestinal mucosa, brain & platelets.
• Causes smooth muscle contraction, ↑ vascular permeability.
Chemotactic factors such as:
•
ECF(eosinophils chemotactic factor):
Released from mast cell granules are strongly chemotactic for eosinophils. It accounts for high
eosinophil counts in many hypersensitivity reactions
•
NCF (neutrophils chemotactic factor): attracts neutrophils.
Enzymatic mediators
such as:
Proteases & hydrolases are also released from the mast cell granules.
•
Proteases as tryptase enzyme: increases mucus secretion, degradation of blood vessels
basement membrane.
Secondary mediators:
Prostaglandins and Leukotrine SRS-A
•
Derived from Arachidonic
•
They are broncho-constrictors, affect secretions of mucus glands, platelet
adhesion, permeability, and dilatation of capillaries.
Platelet activating factor – PAF
•
Low molecular wt lipid released from basophils
•
Causes aggregation of platelets and release of their vasoactive amines
Hives showing smooth, erythematous, and pruritic confluent papules and plaques (2).
College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
6
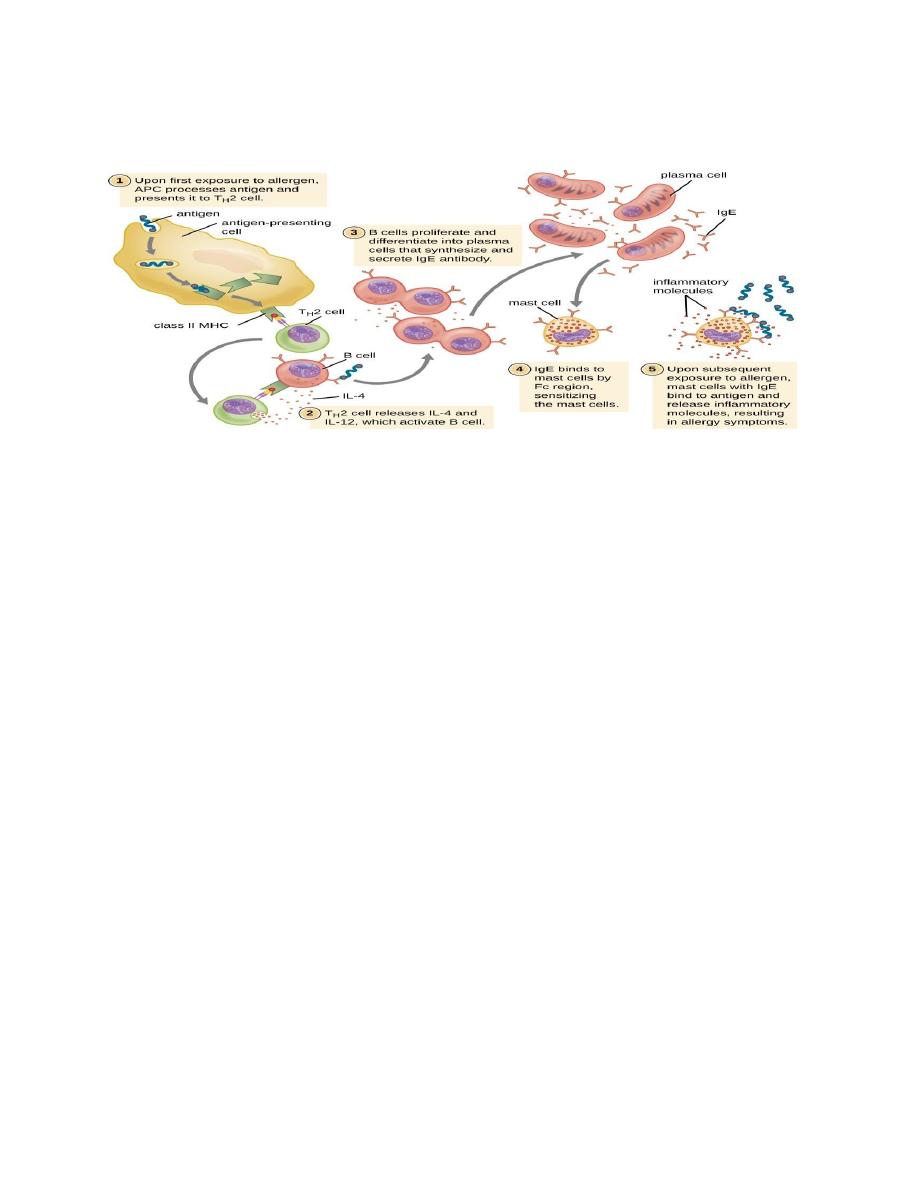
Anaphylaxis
Anaphylaxis is described as relatively rare life threatening immune IgE mediated, systemic
immediate type I hypersensitivity reaction, often occurring within seconds or minutes.
Anaphylaxis post insect sting (3)
Drugs well known for causing type I allergic reactions include:
Penicillins, cephalosporins, quinolones, chlorhexidine, neuromuscular blocking drugs,
some none steroidal anti-inflammatory drugs (NSAIDs), trimethoprim, sulfamethoxazole,
human–animal monoclonal antibodies used for therapy.

College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
7
NOTE:
It is uncommon to find a drug that has not provoked an anaphylactic reaction in at least one rare
individual.
Common foods causing allergy and anaphylaxis:
Nuts can cause severe and fatal allergies
Sea food
Milk, eggs and soy
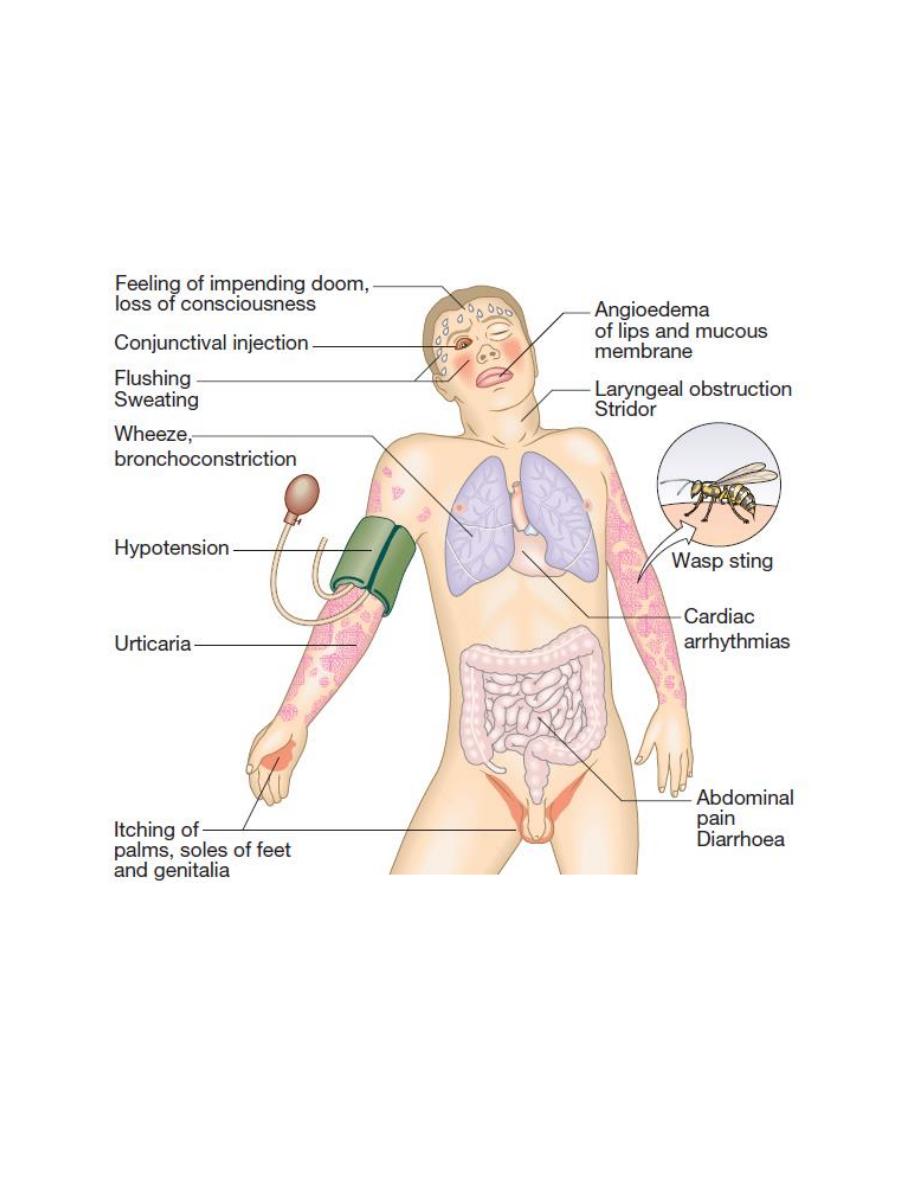
Diagnosis of type I HSR
Medical history
Skin prick testing
• It involves putting a drop of liquid onto the forearm that contains a substance; the patient
may be allergic to.
• The skin under the drop is then gently pricked with a needle. If the patient is allergic to
the substance, an itchy, red bump will appear within 15 minutes.
• The patient should not take antihistamine before the test, as they can interfere with the
results.

College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
8
Detection of total & specific IgE
Assessment of serum eosinophil cataionic protein (poor indicator in chronic asthma).
Skin prick test
Skin prick test (4)
Treatment
The treatment of an allergy depends on what the patient is allergic to.
1-Avoiding exposure to allergens
2- Allergy medications as:
(4)
College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
9
Sodium cromoglycate (DSCG; Intal) and steroids (e.g. betamethasone). They inhibit
mediators release by stabilizing cells lysosomal membranes.
Antihistamines
Adrenaline, isoprenaline, etc., which stimulate β receptors
Anticholinergics (e.g. atropine)
Theophylline, which raises cAMP levels.
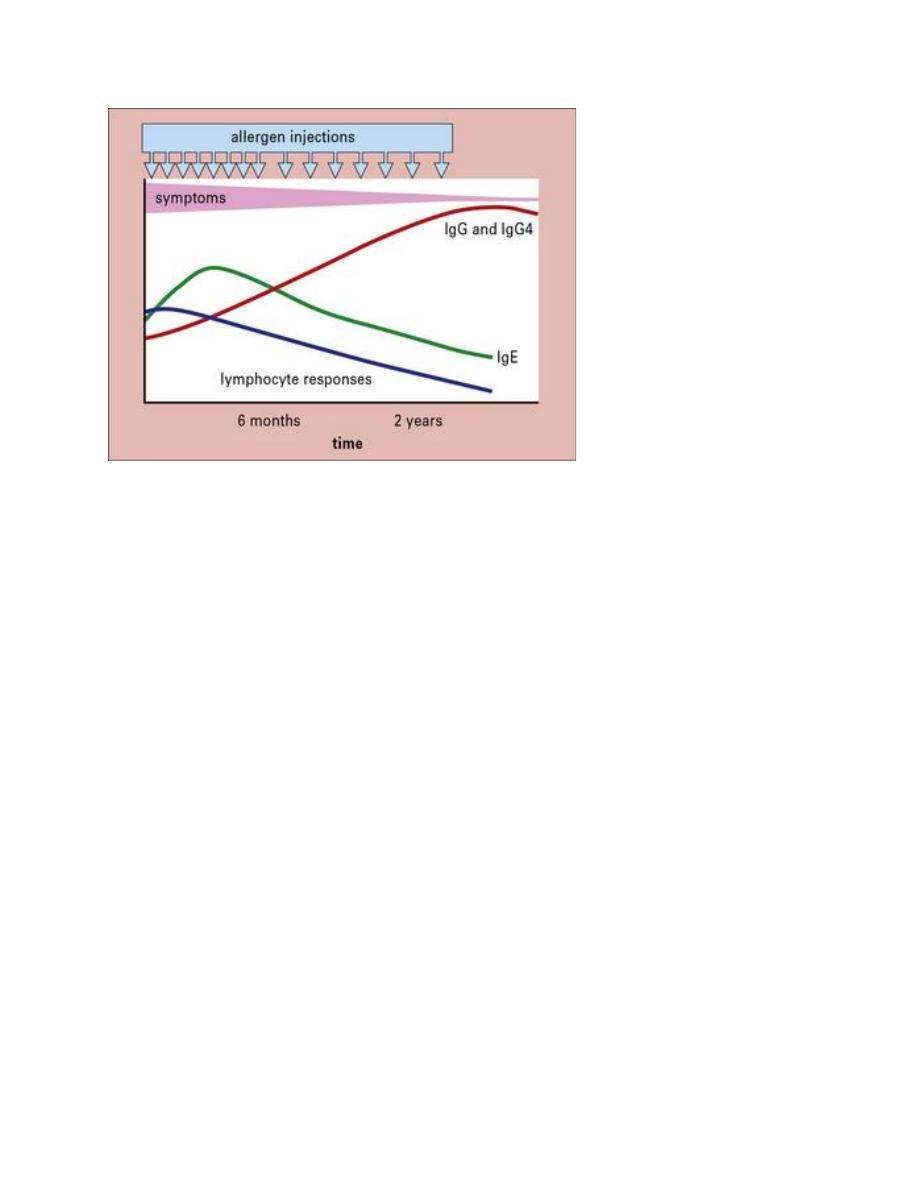
3-Immunotherapy (desensitization or hyposensitization):
It is specific therapy.
Allergic hyposensitization therapy will:
• Decrease the amount of IgE
• Stimulate the production of IgG4, the blocking antibody.
The blocking antibody combines with the allergen, but does not activate mast cells so
histamine is not released and symptoms are prevented.
Procedure:
Weekly injections of very small doses of the allergen for the first year, then gradually
decreased to monthly injections. The improvement is gradual and immediate results
should not be anticipated.
Hyposensitization is usually stopped after 4 years.
College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
10
Change of the amount of each isotype from more IgE to more IgG4 during hyposensetization. (5)
Anaphylactoid reactions:
Mimic signs and symptoms of anaphylaxis,
Are caused by non-IgE mediated release of potent mediators from mast cells and
basophils.
Anaphylactoid reactions occur at the first contact.
This reaction can be caused by:
• Vigorous exercise
• Contrast media that contains radiographic iodine
• Dextran
• Morphine, codeine
• Polymyxin B antibiotic
• NSAIDs
• Idiopathic in 20%

College of Medicine University of Mosul /Department of: Immunology
Subject: Microbiology-Immunology Stage: 3
rd
2021-2022
Lecturer Dr. Ahmed Al harbi Date: 8/12/2021 No.1
Pag
e
11
Summary
HSR is inappropriate immune reaction toward Ag
HSR usually needs more than one exposure to the same Ag
There are 4 types of HSR
Type I HSR is mediated by IgE Ab, cells and pharmacological mediators
Allergens, cells, IgE Abs and mediators are required in type I HSR
Skin prick, detection of IgE and eosinophil study are helpful in Dx of allergy
Avoidance is the best method for prevention of allergy, however medications and
immunotherapy can be used
Anaphylactoid has similar symptoms to anaphylaxis with different aetiology.
References:
1. Lumen learning.com /Immunology
2. NHS.uk
3. Owen J, Punt J, Stanford S and Jones P. Kuby immunology. New York. Macmillan
higher education. 2016
4. Aashwas.in
5. https://clinicalgate.com/immediate-hypersensitivity-type-i/
6. Davidson’s principles and practice of medicine 23
rd
edition.
